Coronavirus disease 2019 (COVID-19), or also called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, has caused global pandemic [1]. Atopic dermatitis (AD) is a chronic, inflammatory skin disease, characterized by eczematous lesions and continuous pruritus. The pathophysiology of AD is complex, and immunity plays a key role [2]. Also, COVID-19 could be related to the immunological factors [3]. Currently, the relationship between the risk of COVID-19 and AD is controversial. Differences were demonstrated among the studies. Therefore, there is a need to analyse the association more comprehensively. In this study, we evaluated the risk of COVID-19 in AD patients through meta-analysis and trial sequential analysis.
Seven databases were searched to select eligible publications. For the included studies, quality was assessed through Newcastle-Ottawa Scale. A study can be considered as high-quality with score ≥ 6 (9 in total). The odds ratio (OR) was used to evaluate the association. Details are in supplementary materials (Supplementary Tables S1, S2, Supplememtary Figure S1). In the analysis procedure, according to the between-study heterogeneity, a fixed or random effect model was selected. Trial sequential analysis (TSA) was performed through TSA software based on Java. TSA is used to evaluate if the case number in each comparison is sufficient. In our study, the 5% risk of type I error (false positive) and 30% risk of type II error (false negative) was set.
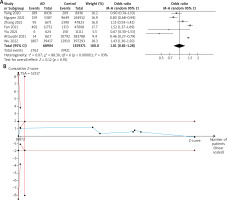
Seven studies were included [4–10]. Frequencies of COVID 19 in AD patients varied from 0.87% to 4.58%. In control subjects, the value varied from 1.42% to 5.00%. Details are in Table 1. Due to the significance of heterogeneity, the random effect model was applied. The merged data suggested that the AD patients did not have an elevated risk of COVID-19 (OR = 1.01, 95% CI: 0.81–1.28, p > 0.05). In TSA, the Z-curve crossed the required information line which indicated that a total of 52.137 cases need be included. Our study included 1.428.275 in total (Figure 1). The TSA result suggested that the case number is sufficient to draw a reliable conclusion. The funnel plot demonstrated asymmetry, indicating the publication bias may exist (Supplementary Figure S2). From sensitivity analysis, the result of meta-analysis was robust, because when each study was ignored, the total effect did not show significance. Subgroup analysis by location was then performed. Also, no significance was shown in each subgroup, which was similar with the total effect (Supplementary Figure S3).
Table 1
Characteristics of included studies
Our study found that the risk of COVID-19 is similar for AD patients and control subjects. Multiple cytokines, such as interleukin-13, participated in the pathogenesis of AD. Also, those cytokines can increase transmembrane protease serine 2 and decrease angiotensin-converting enzyme 2 expression, regulate the entry of SARS-CoV-2 into airway epithelial cells, thus reduce the infection risk [11].
AD patients have more medical needs, but during the pandemic, the long-term follow-up can be solved by teledermatology, which is useful to reduce access to hospital and well accepted by patients [12], so it will not lead to a significant increase in the infection rate. Besides, AD is associated with psychological disorder including depression, anxiety, and autism [13]. Therefore, AD patients might reduce their social interaction and change living habits due to illness. They might less participate in gathering activities and have better hygiene habits such as timely hand hygiene, which also contributes to reduce the infection risk.
There was a limitation that the impact of AD on the severity of COVID-19 was not analysed, because the definitions of severity were varied, which made the analysis of related factors more complex.
In conclusion, the risk of COVID-19 is not elevated in AD patients. However, for AD patients, it is still necessary to pay attention to the prevention in daily life and choose teledermatology appropriately during follow-up visits.