Summary
This study presents a comprehensive investigation into percutaneous closure methodologies applied to coronary artery fistulas (CAFs), a relatively uncommon cardiac anomaly characterized by anomalous connections between coronary arteries and adjacent structures. The study entails a retrospective analysis involving 39 patients who underwent transcatheter closure of CAFs, employing a range of techniques including coil embolization, cyanoacrylate injection, and detachable balloon angioplasty. The achieved procedural success rate of 87.1% underscores the efficacy of these interventions, revealing favorable outcomes in terms of symptomatic amelioration and reduced dependence on anti-anginal medications over a median follow-up duration of 98 months. Noteworthy is the manageable nature of complications encountered, none of which necessitated surgical interventions. The study underscores the evolving landscape of CAF management, accentuating the promising potential of minimally invasive percutaneous closure strategies in enhancing patient outcomes and mitigating symptomatic burdens.
Introduction
Coronary artery fistula (CAF) is a rare coronary anomaly and arises from abnormal communications that develop between one or more coronary arteries and adjacent great vessels or cardiac chambers. The exact prevalence is unknown, but CAF has been reported to occur in approximately 0.1% to 0.2% of all patients who underwent invasive coronary angiography [1]. Although the majority of CAFs are congenital, some of them are acquired due to multiple factors such as vasculitis, vascular trauma during coronary intervention, coronary atherosclerosis or cardiac surgery [2]. Although most CAFs are generally detected incidentally during coronary angiography or noninvasive cardiac imaging, their clinical importance is due to the risk of several complications including heart failure, infective endocarditis, myocardial ischemia, and dysrhythmias [2].
The 2018 American College of Cardiology/American Heart Association guidelines for the management of adults with congenital heart disease recommend closure of CAFs in symptomatic patients and large CAFs irrespective of the presence of symptoms [3]. Surgical closure is accepted as the main therapeutic option for symptomatic CAF. However, transcatheter CAF closure has emerged as a safe and feasible alternative to surgical closure associated with a less invasive procedure, shorter hospitalization and recovery periods and favorable follow-up results [4]. This technique has seen significant advancements since its first application by Reidy et al. [5] in 1983, with various tools and methods now available for the procedure. Several techniques are used for percutaneous closure of CAFs such as coil embolization, occlusion with alcohol foam, percutaneous coronary intervention with detachable balloons, covered stents or with occluder device implantation [6–8]. However, experience and long-term follow-up results with transcatheter closure remain limited.
Aim
We aimed to present periprocedural and long-term outcomes of patients who underwent percutaneous coronary artery fistula occlusion in our center.
Material and methods
Study population
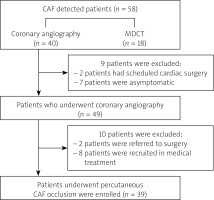
Thirty-nine patients with congenital CAF who underwent transcatheter closure at Hacettepe University, Ankara, Turkey between January 2002 and April 2022 were retrospectively reviewed. Patients who had symptoms or complications related to coronary artery fistula such as heart failure, infective endocarditis, arrythmias or myocardial ischemia and asymptomatic cases with large coronary artery fistula or aneurysm malformation were considered for transcatheter occlusion. The significance of the fistula for treatment was determined based on symptoms such as palpitations, dyspnea, and angina, which could not be explained by other reasons, as well as the specific characteristics listed above. This issue falls within the gray areas of cardiology, and there is no complete consensus on it in the literature. Patients who refused interventional treatment or underwent surgical closure were excluded. Demographic data, periprocedural characteristics, and outcomes during follow-up were obtained from patients’ files and the electronic database of hospital records. The study was approved by the Institutional Ethics Committee (Ethical approval date/decision number: 01.11.2022/2022/18-48) (Figure 1).
Preprocedural management
Detailed physical examination, electrocardiogram and transthoracic echocardiography was performed in all patients and detailed medical history was noted prior to the procedure. Coronary artery fistula was diagnosed via conventional coronary angiography or noninvasively by multi-detector computed tomography (MDCT). All symptomatic patients and patients with large coronary artery fistula (> 8 mm) underwent invasive coronary angiography for assessment of the eligibility of percutaneous closure. In patients receiving warfarin, INR level < 2.0 was targeted and direct oral anticoagulants were discontinued 24 h before the procedure.
Procedures
Informed consent was taken from all patients and procedures were performed under appropriate conscious sedation. The selection of occlusion devices mostly depends on the age of the patient, associated cardiac diseases and the anatomic characteristics of the fistula. According to the selected methods, the transvenous or transarterial approach can be performed. The transarterial approach by the radial or femoral artery is most used for fistulas originating from the proximal coronary, as there is a shorter distance to traverse through the parent vessel. Occlusion of fistulas was achieved with coil embolization, detachable balloon angioplasty or a chemical agent (cyanoacrylate) transfemorally in our center.
Selective coronary angiography is the most important step in percutaneous intervention and is performed to evaluate the both anatomy of the entire native coronary arteries and features of the coronary artery fistula including origin, location, size, number of branches and drainage site in order to determine a suitable treatment option. Patients with concomitant critical coronary artery stenosis underwent percutaneous coronary intervention either during the index procedure or in a subsequent session, depending on the preference of the interventionalist. Right heart catheterization was performed in cases with coronary artery fistula causing suspected hemodynamically significant left-to-right shunt, especially in those who were found to have a high Qp/Qs ratio on echocardiography, to assess the necessity of coronary artery fistula occlusion. Procedural success was defined as either the complete occlusion of the fistula or reduced flow to less than 10% of the baseline flow.
Coil embolization
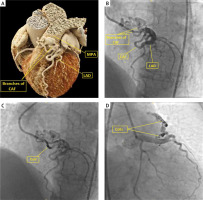
After the cannulation of coronary vessels with a 7- or 8- Fr JR (Judkins Right) guiding catheter for the right coronary artery (RCA) and a 7- or 8-Fr JL (Judkins Left) guiding catheter for the left main coronary artery (LMCA), unfractionated heparin (60 to 100 IU/kg, targeted ACT level of > 250 s) was administered intravenously. A 0.014-inch guidewire was advanced into the fistula course. After selective catheterization of the fistula with microcatheters (Excelsior microcatheter, Boston Scientific, Fremont, CA, USA) over the floppy wire, detachable coils were used to occlude fistulas (Micrus Microcoil System, Micrus, San Jose, California, USA). It is suggested that the coil diameter is slightly larger than the vessel diameter (30% larger) to prevent coil displacement and migration. They were placed sufficiently far from the drainage opening to prevent migration into the pulmonary artery (PA) and just at a vessel curve before the branch. It is important to keep the position of the microcatheter and release the coils just at a vessel curve. To obtain complete occlusion, coils were implanted so as to merge together, forming a conglomeration. After coil deployments, coronary angiography was performed to assess the presence of residual flow. In cases with significant residual flow and amenable anatomy, additional coils were deployed until a suitable closure was achieved. Procedures with less than 10% residual flow were considered as a successful procedure and the procedural success was determined with a final angiography (Figure 2).
Figure 2
A – 3D reconstructed CT image of coronary artery fistula (CAF) originating fom left anterior descending artery (LAD) and draining into the main pulmonary artery (MPA). B – Coronary angiography shows the CAF between the LAD and MPA. C – Occlusion of the branch of the CAF with coil embolization. D – Blood flow stopped in CAF after embolization of the two branches of the CAF
Cyanoacrylate technique
For closure with glue (cyanoacrylate), initially the coronary ostium was catheterized with guiding catheter and a 0.014-inch guidewire was introduced through the catheter and advanced into the fistula. Then, the CAF was selectively cannulated with a 4-Fr catheter (GlideCath Vertebral, Terumo Europe N.V., Leuven, Belgium) and a microcatheter (Excelsior SL-10, Boston Scientific, Fremont, CA, USA) was advanced deep enough into the fistula through the 4-Fr catheter. Glue was mixed with Lipiodol (Lipiodol ultra-fluide, Guerbet, France) to make the occlusion of the fistula visible by fluoroscopy. Approximately 0.5 ml of cyanoacrylate (Liquiband; MedLogic Global, Plymouth, Devon, England) was mixed with 2.5 ml of Lipiodol and 1/6 diluted glue was yielded. The mixture was inserted into the fistula and afterwards a final angiography was performed.
Detachable balloon technique
Percutaneous transcatheter closure with a detachable balloon (GVB16, Minvays, Gennevilliers, France) was performed after cannulation of the coronary artery with a 8-Fr Judkins guiding catheter. Afterwards, a 0.014 inch guidewire was advanced through the fistula course and a detachable balloon was advanced over the guidewire. When the position of the balloon was suitable, occluding the artery, it was detached by gentle traction and subsequent coronary angiography was performed for the evaluation of residual flow.
Follow-up
Electrocardiography (ECG) and transthoracic echocardiography were performed on the day of the procedure prior to intervention. ECG was performed and blood was sampled for troponin measurement after the procedure. Asymptomatic cases with normal troponin level and without any ECG changes were discharged the next day. Upon discharge, patients received antiplatelet therapy based on the results of coronary angiography. If atherosclerotic heart disease was detected, and no interventional procedure other than fistula closure was performed, aspirin alone was initiated. In cases where coronary artery disease was not detected, no antiplatelet therapy was administered following fistula closure. Patients with a prior diagnosis of atherosclerotic heart disease continued their existing antiplatelet therapy with aspirin. Routine follow-up visits were scheduled after 1, 6 and 12 months and annually thereafter. If patients had symptoms consistent with recurrence of coronary artery fistulas, contrast enhanced coronary BT angiography or re-do invasive coronary angiography was performed. The treadmill exercise stress test or myocardial perfusion scintigraphy was performed for ischemia detection in selected patients.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation or median (interquartile range – IQR), while categorical data are expressed as percentage (%). Comparison of parameters before and after the coronary artery fistula occlusion was assessed using the Wilcoxon rank test or paired sample t-test. Categorical dependent variables were compared using the McNemar test. SPSS software (version 22.0; IBM) was used for statistical analysis. Two tailed p-values lower than < 0.05 were considered statistically significant.
Results
We screened 58 patients with the diagnosis of coronary artery fistula which was detected by MDCT or conventional coronary angiography and enrolled a total of 39 patients after excluding 19 cases. Mean age of the study population was 57.3 ±12.5 years and 59% of the cases (n = 23) were male. Hypertension was present in 22 (56.4%) patients and diabetes was present in 8 (20.5%) cases. The most common complaints at application were angina (69.2%) and exertional dyspnea (38.4%). Many of the cases (51.2%) were under treatment with at least one antianginal drug. Presence of ischemia was established with myocardial perfusion scintigraphy in 7 cases, while the treadmill exercise test detected ischemia in 9 patients. Baseline characteristics and echocardiographic measurements are presented in Table I.
Table I
Baseline characteristics of the study population (n = 39)
[i] Data are mean ± standard deviation or median (min.–max.), or number (%). ACEi – angiotensin converting enzyme inhibitors, ARBs – angiotensin receptor blockers, NOACs – novel oral anticoagulant agents, LA – left atrium, LVEDD – left ventricular end-diastolic diameter, LVEF – left ventricular ejection fraction, sPAP – systolic pulmonary artery pressure, RVEDD – right ventricular end-diastolic diameter.
A total of 50 fistulas were detected in 39 patients. Single CAF was established in 30 (76.9%) cases, while 7 (17.9%) patients had two CAFs and 2 (5.1%) patients had three CAFs. Median size of the CAFs was 2 (1–9) mm and a large fistula was detected in only 2 (5.1%) patients. Right heart catheterization was performed in 2 cases with suspected significant left-to-right (LR) shunt and moderate LR shunt (Qp/Qs = 1.4–2.2) was confirmed in both of them. Most of the CAFs originated from the left anterior descending artery (n = 19) and right coronary artery (n = 19). Although there were several draining sites, the pulmonary artery was the most common draining site (n = 22), followed by the right ventricle (n = 16) and left atrium (n = 5).
Coil embolization was preferred in most patients (n = 36), while cyanoacrylate was used in 3 cases. Detachable balloon angioplasty was performed in only 1 case due to inappropriate coronary anatomy consisting of high risk for coil embolization to the pulmonary artery. Combined coil and cyanoacrylate embolization was used in 1 patient. Procedural success was achieved in 34 cases while the intervention failed in 5 patients. Complete occlusion was carried out in 32 patients. Origin of the fistula was the left anterior descending artery in all of the cases with a failed procedure. Two of the failed patients underwent surgical occlusion while the remaining 3 cases were followed with medical treatment.
One patient had atrial fibrillation immediately after the intervention, which returned to sinus rhythm with medical cardioversion. Also, 3 patients had chest pain early after fistula closure. But electrocardiographic records were unremarkable and cardiac markers were within normal limits. The echocardiographic examination revealed normal findings with no segmental wall motion abnormalities. A femoral artery pseudoaneurysm occurred at the insertion site in 2 cases, and the pseudoaneurysms thrombosed after manual compression in both cases. Pericardial effusion developed in 2 patients and resolved with medical treatment during follow-up. Transient ischemic attack developed in 1 patient during coronary angiography and the transcatheter occlusion procedure was postponed for 3 months. Contrast-induced nephropathy occurred in only 1 case and renal functions recovered with intravenous saline infusion. Characteristics of fistulae and procedures are presented in Table II. During follow-up anginal symptoms occurred in 18 cases. Ischemia was documented in 4 patients and they underwent coronary angiography. Significant coronary artery lesions were detected in 2 of them. CAFs were still occluded in the remaining 2 cases and patients were diagnosed with microvascular angina. Follow-up coronary imaging was performed due to symptoms regarding ischemia in 14 cases without documented ischemia via myocardial perfusion scintigraphy (MPS) or the treadmill exercise test (10 patients with CT angiography and 4 patients with invasive coronary angiography). Recanalization was detected in 2 patients and re-do coil embolization was performed in one of them, while the other case was followed with medical treatment due to the patient’s refusal of intervention. Median Canadian Cardiovascular Society angina class was reduced (1 vs. 0; p < 0.001) and the median number of anti-anginal drugs used decreased (1 vs. 0; p = 0.001) in the long term. The percentage of patients with dyspnea was also distinctly reduced and mortality occurred in only 1 case during a median of 98 (6–195) months of follow-up (Table III).
Table II
Characteristics of fistulae and procedures
Discussion
In this study we report the one of the largest series and follow-up periods in patients who underwent transcatheter coronary artery fistula occlusion in the literature. We established that transcatheter CAF occlusion is a safe procedure and it has favorable long-term outcomes. Most of the patients included in our study had symptoms related to CAF and only 2 patients underwent the procedure due to large CAF without symptoms.
In our study, CAFs originated from the RCA (38%) and left anterior descending (LAD) (38%) and 32/39 (82.0%) cases had a single CAF mainly draining to the pulmonary artery. CAFs can occur from any of the major coronary arteries, including the left main coronary artery, but the majority of them originate from the RCA or LAD, with the Cx being less commonly involved [2, 9]. CAFs mostly drain into right-sided chambers and venous circulation rather than left-sided chambers due to relatively low pressure inside right-sided chambers compared to left-sided chambers. Most of the patients (80%) had a single CAF, and multiple fistulas were detected in a small proportion of cases [10–12].
Transcatheter closure of coronary artery fistulas may be achieved by two different approaches. The transarterial approach is appropriate for fistulas certainly originating from the proximal part of the coronary artery, whereas the transvenous approach should be considered in patients with fistulas from the distal coronary bed. Coil embolization should be preferred in tortuous fistulas, while both coil embolization and closure with a vascular plug are suitable for straight fistulas. There are different types of coils including pushable stainless steel or platinum coils and detachable coils. Pushable coils can be used in fistulas with a small diameter, while detachable coils should be preferred in larger fistulas due to increased embolization risk [13]. The aneurysmal proximal coronary artery segments (> 10 mm) that develop in large distal CAFs are related to an increased risk of thrombus formation secondary to stagnant flow. Therefore patients with a large fistula with an enlarged coronary artery and cases with significant myocardium at risk in case of complications during transcatheter fistula closure should be referred for surgical closure [14, 15]. Graft covered stent implantation might be an option in treating plexiform fistulas with multiple origins or lesions with unfeasible anatomy for embolization with coils or occluders. However, it should be noted that stent grafts have a 10–15% risk of thrombosis [16].
Among the transcatheter interventions, percutaneous closure with coil embolization is the most frequent and widely accepted method. El-Sabawi et al. [17] recorded a 90% acute procedural success rate in 45 patients with 56 CAF closures with complications including device migration in 3 patients, intracranial hemorrhage in 1 patient, and MI in 4 patients. All device embolization cases occurred in patients treated with pushable coils. In another series of 33 patients, Armsby et al. [18] reported successful closure in 82% of cases and complications including 5 cases of transient ST-T-wave changes, 4 cases of transient arrhythmia, 1 case of coronary spasm, 1 case of fistula dissection, and 1 case with unretrieved device embolization. Transcatheter CAF occlusion is a safe intervention in experienced centers and reported complication rates are reasonable. Pericardial effusion, arrhythmias, insertion site complications, coronary artery dissection, transient ischemic attack, AV block and distal embolization are complications reported in the literature [19, 20]. Extreme vessel tortuosity, large fistula size and multiple drainage sites are important limitations of the percutaneous intervention and main causes of complications [2]. In our trial, the procedural success rate was found to be 87.1% and complications included 2 cases of insertion site problems (pseudoaneurysm), 2 cases of pericardial effusion, 1 case of transient ischemic attack and 1 case of contrast-induced renal failure. None of our complications required surgical intervention and they recovered during follow-up.
In our study group, most of the patients were symptomatic; only 2 cases were asymptomatic with large CAFs. Thirty-six of the CAFs were closed via coil embolization, in 3 patient cyanoacrylate and in 1 patient balloon detachment was used. Only in 1 patient was a combination of coil embolization and cyanoacrylate used due to incomplete occlusion. In 1 patient with the complication of infective endocarditis, the CAF was closed with a detachable balloon; only partial recanalization was observed in the follow-up and an additional intervention was not planned. Balloon detachment procedure was selected because of the large and tortuous CAF. Closure with the combination of glue (cyanoacrylate) and coil was used in 1 patient because of residual flow after coil embolization. Combination of these 2 methods made the intervention successful without residual flow at follow-up angiography. Besides the widely used coil embolization technique, both closure with glue (cyanoacrylate) and balloon detachment seemed to be effective and safe methods of percutaneous transcatheter closure intervention. But these methods have not been widely used recently.
Not every patient is a suitable candidate for coronary artery fistula closure. While there may not be a definitive consensus in this regard, contraindications for CAF closure can vary based on individual patient factors and specific clinical scenarios. Nonetheless, some common contraindications may encompass severe comorbidities that increase procedural risks, substantial distal vessel disease hindering access and closure, active infections, and patients who are unwilling or unable to comply with the required post-procedure follow-up and surveillance. It is imperative to evaluate each case on an individual basis, taking into account the potential risks and benefits before determining the appropriateness of CAF closure. In our study, closure decisions were made taking these factors into consideration.
In the follow-up, symptomatic patients were evaluated with MDCT coronary angiography. To detect the fistula origin, course and drainage site, and relationship of anatomic structures, MDCT has an important role both in diagnosis and follow-up because of its higher spatial and temporal resolution properties. Prognosis of our patients after the closure procedure is good in long-term follow-up results (median: 98 months, range: 6 to 195 months). It was reported in a retrospective study with mean 4 years follow-up that transcatheter CAF occlusion was related to significant improvements in symptoms including palpitations, dyspnea and angina [19]. We found that improvement of patients’ symptoms such as angina, dyspnea and palpitation were significant after a median 98 months follow-up and the number of prescribed anti-anginal drugs was distinctly lower than prior to the procedure in the long term. These findings suggest that transcatheter closure of the CAF is an effective and safe method in the appropriate coronary anatomy.
This study represents the results of the retrospective data from a single center experience; therefore prospective, multicenter studies will be valuable for obtaining more certain and evidence-based knowledge. Follow-up coronary artery imaging was not performed in all cases. Therefore there might be some overlooked asymptomatic cases with CAF recanalization. New atherosclerotic lesions yielding anginal symptoms might have developed during follow-up as atherosclerosis has a progressive course and angina assessment during follow-up does not reflect only CAF-related angina.
Conclusions
Coronary artery fistulae are rare but may cause symptoms including angina, palpitations and exertional dyspnea. Occlusion of the coronary artery fistula should be considered in symptomatic cases and asymptomatic cases with large fistulae. Procedural success rate and long-term outcomes of percutaneous CAF occlusion are reasonable, and it is a safe intervention in experienced hands with low complication rates.