Percutaneous mitral balloon valvuloplasty (PMBV) is a treatment of choice in selected symptomatic patients with mitral stenosis. Frequency of mitral restenosis after PMBV may be as low as 4% in selected subgroups [1]. However, in a real-life population the need for repeat mitral intervention (PMBV or surgical) may approach 40%. The inability to cross the mitral valve (MV) accounts for a non-negligible rate of unsuccessful PMBV.
A 47-year-old female patient after PMBV 4 years ago, with heart failure class III according to the New York Heart Association and rheumatoid arthritis was admitted due to MV restenosis. Transthoracic echocardiography (TTE) revealed fusion of both mitral commissures, mean mitral gradient (MG) 12 mm Hg; maximal MG 27 mm Hg and mitral valve area (MVA) by planimetry 1.0–1.2 cm2. Left atrium (LA) area was enlarged to 27 cm2. The standard PMBV procedure with the Inoue balloon was initiated via the right femoral vein. Septal puncture was performed under guidance of transesophageal echocardiography (TEE), which was then removed. After having placed the balloon into the LA, several maneuvers aiming to cross the MV orifice were done. However, the balloon’s shape during initial inflation of the distal chamber was not typical and the balloon slipped away without full inflation (Figure 1). Thus, high suspicion was raised that the balloon was advanced into the left pulmonary vein (PV) instead of across the MV. Direct TTE monitoring during the next attempts clearly showed that the balloon did not cross the MV. After a few more and unsuccessful attempts to cross the MV, the procedure was stopped without acute complications. So we planned a second approach with TEE guidance extended to MV crossing (if needed). The next procedure was done 1 month later using a slightly different septal puncture. MV crossing with the balloon was possible without TEE guidance and successful balloon inflations across the MV were done. Post-procedural MG decreased to 13/7.2 mm Hg (maximal and mean, respectively). MVA was found to be 1.9–2.0 cm2 by planimetry.
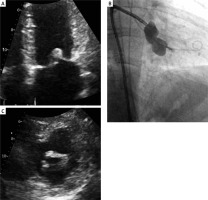
Figure 1
A, B – Transthoracic echocardiography (apical view and parasternal short axis view): thickened leaflets of the mitral valve with significant stenosis. C – Percutaneous mitral balloon valvuloplasty: atypical shape of the Inoue balloon during first inflation (probably in the pulmonary vein, and not across the stenotic mitral valve)
With this case, we want to show a possible (and dangerous) complication of PMBV, if the catheter placement is incorrect and unrecognized before balloon inflation. Apparently, only a few cases of PV rupture, either iatrogenic [2] or due to blunt chest trauma [3, 4], have been reported. To our best knowledge, no reports of PV injury during PMBV have been presented before. Proper transseptal puncture is crucial for further maneuvering of the catheter within the LA. Probably the transseptal puncture during our first approach was not optimal. For most PMBV cases, the preferred transseptal puncture site is in the posterior and inferior region of the fossa ovalis. We do not routinely use TEE guidance during MV crossing or for intraprocedural MV assessment after sequential balloon inflations. However, TEE guidance may be helpful, especially in patients with very dilated LA, unusual IAS morphology (such as abnormal IAS bulge), critical mitral stenosis (MVA < 0.5 cm2) or subvalvular disease. TEE is very helpful to optimize balloon position across the MV leaflets, avoid entrapment in the subvalvular apparatus or balloon advancement into the PV (as probably occurred in our case).
Improper advancement of the Inoue-balloon into the PV may occur during PMBV. Vigilant balloon inflation (and quick deflation) is crucial to avoid serious complications. TEE guidance during PMBV may be indispensable in patients with unfavorable anatomy.








