Introduction
The prevalence of obesity among children is increasing globally. Currently, obesity has evolved into a significant worldwide health issue, with approximately 200 million school-aged children falling into the overweight/obese category. Among them, 40-50 million are classified as obese [1]. The escalation of excess body weight is a progressively mounting issue and a growing subject of public health concern within developing nations [2]. This phenomenon can potentially contribute to various health complications during childhood, adolescence, and adulthood. Even during childhood, obesity is a risk factor for future cardiovascular disease, including hypertension and dyslipidemia. These risk factors have been proven to accelerate the progression of atherosclerotic lesions in the coronary arteries of young people [3].
The global rise of childhood obesity poses a serious challenge to public health, as its occurrence continuously grows across the world. The likelihood of overweight and obese children transitioning into obese adolescents and adults is considerable, bearing significant short-term and long-term implications for both health and economics [4,5]. Medical conditions linked to obesity, encompassing metabolic syndrome, insulin resistance, type 2 diabetes mellitus, and cardiovascular ailments, previously thought to exclusively affect adults, have now manifested in the pediatric population [6].
Globally, the prevalence of obesity increased from 0.7% in 1975 to 5.6% in 2016 in girls, and from 0.9% in 1975 to 7.8% in 2016 in boys for the age-standardized base. Obesity rates exceeding 20% were observed in various nations across Polynesia, Micronesia, the Middle East, North Africa, the Caribbean, and the United States. As of 2016, an estimated 75 million girls and 117 million boys globally were classified as moderately or severely underweight. Simultaneously, approximately 50 million girls and 74 million boys worldwide were identified as obese during the same period [7]. In developing nations, the Middle East emerges with the most substantial excess of dietary energy, and there exists compelling evidence of a swift surge in risk factors for noncommunicable diseases, prominently including obesity [8]. Rates of obesity and being overweight increased significantly across different regions globally. Many studies show higher rates than in Europe. For instance, in Qatar, the prevalence of boys aged 12-17 years being overweight stood at 28.6%, while for girls in the same age group, it was 18.9% [9]. These disorders lead to high mortality and morbidity. Nutritional status has been improved a lot and because of this obesity has increased markedly in most Asian countries [10].
According to the World Health Organization (WHO), obesity is when someone’s body mass index (BMI) falls at or above the 95th percentile for their age and sex. Meanwhile, being overweight is identified as falling between the 85th and 95th percentiles on the BMI scale for age and sex. WHO’s definition of BMI pertains to the weight in kilograms divided by the square of height in meters, a metric recommended for assessing children and adolescents [11].
Hence, it is crucial to focus on preventing childhood obesity and effectively addressing overweight issues among children. The results of this study are expected to offer evidence-based suggestions for forthcoming strategies aimed at preventing non-communicable conditions like hypertension, being overweight, and obesity. Despite available data on the prevalence of being overweight and of obesity among adults, accurate figures about the prevalence of childhood obesity and being overweight among school children in developing countries are currently absent.
Aim of the work
This study aimed to explore the prevalence of obesity in school children and its related factors in an important region inside the Kurdistan Region.
Material and methods
Study design and sampling
This research constituted a cross-sectional investigation involving 550 secondary school students aged 13 to 18, comprising 316 females and 234 males. The participants were selected from 32 different public secondary schools in Duhok City, Iraqi Kurdistan. The inclusion of schools was determined through a simple random sampling method, utilizing a list of all secondary schools in Duhok City obtained from the Duhok Administration of Education. The aim was to incorporate 20% of these schools into the study. To achieve this, the names of the schools were input into the SPSS statistical software version 25, resulting in the random selection of 32 schools (21.05%) for inclusion in the study. However, the number of students selected from each school was based on the proportion of students, assuming an average of 10 classes per school. Five classes were then randomly chosen through simple random sampling, and, subsequently, 15 students from each selected class were chosen using the same sampling method. The selected students were then invited to participate in the study. The data collection was performed between November 3rd 2021 and April 10th, 2022.
Data collection methods
The research plan was approved by the research committee at Duhok University’s College of Nursing. Additionally, ethical clearance was obtained from the Directorate General of Health and the Directorate General of Education in Duhok. Subsequently, the researcher visited the selected schools to introduce the purpose of the study and received the consent of each school administration. Following the receipt of schools’ consents, a comprehensive questionnaire was crafted to gather data on personal, socioeconomic, demographic, and lifestyle aspects. Furthermore, potential risk factors were assessed through the questionnaire, and specific details such as age, gender, and parental educational background were acquired using forms that were provided alongside the consent forms.
The children’s body weight was measured using a Digital Personal Flat Scale. To ensure accurate measurements, the children were instructed to remove their shoes and any heavy clothing, such as sweaters. Body weight readings were recorded to the nearest 0.1 kg. Similarly, body height measurements were taken with precision, rounded to the nearest 0.5 centimeters. The height measurement followed a specific protocol: no shoes, heels placed together, and the head touching the measuring ruler with the ruler aligned horizontally. During the measurements, the children were directed to look straight ahead and maintain a still posture on the scale, with both feet together, legs extended, arms by their sides, and shoulders level. The stadiometer’s headpiece was gently lowered until it made contact with the top of the child’s head. The resulting height was measured in centimeters and the weight in kilograms.
Measurements
The BMI was computed as the ratio of a child’s body weight (in kilograms) to the square of their body height (in meters). To assess the BMI in relation to age and gender, growth charts released in 2000 by the Centers for Disease Control and Prevention were utilized. These charts facilitated the plotting of the BMI values against age for both males and females. The BMI categories were defined as underweight (less than the 5th percentile), normal weight (5th to 85th percentile), overweight (85th to 95th percentile), and obese (greater than the 95th percentile) [12].
Data collection occurred via a prearranged and pretested questionnaire that encompassed variables like age, gender, place of residence, sleep patterns, BMI, and dietary practices. Regarding dietary habits, factors such as the frequency of daily meals, and the consumption of junk food, sweets, and sweetened beverages were taken into consideration. In terms of physical activity, the assessment involved quantifying the daily hours dedicated to outdoor pursuits such as walking, jogging, team sports, and other similar activities.
Validity and reliability
In terms of validity, it must be mentioned that the factors included in this study were extracted from previous studies in the literature. The pre-designed questionnaire was sent to five experts in different fields for evaluation. Their comments were considered in the final version of the questionnaire before collecting the data. In terms of reliability, the first 10 cases were collected by the first and third researchers. The obtained data were entered into statistical software for analysis. The final output showed no significant difference between these two measures. Therefore, we considered the measures reliable in this study.
Statistical analyses
The general information of school children was presented in mean and Sta. Deviation or number and percentage terms. The prevalence of obesity and being overweight among school children was determined in number and percentage terms. The association of being overweight and of obesity with general characteristics, diet behaviors, lifestyles, and parents’ characteristics were examined in a Pearson chi-squared test. The predictors of obesity were determined in the nominal logistic regression model. A significant level of difference was identified in a p-value<0.05. The JMP Pro 14.3.0 was used for the statistical calculations.
Results
Demographic characteristics of the children
The mean age of the children was 15.54 years, with ages ranging between 13 and 18 years old. The study included both male (42.54%) and female (57.46%) participants, residing in both urban (90.0%) and rural areas (10.0%). The findings indicated that half of the children engaged in regular physical activity, with 23.64% exercising for less than 30 minutes per day, 21.27% for more than 45 minutes per day, 30.18% for 1-3 times per week, and 19.64% for 4-7 times per week. The majority of the children were classified as normal sleepers (58.55%), followed by long sleepers (37.27%), with the remaining classified as short sleepers (4.18%) (Table 1).
Table 1
General information on the school children
Dietary behaviors of the children
The study revealed that a majority of the children consistently consumed breakfast (66.91%), lunch (83.27%), and dinner (89.64%), with 53.27% opting for an additional portion of food. Furthermore, the findings indicated that a significant portion of the children regularly consumed junk food, with 52.0% indulging up to 3 times per week and 39.46% consuming it more than 3 times per week. Conversely, the majority of the children predominantly consumed homemade food (91.64%). The prevalence of the consumption of sugar-sweetened drinks (SSB) was high, with 89.64% of children drinking them 1-3 times per day (85.09%) or 4-7 times per day (4.55%). Additionally, the study highlighted that 17.82% of children used fat in their food freely, while 82.18% employed mild to moderate levels of fat usage (Table 2).
Physical activity and obesity among children’s parents
The study revealed that a significant proportion of the children’s parents had either no education or a low level of education. Additionally, approximately one-fourth of the parents were classified as being overweight or obese. Only a small percentage of the parents engaged in regular physical activity. Regarding health conditions, the prevalence of diabetes mellitus among fathers and mothers was found to be 12.73% and 12.36%, respectively (Table 3).
Table 3
Characteristics of parents of the school children
Obesity in children and its associated general and dietary characteristics
The study indicated that among school children, the prevalence of being overweight and of obesity was 13.27% and 14.91%, respectively. The majority of children were within the normal weight range (64.55%), while 7.27% were classified as underweight. Interestingly, the study found that females were more likely to be overweight (16.77%) and males were more likely to be obese (13.68%; p=0.023). Furthermore, the prevalence of obesity was not significantly associated with residency (p=0.3257), exercise (p=0.3508), sleep patterns (p=0.4569), or media consumption (p=0.6555; Table 4).
Table 4
Association of obesity with general information on the school children
Furthermore, our analysis did not reveal a significant difference in the prevalence of obesity and being overweight among children with varying dietary behavior characteristics (Table 5).
Table 5
Association of obesity with the dietary behavior information on the school children
However, the study did uncover a notable association between children with overweight or obese fathers and the likelihood of being overweight/obese in children. Interestingly, the prevalence of being overweight and of obesity among children was not found to be associated with other general characteristics of the parents (Table 6).
Table 6
Association of obesity of school children with parents’ characteristics
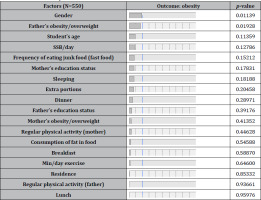
Predictors of obesity of school children
The study revealed that being male and having overweight or obese fathers were significant predictors of the prevalence of obesity among the school children. However, other factors examined were not shown to predict obesity among this demographic, as depicted in Table 7.
Discussion
This study showed that most children had normal BMI values (boys, 61.97%; girls, 66.46%), 14.91% were overweight (boys, 12.39%; girls, 16.77%), and 13.27% were obese (boys, 13.68%; girls, 12.97%). The prevalence of being overweight in our sample of children was 14.91%.
The findings reported in this study are similar to those observed in certain neighboring Middle Eastern nations, such as Jordan [13]. However, this investigation also revealed that the occurrence of being overweight and of obesity among Duhok adolescents was comparatively lower than in several other countries. For instance, in Saudi Arabia the prevalence of being overweight and of obesity in adolescents aged 15-19 years was reported as 16% and 24%, respectively [14]. Meanwhile, among adolescents with a mean age of 14.9 years in the eastern United States, the projected prevalence of being overweight was 19.8%, and for obesity, it was 26.6% [15]. Additionally, the rates of being overweight and of obesity discovered in this current research were similar to those documented among Chinese adolescents aged 13-17 years [15].
The present study showed a lower prevalence compared to research findings in Ghana, which reported a rate of 16.4% [16], and in China, where the rate was 20.0% [17]. The variability in these rates may stem from diverse factors, including socio-demographic and economic distinctions [18]. The prevalence of being overweight and of obesity among secondary school students in the Kurdistan Region exceeds those in certain other countries. For instance, in Morocco, the prevalence of being overweight and of obesity in adolescents aged 12-18 years was estimated at 7.69% and 3.41%, respectively [18].
An additional potential explanation for the escalation of obesity among younger individuals could be their increased exposure to fast food compared to older age groups. Our investigation showed a noticeable elevation in the prevalence of being overweight and of obesity linked to gender. Our findings indicated that the prevalence of being overweight was greater among girls than boys, and this discrepancy was statistically significant (16.77% vs. 12.39%).
The findings from this study are different to the results from other research that indicated elevated rates of weight gain and obesity among girls [19]. The observed sex-related differences in our study can potentially be attributed to the fact that boys have more exposure to unhealthy fast food compared to girls. The boys in our region have increased opportunities to spend time with their friends away from home. Our study identified a prevalence of weight gain and obesity among Kurdish teenagers, with boys being at a higher risk of obesity compared to girls. The gender-based variations observed in our study can be ascribed to the distinct characteristics of Kurdish culture. Contrarily, adolescent girls, who often place a heightened emphasis on their body image, tend to adopt healthier dietary practices and demonstrate greater vigilance over their eating habits.
The impact of gender on obesity can be linked to hormonal shifts during puberty, leading to the emergence of secondary sexual traits that facilitate the accumulation and redistribution of fat [20]. The WHO recommends that children and adolescents aged 5-17 engage in a minimum of 60 minutes of moderate to vigorous-intensity physical activity daily. It is advised to include vigorous-intensity exercises that promote muscle and bone strength, at least three times a week [21].
The prevalence of being overweight and obese was not significantly different between urban and rural areas than in our study. The prevalence of obesity based on the residency could be different within various geographic locations [22,23]. The culture of the people in urban and rural areas of developing and developed countries could be a reason for this discrepancy.
Although the study indicated a lack of statistical significance between BMI and the educational background of parents. It is worth noting that higher BMI in children often appears linked to parents with lower levels of education. Educated individuals tend to exhibit a greater awareness of this issue and a higher dedication to safeguarding their children against the risks of excess weight and obesity [23].
Contrary to other research [24], this study found no correlation between watching TV for more than 3 hours per day and having a high BMI. Unlike some studies where BMI was notably linked to increased hours of TV viewing per day, this inconsistency might be attributed to the cultural norm in our society, where the practice of eating while watching TV is less prevalent.
Sleep duration, which regulates body weight and metabolism through the modulation of pivotal hormones such as leptin [25] emerges as a noteworthy factor. However, it could also potentially be a secondary consequence of being overweight or obese [26]. In contrast, factors such as the consumption of “junk” food [26] did not yield significant results in our study.
The association between obesity and being overweight and the fathers’ occupation and education level was not statistically significant in our study. Although the study showed that children primarily consumed meals at home, they still encountered the availability of harmful items like chips, sugary beverages, and sweets at school. The behavior of consuming junk food and sweet beverages is common in other regions as well [27]. This situation poses a hazard to children’s growth and well-being, contributing to both the risk of obesity and noncommunicable diseases (NCDs) due to the inadequate expenditure of energy that children consume [28]. The excess energy is subsequently stored as body fat, leading to an elevation in body weight and placing a child at risk of developing obesity, cardiovascular ailments, and diabetes [29].
Recommendations
The outcomes of the current study call for the necessity to establish a strategic approach for preventing and addressing this growing endemic. Contemporary dietary behaviors significantly contribute to the emergence of childhood obesity, necessitating careful observation and control. We propose the implementation of platforms aimed at educating adolescents about the significance of balanced nutrition, along with increasing awareness about the risks associated with excessive weight gain. Such measures are pivotal in the prevention of nutrition-related ailments. Furthermore, it is advisable to incorporate courses in the high school curriculum in Duhok that promote the adoption of healthy eating habits and regular engagement in sports and physical activities. Moreover, the introduction of supplementary educational initiatives to address matters linked to being overweight and to obesity is crucial for nurturing a generation characterized by both physical health and mental well-being.
Strengths and limitations
The strong points of this study are including a sufficient sample size of school children through a random sampling technique. However the study was not exempt from limitations. The variables included in the study were self-reported data, introducing the potential for both over- and under-reporting. In addition, we may have not included all the related factors to being overweight and obesity, such as social and psychological factors. We used the BMI as an indicator of obesity. BMI is not as accurate an index as waist-hip ratio and skin-fold thickness, which directly measure fat mass. It’s important to emphasize the need for further research to explore other relevant factors that were not covered in the current study.
Conclusions
To summarize, the study revealed a notable prevalence of being overweight and of obesity among adolescents residing in Duhok City. The escalation in obesity rates is likely attributed to swift urbanization, the shift from traditional to Western lifestyles, and the adoption of unhealthy dietary patterns. The study identified that being the female gender and having a father who is classified as overweight or obese were associated factors to obesity and being overweight.