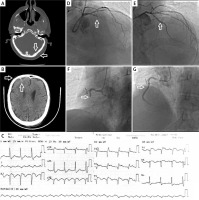
A 60-year-old male patient was admitted to the emergency department following a road traffic accident and head trauma. A fracture in the occipital bone and a subarachnoid hemorrhage (SAH) in the right frontal region were detected on computed tomography (CT) (Figures 1 A, B). On arrival, an electrocardiogram (ECG) showed sinus rhythm with no ischemic findings. Physical examination results were unremarkable, except for ecchymosis on the anterior and posterior surfaces of the head and no evidence of blunt trauma to the thorax. During the follow-up in the emergency department, the patient experienced severe chest pain. The follow-up ECG revealed acute ST-segment elevation in the V2-6 leads (Figure 1 C). Urgent surgical intervention was not considered in neurosurgical consultations. Instead, serial CT follow-up was recommended and anticoagulant and antiplatelet therapies were initiated in a controlled manner. After a loading dose of 100 mg of oral acetylsalicylic acid, 300 mg of clopidogrel, and intravenous unfractionated heparin at 80 U/kg, emergency coronary angiography revealed thrombotic total occlusion in the proximal part of the left anterior descending artery (LAD) and right coronary artery (RCA) (Figures 1 D, E). The LAD and RCA lesions were crossed using a floppy guidewire. Both lesions had a high thrombus burden. Thrombus aspiration was performed using an aspiration thrombectomy device and control images showed dissected plaques causing partial narrowing of both coronary arteries. Subsequently, zotarolimus-eluting stents were implanted directly into the LAD lesion (3.0 × 15 mm) and RCA lesion (3.5 × 18 mm) without pre-dilation (Figures 1 F, G). TIMI grade 3 flow was achieved in the LAD and RCA, and the patient was transferred to the coronary intensive care unit. The total ischemic time was 26 min. SAH was self-limiting, and no increase was detected on brain CT scans taken during in-hospital follow-up. The patient was discharged after 7 days on dual anti-aggregant therapy with acetylsalicylic acid (81 mg) and clopidogrel (75 mg).
Figure 1
A – Fracture in the occipital region (with arrow), B – SAH in the right frontal region (with arrow), C – acute anterior myocardial infarction in ECG, D – LAD total occlusion (with arrow), E – LAD image after successful PCI procedure (with arrow), F – RCA total occlusion (with arrow), G – RCA image after successful PCI procedure (with arrow)
Concurrent acute myocardial infarction (AMI) and SAH are rarely reported, remain challenging to manage [1, 2], and are associated with increased in-hospital mortality, prolonged in-hospital stay, and poor functional status [3]. It is difficult to decide whether one should be treated first, and the immediate treatment of one of these conditions may worsen the other. In selected cases with low risk of bleeding, dual antiplatelet therapy may be appropriate with close clinical monitoring and supervision by the surgical team. Herein, we report a case of multiple coronary artery occlusions due to trauma and SAH, suggesting increased hypercoagulability. It should be noted that increased emotional stress and catecholamine release can lead to various overlooked clinical consequences. To our knowledge, this is the first report of multiple coronary occlusions following a SAH. More data are needed to determine the most appropriate treatment for bleeding and thrombosis in these patients.








