Summary
Operator-patient sex discordance may impact the outcomes of surgical procedures; however, no such impact was confirmed for percutaneous coronary interventions in our study. Women were underrepresented as interventional cardiologists. Efforts are needed to provide women with equitable opportunities.
Introduction
Cardiovascular disease is a leading cause of morbidity and mortality in women and men, although there are substantial gender disparities in presentation and outcome [1–3]. Importantly, female gender is associated with worse results of percutaneous coronary intervention (PCI) performed in different clinical scenarios [2], from stable angina [4], through acute coronary syndromes [5–8], to cardiogenic shock [9]. These may be related to more advanced age and higher prevalence of comorbidities at presentation in women as compared to men [1]. In addition, some differences in the vascular ageing process [10] and atherosclerotic plaque composition [3] between women and men were confirmed. On the other hand, women are more likely than men to be subject to health disparities [1]. These disparities may arise from sociocultural and socioeconomic factors and may result in less optimal cardiovascular disease care. For instance, one aspect of this issue is the presence of sex or gender discordance between patients and physicians, especially among male physicians and female patients [1]. Such discordance was associated with increased mortality among female patients treated by male physicians after acute myocardial infarction (AMI) [11]. In contrast, no excess in mortality was observed for male patients treated by female physicians. Interestingly, a recent study suggested that sex discordance between surgeons and patients negatively affects outcomes of patients undergoing common surgical procedures [12]. Whether such a relationship exists for patients undergoing less invasive procedures is less well established.
Aim
We sought to assess the impact of operator-patient sex discordance on periprocedural outcomes of PCI using data from the Polish National Registry of PCI (ORPKI).
Material and methods
The ORPKI is a national registry conducted by the Jagiellonian University Medical College in Krakow collecting data on all percutaneous procedures in interventional cardiology performed in Poland [13–16]. Data were collected from January 2014 to December 2020 in 154 invasive cardiology centers. Data on 581,744 consecutive patients undergoing single-stage coronary angiography and PCI were retrieved from the database for this analysis. Patients were divided into four groups based on the patient and operator sex. Operator-patient sex discordance was defined as the procedure done by a male operator in a female patient or by a female operator in a male patient. All angiographies and PCIs were carried out according to contemporary medical standards. The decision on concomitant pharmacotherapy and procedural technique was the operator’s choice. The primary endpoint was all-cause periprocedural (in the catheterization laboratory) mortality. In addition, data on other periprocedural complications, including stroke, cardiac arrest, coronary artery perforation, no-reflow, allergic reaction, and puncture site bleeding, were collected. The assessment of complications and grading of epicardial flow with Thrombolysis in Myocardial Infarction (TIMI) scale before and after PCI were based on the operator’s judgment. Also, occurrence of bleeding was self-reported by the operators, particularly in the case of any overt, actionable sign of puncture sign bleeding. The mean number of PCIs performed per site and operator was the mean for a seven-year study period.
Statistical analysis
Continuous variables are presented as means with standard deviations and were compared across groups using Student’s t test. Categorical variables were compared with Pearson’s χ2 or Fisher’s exact test if 20% of cells had an expected count of less than 5 (Monte Carlo simulation for Fisher’s test using tables of higher dimensions than 2x2). Multivariable models were constructed with adjustment for all clinically important and meaningful baseline and procedural characteristics. Periprocedural outcomes associated with the presence versus absence of operator-patient discordance by patient sex are presented as odds ratios (OR) with two-sided 95% confidence intervals (CI). P-values < 0.05 were assumed to indicate statistical significance. Statistical analysis was performed in STATA 17.0 (StataCorp LLC, 2021).
Results
Between 2014 and 2020, data on 581,744 patients undergoing single-stage coronary angiography and PCI were collected in the ORPKI Registry. During the study period, procedures were carried out by 34 female and 782 male operators. Of 581,744 patients, 194,691 patients were sex discordant with their operator (12,479 female operator with male patient and 182,212 male operator with female patient) while 387,053 were sex concordant (female operator with female patient 6,068; male operator with male patient 380,985). Study groups differed in most baseline characteristics (Table I) as well as procedural details and pharmacotherapy (Table II).
Table I
Baseline characteristics
Table II
Procedural details and pharmacotherapy
[i] Values are presented as percentages or mean (±standard deviation). CTO – chronic total occlusion, FFR – fractional flow reserve, GP – glycoprotein, IVUS – intravascular ultrasound, LAD – left anterior descending artery, LMCA – left main coronary artery, OCT – optical coherence tomography, PCI – percutaneous coronary intervention, TIMI – Thrombolysis in Myocardial Infarction.
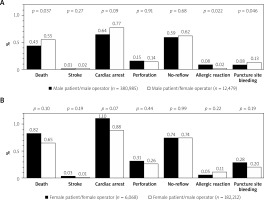
Among female patients no difference in the risk of the composite of periprocedural complications between patients discordant versus concordant with operators was noted (2.70% vs. 3.02%; p = 0.14). In addition, there were no differences in the individual components of periprocedural outcomes (Figure 1 A, Table III). Similarly, among male patients no difference in the risk of the composite of periprocedural complications (1.92% vs. 1.87%; p = 0.69) between discordant and concordant patients was observed. The risk of death (0.55% vs. 0.43%; p = 0.037) and bleeding at the puncture site (0.13% vs. 0.08%; p = 0.046) was higher in male patients discordant versus concordant with operators (Figure 1 B). Conversely, the latter were at lower risk of allergic reactions (0.02% vs. 0.08%; p = 0.022). However, all the differences in outcomes between male patients discordant versus concordant with operators were no longer significant after adjustment for covariates, except for allergic reactions, which were fewer in male patients discordant versus concordant with the operator (Table III).
Table III
Associations between operator-patient sex discordance and periprocedural outcomes
Discussion
Our main findings are that women constitute around 4% of all PCI operators in Poland and were responsible for around 3.2% of all PCIs between 2014 and 2020. Importantly, no association between operator-patient sex discordance and periprocedural outcomes was confirmed regardless of patient sex, except for fewer allergic reactions in male patients with female operators compared with male operators. With regard to the latter finding, underlying reasons must remain uncertain. The overall occurrence of allergic reactions in men was low and this finding could be due to chance alone. Our findings are largely in line with the Blue Cross Blue Shield of Michigan Cardiovascular Consortium’s DISCO study [17]. Similar to our study, a minority of PCI operators were women (4.5%) performing only 2.66% of all PCIs. In this study, there were no significant differences in in-hospital mortality, acute kidney injury, transfusion or major bleeding among male and female patients undergoing PCI performed by sex-concordant vs. sex-discordant operators. These findings were confirmed using adjusted linear regression models as well as propensity score matching technique. On the other hand, a recent study from Wallis et al. suggested a negative impact of sex discordance between surgeons and patients on 30-day outcomes of patients undergoing common surgical procedures [12]. Importantly, this association was still significant after adjustment for several procedural-, patient-, and hospital-related characteristics. Similarly, the treatment of female patients by male physicians was associated with increased mortality after AMI in a study by Greenwood et al. [11]. Evidence on sex- and gender-related aspects in the clinical presentation and disease course of patients with AMI is increasing. For instance, women with AMI are more likely than men to present with symptoms other than chest pain [18]. Greenwood et al. not only found better outcomes of female AMI patients when treated by a female physician but also that male physicians are more effective at treating female AMI patients when they work with more female colleagues and when they have treated more female patients in the past [11]. These findings may suggest a beneficial effect of increased awareness and knowledge about sex- and gender-related aspects in AMI patients. While this study analyzed AMI admissions from 1991 to 2010, positive changes due to ongoing efforts to raise awareness about sex- and gender-related aspects of heart disease have occurred since. These positive changes together with differences in follow-up and study endpoints may have contributed to the conflicting results.
The performance of female and male operators has been reported to be similar. The previous analysis of the ORPKI registry has confirmed similar practice patterns and outcomes of PCIs performed by female as compared to male operators [19]. Similarly, in the DISCO study, no differences in in-hospital mortality were found between patients treated by male or female interventional cardiologists [17]. Interestingly, PCIs performed by female physicians were more frequently rated as appropriate as compared to procedures performed by their male counterparts. In addition, female interventional cardiologists more frequently prescribed recommended medical therapies than male interventional cardiologists [17].
Overall, supporting more women to enter the field of interventional cardiology may lead to a more diverse workforce, which has been shown to be beneficial [20, 21]. Diversity strengthens teams and provides additional resources for problem resolution. However, despite several initiatives, including the EAPCI Women Committee, women are still underrepresented as PCI operators [22], as confirmed by our study. More efforts are needed to provide women with equitable opportunities for a successful career in interventional cardiology.
Limitations: Several limitations of this study should be acknowledged. First, the follow-up was limited to the periprocedural period, which means that assessing the long-term impact of operator-patient sex discordance was not possible. Also, the frequency of complications might be underreported. Second, the study did not evaluate the effect of concordance between patients and other catheterization laboratory staff members, such as nurses and technicians. The patients were stratified based on biological sex rather then gender, which may influence interpersonal interactions even more. Operator volume reflects the number of PCIs performed between 2014 and 2020 and may not correspond to overall operator work experience and seniority. In addition, observed differences in using antiplatelet/antithrombotic agents might be affected by the lack of data on prehospital administration of those agents. Also, the data on other drugs and procedures during in-hospital stay were not available. Consequently, the evaluation of adherence to recommendations was not possible. The ORPKI database also lacks information on lesion complexity, the extent of coronary artery disease (e.g., Syntax Score), and crucial clinical factors that may affect prognosis, such as body mass index, left ventricular ejection fraction, baseline hemoglobin level, baseline serum creatinine level, and atrial fibrillation. As no data on the change in hemoglobin level are available in the study, we could not adhere strictly to the Bleeding Academic Research Consortium criteria for evaluating bleeding events.
Conclusions
No detrimental effect of operator-patient sex discordance on periprocedural outcomes was confirmed in a large, unselected cohort of patients undergoing PCI. Some of the observed differences in outcomes between male patients discordant versus concordant with operators were primarily related to the differences in baseline risk profile.
Conflict of interest
Dr. Mehran reports institutional research payments from Abbott, Abiomed, Alleviant Medical, Amgen, AM-Pharma, Arena, AstraZeneca, AtriCure, Bayer, Biosensors, Biotronik, Boston Scientific, Bristol-Myers Squibb, CardiaWave, CeloNova, Chiesi, Concept Medical, CSL Behring, Cytosorbents, Daiichi Sankyo, Element Science, Faraday, Filterlex Medical, Humacyte, Idorsia, Janssen, Magenta, Mediasphere, Medtelligence, Medtronic, Novartis, OrbusNeich, Penumbra, PhaseBio, Philips, Pi-Cardia, PLx Pharma, Protembis, RenalPro, RM Global, Shockwave, Vivasure, Zoll; personal fees from Cine-Med Research, Ionis Pharmaceuticals, Novartis, Vectura, WebMD; Equity < 1% in Applied Therapeutics, Elixir Medical, Stel, ControlRad (spouse); Scientific Advisory Board for AMA, ACC (BOT Member), SCAI (Women in Innovations Committee Member), JAMA Cardiology Associate Editor; Faculty CRF (no fee). Other authors declare no conflict of interest.