Global estimates suggest that there are approximately 25 million transgender individuals worldwide, with about one million residing in the United States. The increasing accessibility of plastic surgery and more inclusive insurance policies have led to a rise in the number of transgender individuals opting for surgical treatments. According to 2019 research, about 28% of transgender women have undergone gender-affirming surgical procedures, with 5–13% of these surgeries involving genital reconstruction. Among transgender women who have not had gender-affirming surgery, approximately 45–54% express a desire to have such procedures in the future [1]. Often, these treatments significantly alleviate gender dysphoria, which is the distress caused by a discrepancy between a person’s experienced or expressed gender and their assigned sex at birth, thereby enhancing their quality of life. The scarcity of precise epidemiological data on gender dysphoria is probably a result of ongoing social stigma [2].
A 39-year-old transgender patient was admitted to the gastroenterology department in July 2023 with progressive weakness, weight loss (approximately 8 kg in 2 months), severe abdominal pain primarily during defecation, diarrhoea with blood (including nocturnal episodes), and vaginal bleeding. The patient had undergone surgical gender reassignment on 11 November 2021. The surgery involved the removal of external genital organs, formation of labia, creation of an external urethral opening, and separation of the sigmoid and neovaginal sections. The patient was receiving hormonal treatment under an endocrinologist’s care. Prior to the 2021 surgery, a colonoscopy had indicated normal mucosal condition. The patient also had a history of vitiligo and bronchial asthma, was married with children, and is currently in a civil partnership with a woman. In May 2023, the patient experienced loose bowel movements with blood and vaginal bleeding for the first time, accompanied by laboratory findings of thrombocythaemia (535 thousand; normal range: 150–400 thousand), peripheral eosinophilia (13.8%; N < 7), elevated IgE level (754 IU/ml; N < 100), and increased stool calprotectin level (261 µg/g). Stool cultures for pathogenic bacteria and parasites were negative. Transglutaminase antibodies were within normal limits. Due to neovaginal bleeding, the patient was also referred to a gynaecologist, who found no pathological changes.
Upon admission, the patient was diagnosed with normocytic anaemia (Hb 8.9 mg%), thrombocythaemia (611,000), low iron (Fe 16 µg/dl; N 37–145) and ferritin levels (8 ng/ml), elevated C-reactive proin (CRP) (15.7 mg/l; N < 5.0), and decreased protein (44 g/l; N 64–83) and albumin levels (22 g/l; N 35–52). Stool calprotectin was markedly elevated (1200 µg/g). Other tests, including lipid profile, stool cultures, and screenings for hepatitis and HIV, were negative. Due to the clinical picture and previous history of inflammatory bowel disease (IBD), endoscopic examinations were performed, obtaining the following results:
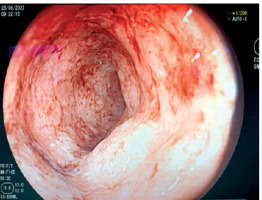
During the colonoscopic examination, inflammatory changes were observed covering the mucous membrane of the entire large intestine. The endoscopic assessment of the severity of lesions was classified as Mayo 3. Histopathological examination confirmed the presence of ulcerative colitis (UC) lesions (Figure 1).
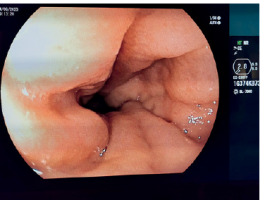
During the endoscopic examination, the mucosa of the neovagina was assessed. The neovagina was prepared from a fragment of the sigmoid colon, in accordance with the operating protocol. The severity of inflammatory changes was confirmed as Mayo 3 (Figure 2), a finding that was corroborated by histopathological examination, indicating inflammatory changes in the course of UC.
Gastrofibroscopy revealed changes characteristic of erosive gastropathy.
Additionally, computed tomography (CT) enterography was performed, revealing inflammatory changes mainly in the transverse colon and the left half of the intestine, as well as in the neovagina.
Treatment included steroid therapy, oral mesalazine, local treatment with suppositories, butyric acid, and nutritional therapy with enteral and intravenous iron supplementation. The patient’s condition improved, with reduced bowel movements and cessation of neovaginal bleeding. After 2 months, the patient reported good well-being, with improved lab results and reduced inflammation in endoscopic evaluations (Mayo 1) (Figures 3, 4). The patient remains under our Gastroenterology Centre’s supervision.
Transgender individuals, whose gender identity differs from their assigned sex at birth, often begin gender affirmation with hormone therapy. This therapy aims to develop secondary sexual characteristics aligning with their gender identity. Established hormonal therapy protocols for feminisation (oestrogens and anti-androgens) and masculinisation (testosterone) are generally safe and improve mental health outcomes, including depression, anxiety, and gender dysphoria [3]. However, they can also lead to medical issues like weight changes and chronic disease risks [4].
The next stage of gender affirmation, after hormonal treatment, is transgender surgery. For transgender women, this involves removing the corpus cavernosum, shortening the urethra, and performing gender-affirming valvuloplasty to create a neovagina, often using skin from the penis and segments of the large intestine or peritoneum [5–9]. Indications for gender reassignment surgery include documented gender nonconformity, informed consent, understanding of reproductive impacts, legal adulthood, a minimum of 6 months of hormone therapy, and evaluations by mental health professionals. Contraindications include severe comorbidities, smoking, and, for vaginoplasty, a body mass index (BMI) > 30 kg/m2. Specific contraindications for intestinal vaginoplasty include extensive abdominal surgery, ulcerative colitis, and colorectal cancer. These surgeries, often performed laparoscopically or robotically, have complication rates comparable to other elective colorectal surgeries. Complications can include segmental necrosis, anastomotic leak, intestinal obstruction, rectovaginal fistula, stenosis, and in the case of neovagina formation, inflammation of the intestinal mucosa, pain, bleeding, or unpleasant vaginal odour. Treatment may involve short-chain fatty acids and/or locally acting anti-inflammatory agents. Endoscopic surveillance is recommended every 5 years due to the chronic inflammation and increased colorectal cancer risk [10–14]. Despite potential complications, most transgender individuals report satisfaction with the results of genital surgery in terms of quality of life and sexual health. The growing transgender population highlights the need for better training and understanding among healthcare providers to meet their healthcare needs effectively.
It is worth emphasising that research shows that individuals who identify as transgender tend to have lower levels of college education and are less likely to identify as heterosexual compared to those who do not identify as transgender. When accounting for these and other characteristics, it is observed that transgender individuals generally experience lower employment rates, reduced household incomes, higher rates of poverty, and poorer self-rated mental and physical health in comparison to their cisgender counterparts [15, 16]. Historically, individuals with gender minority identities have faced significant challenges in accessing healthcare. Experiences of discrimination and transphobia can hinder effective communication, adversely impact the quality of care, and result in poorer health outcomes [17, 18]. Hence, it is even more crucial to develop guidelines and recommendations for this group of patients to ensure not only the provision of effective medical treatment but also the understanding of their individual needs. Although there have been attempts to create some guidelines devoted to transgender patients with IBD [19, 20], to the best of our knowledge, a case as specific as the one we describe has not yet been documented in scientific publications.
We can state with a high degree of confidence that the number of transgender individuals encountered and treated by healthcare professionals will continue to grow. In addition to complications related to surgical procedures, it is important to consider coexisting chronic diseases, such as ulcerative colitis or Crohn’s disease, as potential causes of symptoms. These symptoms may include bleeding, not only from the anus but also from the neovagina in transgender patients.