Introduction
Type 1 diabetes mellitus is characterized by autoimmune destruction of beta cells in the pancreas, resulting in insufficient insulin production and the appearance of hyperglycemia [1]. It is one of the most common chronic diseases occurring in children in Poland. Observing the trends in the incidence of the disease in the group of the youngest children in 2025 it is predicted that almost fourfold increase in the incidence [2]. Currently, 5–10% of diabetes patients are teenagers [3]. During this period, the influence of peers and observation of their eating habits plays a significant role [4]. Unfortunately, they very often differ from the principles of proper nutrition, which, according to the PTD Diabetes Poland, should be introduced as an element influencing the proper metabolic balance of patients with type 1 diabetes [5]. According to the adopted standards, carbohydrates should cover 45–50% of the daily energy demand, and the simple sugars contained in it should not exceed 10%. In a balanced diet, protein should cover 15 to 20% of the daily calorie intake and fats 30–35% [6]. Recent publications also emphasize the beneficial effect of a carbohydrate-reduced diet on correct metabolic balance [7]. However, it has not yet been verified how such a diet will affect the physical and mental development of children and adolescents [8].
In addition to the strict principles, the National Food and Nutrition Institute in Warsaw provides knowledge on healthy eating by means of the pyramid of healthy nutrition and lifestyle of children and adolescents. It uses a graphic representation of how often and in what quantity a given group of products should be included in a properly balanced diet [9]. In addition, for adolescents suffering from type 1 diabetes, a diet with a low glycemic index (GI < 55) improves glycemic control [10]. Currently, there are numerous publications indicating the beneficial effect of various diets on the proper metabolic control in type 1 diabetic patients and their health status. One of them is the Mediterranean diet, which has been proven to have a beneficial effect on the physical and mental well-being of children with type 1 diabetes [11].
The aim of this study was to assess the condition and dietary habits of male adolescents with type 1 diabetes and to compare their eating habits to generally accepted standards of proper nutrition. It was assumed that the previously conducted nutritional education, knowledge of the basic principles of proper nutrition will affect the nutritional habits of patients. In addition, it was concluded that the majority of patients will follow the dietary recommendations to maintain proper metabolic balance and prevent the occurrence of complications.
Material and methods
Characteristics of the test group
The study group consisted of 20 boys with type 1 diabetes, who were diagnosed using ISPAD criteria [12]. The examined teenagers remain under the care of the Department of Pediatrics, Endocrinology and Diabetology of the Medical University of Gdansk. On this basis the body mass index (BMI) was calculated, which was 20.4 ±2.7 kg/m2. BMI in pediatric population should be interpreted using percentiles score according with sex and age. In the study group, 7 patients were found to be underweight and none of the qualified individuals were overweight or obese. The mean age of patients was 14.6 ±1.58 years. The body weight of the studied group was 59.4 ±15.0 kg and the average height was 170.5 ±9.2 cm.
Before the test, each patient was presented with a physical effort protocol and all participants signed an informed consent to the examination. Furthermore, the consent to the study was obtained from the Bioethics Committee of the Medical University of Gdansk. Each patient was treated with a personal insulin pump from Medtronic Paradigm Veo or MiniMed 640G. An additional criterion for inclusion in the study group was Tanner II, IV or V sex maturity; balanced physical activity, no ketoacidosis incidents and infrequent occurrence of hypoglycemia in the last five years.
In the study group, the average duration of the disease was 7.4 ±4.3 years and the average duration of pump therapy was 6.8 ±4.1 years. The average value of HbA1c was 7.55 ±0.84%. The exclusion criteria included obesity, other chronic diseases that could affect the occurrence of hypoglycemia and the patient’s lack of consent to participate in the study. The general characteristics of the study group are presented in Table I.
Assessment of nutritional status
In each participant the nutritional status was assessed using anthropometric methods (height, body weight). Based on the results obtained, the body mass index (BMI) was calculated using the following formula: Body mass ratio (kg) to height per square (m2) [13]. Additionally, the WHR (waist – hip) indicator was used, whose formula is the ratio of waist to hip circumference [14]. Its interpretation indicates the distribution of body fat [15]. The body composition was then analyzed by using the InBody 770.
Assessment of the diet
During the examination, a thorough nutritional history was conducted; with each boy a nutritional interviews was performed and a 7-day dietary diary was recommended. On the basis of the information received, the dietary habits of patients with type 1 diabetes were evaluated. Additionally, a dietary analysis was performed on the basis of the test of Starzynska [16].
Results
Body composition analysis
The following results were obtained from the body analysis composition performed by using the InBody 770 device. The average content of adipose tissue was 14.72 ±6.25%, which is 8.71 ±4.10 kg per kg. 60% of the examined patients showed a normal body fat content despite the lack of regular physical activity. The average content of skeletal muscles in the examined group was 28.2 ±6.93 kg, which in half of the adolescents indicated normal body fat content. An additional parameter obtained by using this method was the total body water content, whose average in the examined group was 38.05 ±8.42 L. More than a half of the examined adolescents were properly hydrated for the reason that this parameter correlates with the content of skeletal muscles in the body. On account of the results obtained, the WHR index was calculated, whose average value in the examined group was 0.796 ±0.034, this result does not indicate the occurrence of abdominal obesity in the examined adolescents. The obtained results are presented in Table II.
Analysis of dietary regime
On the basis of the analysis of the patients’ diet, the energy demand is covered by three quarters of the study group. According to the accepted standards regarding the macronutrients, less than 45% of adolescents cover the recommended daily amount of carbohydrates. The very high consumption of monosaccharides is alarming, as almost all subjects (95%, n = 19) consumed more than the accepted recommendations of the PTD Diabetes Poland. Additionally, 45% of the respondents did not cover their daily dietary fiber requirements. The research results also indicated that the consumption of the remaining macronutrients, including protein and fat, was not satisfactory. The above-mentioned parameters are presented in Table III.
Table III
Analysis of nutrition
Dietary habits and meal quality of adolescents with type 1 diabetes were analyzed on the basis of dietary diaries and the test of Starzynska. The majority of the study subjects have very similar nutritional errors, which include: lack of regularity of consumed meals; low consumption of vegetables and fruits; low consumption of whole-grain products; excess consumption of animal products; low consumption of fish, nuts, grains and seeds; occurrence of numerous unhealthy snacks such as sweets, chips; frequent consumption of sweet drinks; inappropriate portions of meals that are too large; choice of inappropriate technological treatment such as deep-frying.
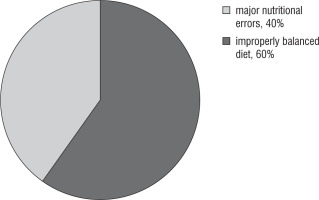
To evaluate the diet and interpretation of the received menus a test according to Starzynska was applied. By mean of the conducted test it was found that 60% of the subjects had dietary mistakes such as: lack of proper meals, low consumption of lean dairy products, lack of fruits and vegetables as well as lack of groats and dry seeds of legumes. The test results are presented in Figure 1.
Discussion
Numerous publications emphasize the importance of proper nutrition in the process of glycemic control and preventing metabolic complications in the future. The most recent reports from 2019 confirm that the introduction of the principles of rational nutrition together with the recommendations of the Mediterranean diet ensure the maintenance of proper glycemia [17]. The American Diabetes Association also stresses the importance of a properly balanced diet with a reduction in monosaccharides and saturated fatty acids to reduce the need for insulin and maintain normoglycemia [18].
Unfortunately, improper nutrition is very common in adolescents with type 1 diabetes. A study by Race Mackey et al. published in 2018 shows that a diet rich in fats and increased energy intake in relation to daily demand has a negative impact on the metabolic control of diabetes [19].
Another study published by Gilbertson et al. and Delahanty emphasizes how improper nutrition, including excessive intake of monosaccharides, saturated fatty acid fat and protein, increases the risk of overweight and obesity in children with type 1 diabetes [20]. Moreover, the studies by Delahanta et al. have proven that high concentrations of saturated and unsaturated fatty acids consumed in the diet closely interfere with higher values of glycated hemoglobin in children. The analysis of the conducted studies showed that the method of intensive functional insulin therapy with a personal insulin pump may result in reduced dietary restriction in adolescents leading to overweight development and worse metabolic balance of the disease. The study proved that adolescents with type 1 diabetes had regular snacks and skipped the main meals. The research carried out by Kleinowska et al. proved that younger children with type 1 diabetes followed a more balanced dietary regime compared to teenagers between 13 and 18 years of age. The author emphasized that the adolescent age favors the development of abnormal eating habits, which is a consequence of improperly balanced diabetes [21].
In the studies by Mehta et al. a special role was attached to the level of knowledge of patients with type 1 diabetes. The authors emphasized that adolescents with type 1 diabetes misinterpret products called healthy. The main problem of this group of patients was a mistaken perception of the limitations of carbohydrate intake. Unfortunately, they were replaced by excessive consumption of protein and fat products. The authors paid special attention to the fact that an excessive fat supply does not cause an increase in postprandial glycemia levels, however contributes to overweight, insulin resistance and lipid metabolism disorders [22].
The studies by Joanna Sadowska and Katarzyna Kaldonska pay particular attention to the insufficient intake of minerals and vitamins by teenagers in their diet, which are necessary for proper growth and development. Scientific research presented by the above mentioned authors proved that the lack or low content of water-soluble vitamins in the diet contributes to disorders of carbohydrate metabolism and the formation of skin lesions. In their analysis, the authors have proven that various dietary deficiencies, despite a properly balanced diet, may be the cause of increased diabetes symptoms and numerous accompanying changes [23].
Subsequent studies of Gilbertson’s syndrome in a group of Australian teenagers with type 1 diabetes also confirm that consumption of too much monosaccharides affects higher lipid levels, increased BMI and HbA1c [24].
The results of the above mentioned publications demonstrate similar conclusions to the assumptions presented in this publication. The main nutritional mistakes of patients with type 1 diabetes are the excess of monosaccharides from sweets and sugary drinks, too high energy density of food due to the improper technological processing for meal preparation or choosing highly processed food.
However, it should be stressed that there is also a group of patients who are struggling with nutritional problems called diabulimia [25]. It has been observed that often too much focus on a restrictive diet and maintaining proper body weight, especially in a group of teenagers, can lead to nutritional disorders [26].
On the other hand, there is no difference in dietary habits between healthy male adolescent and teenager with type 1 diabetes. In both groups, eating habits need to be changed. Identical nutritional mistakes are observed, such as: lack of breakfast, deficiency of lean dairy products, vegetables and fruit, whole grains or fish consumption. Instead, there is an excess of highly processed food. Unfortunately, peers and the mass media has the greatest influence on the occurrence of bad eating habits [27].
Conclusions
In conclusion, despite frequent nutritional education regarding the beneficial effect of proper nutrition on glycemic control and prevention of diabetic complications, the nutritional habits of male adolescents differ from those of proper nutrition. Additionally, it should be noted that despite the proper results of the body composition analysis, it has been observed that even in those patients the problem with an erroneously balanced diet, long breaks between meals and lack of regular physical activity adversely affect the metabolic balance.

 ENGLISH
ENGLISH