Summary
Although antegrade intervention technique is frequently used in the endovascular treatment of femoropopliteal artery occlusive disease, it has been reported to be associated with failures and some intervention site complications in occlusive and complex lesions. We evaluated 45 procedures performed in our hospital within the scope of our study to investigate the safety and effectiveness of the retrograde popliteal artery intervention technique, which is one of the intervention options in the endovascular treatment of the disease. According to the results of our study, we believe that the retrograde popliteal artery intervention technique is an effective and safe option for endovascular revascularization, especially in long segment and complex femoropopliteal artery occlusions.
Introduction
The role of endovascular treatment modalities in the current management of occlusive peripheral arterial disease (PAD) has been reported to be increasing [1, 2], and most patients with symptomatic occlusive PAD have extensive complex lesions and occlusions in the superficial femoral artery (SFA) [3]. Although surgical revascularization is recommended as the first-line revascularization in this group of diseases, the majority of which are reported to be long segment occlusions [4], endovascular procedures can also be successfully performed in SFA occlusive disease involving the proximal popliteal artery (PA) segment [5]. In the Global Vascular Guidelines (GVG), recommendations are expressed in the management of chronic leg ischemia, taking into account the severity of the disease and its anatomical classification [6]. Even though it has been reported that femoropopliteal artery (FPA) endovascular revascularization procedures are often performed with contralateral femoral artery or ipsilateral femoral artery interventions, and antegrade femoral artery interventions, which are technically relatively challenging, have the advantage of better control [7], it has also been reported that recanalization failure may occur in approximately 20% of patients due to the inability to re-enter the distal true lumen, and some materials have been developed for this reason [8, 9]. Moreover, it has been reported that the retrograde endovascular access technique with PA intervention, which was previously considered a substitute option, has been evaluated to increase the success rates in SFA recanalization [1] and is a valid alternative [10, 11].
Aim
The aim of this study was to evaluate the safety of PA retrograde intervention and our early procedural success rate in endovascular revascularization of symptomatic FPA occlusive disease.
Material and methods
Patients who underwent endovascular revascularization due to occlusive FPA and whose clinical data could be obtained from a total of 95 endovascular revascularization procedures performed for treating symptomatic occlusive peripheral artery disease between June 2016 and October 2017 were included in this retrospective study. The study was approved by the ethics committee of the institution (2017, TUEK-30278912), and the study was conducted in accordance with the Declaration of Helsinki guidelines. Inclusion criteria were defined as patients who underwent endovascular revascularization procedures for symptomatic (Fontaine class 2b-4) occlusive FPA disease and using medical therapy for PAD due to complaints of more than 2 months. Patients with critical leg ischemia (Fontaine class 2b-4) with occlusive SFA or SFA + PA disease who were receiving medical treatment for their complaints were included in the study. All patients included in the study were evaluated before the procedure for occlusive FPA by Doppler ultrasonography (DUS) or computed tomography angiography (CTA). Patients who underwent hybrid (bypass grafting surgery + endovascular procedure) revascularization in the same session, patients who underwent a percutaneous endovascular procedure for iliac artery occlusive disease or below-knee arterial occlusive disease in the same session, patients whose endovascular treatment could not be performed due to intervention failure, patients who underwent thromboembolectomy for acute arterial thromboembolism, patients who underwent an endovascular procedure for arterial aneurysm, patients who underwent aneurysm repair, patients who underwent endarterectomy of their common femoral arteries (CFAs), and patients who had previously undergone peripheral arterial bypass grafting or endovascular treatment for existing FPA disease were excluded. Medical information of the patients was reviewed from the hospital automation system and patient files and recorded. Informed consent was obtained from all patients for the endovascular interventional procedure for the treatment of obstructive PAD, and acetylsalicylic acid (ASA) + clopidogrel treatment had been initiated in the pre-procedure period. All procedures were performed in the angiography unit or in the cardiovascular surgery operating room with a scoping device. Patients who underwent antegrade revascularization via CFA were assigned to the Antegrade Group (n = 33) and patients who underwent retrograde revascularization via PA were assigned to the Retrograde Group (n = 12). PA intervention was performed as the first-line procedure in patients with obstructive FPA disease who were considered to have severe stenosis or occlusion in the CFA or no stump in the proximal SFA on CTA examinations, while in eligible patients, the antegrade intervention was attempted first through the ipsilateral or contralateral CFA, and in the case of failure to pass the lesion, the patient was turned to the prone position and retrograde intervention from the PA was performed with ultrasound guidance. Ultrasonographic imaging was used to evaluate the PA, and compression maneuvers were used to evaluate the popliteal artery and vein. For image quality, an ultrasound-guided PA puncture (with an 18G needle) was performed first and local anesthesia was then applied and a 6-7F introducer was inserted into the popliteal artery in accordance with the physician’s evaluation. In all patients following arteriography, 5000 IU of intravenous heparin was administered, and recanalization was first attempted using 0.035″ hydrophilic guidewires, and a support catheter was used for failure to pass the lesion with 0.035″ hydrophilic guidewires. Balloon dilatations were applied to the diseased artery segments in which hemodynamically significant stenosis/occlusion was observed, in accordance with the size of the lesion, atherectomy (especially in long segment occlusive lesions with more dense calcification) and self-expandable stent implantation procedures (in cases of hemodynamically significant stenosis or dissection secondary to the procedure) were performed according to the characteristics of the lesion and the effectiveness of the procedure. When more than one stent implantation was required, stents were implanted by overlap technique. When primary stenting was planned, predilatation was performed first and postdilatation was performed if adequate patency was not achieved after stenting. Finally, postprocedural imaging was performed to ensure adequate flow and to assess whether any extravasation, distal embolism, or dissection had occurred.
The introducers in the popliteal region of the patients were removed as soon as the patient was admitted to the ward bed, and after approximately 10 min of manual compression, they were followed up with sandbagging for approximately 6 h. Each patient was advised to take lifelong antiplatelet therapy (including two antiplatelet therapies containing ASA and clopidogrel for 2 months) after the procedure. Patients were called for routine follow-up in the 1st week, and 1st and 3rd month after the procedure for the status of their complaints, physical examination findings, and Doppler ultrasound examination when necessary.
The technical success of the procedure was defined as crossing the SFA lesion with a guidewire and entering the true lumen with less than 30% stenosis remaining after the procedure. Thromboembolism, extravasation, hematoma, pseudoaneurysm, amputation, and death were considered adverse events.
Statistical analysis
Continuous variables were expressed as median and range. Categorical variables were compared using the χ2 test and Fisher’s exact test where appropriate. Continuous variables with normal distribution were compared using the independent samples T test. Non-parametric data were compared using the Mann-Whitney U test. A p-value ≤ 0.05 was considered statistically significant.
Results
We evaluated 45 peripheral endovascular procedures performed on 39 patients with a mean age of 62.49 ±11.38 years in the Cardiovascular Surgery Department of our hospital on different dates for chronic occlusive FPA disease. Thirty-eight (84.4%) of the patients who underwent peripheral endovascular procedures had diabetes mellitus (DM) in the study. Twelve (26.7%) of the endovascular treatment procedures were performed with retrograde access through the popliteal artery (Retrograde Group). Among the patients in our study, in the Retrograde Group, 11 (91.6%) patients had a GLASS 2-3 class lesion, while this number was 29 (87.8%) in the Antegrade Group. However, the number of patients with Trans-Atlantic Inter-Society Consensus (TASC) II class C-D lesions was 9 (75%) in the Retrograde Group, while this number was 10 (30.3%) in the Antegrade Group. The demographic data of the groups and data about the procedure are presented in Table I.
Table I
Demographic characteristics of the groups
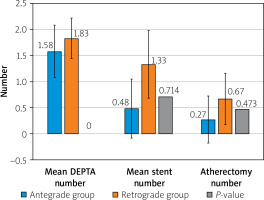
In neither group were any complications of arterial rupture, distal embolism, early thrombosis, or pseudoaneurysms observed, and the success and complications are summarized in Table II. While no stent was used in 1 patient in the Antegrade Group, no stent was used in 5 patients in the Retrograde Group. The materials used in the endovascular treatment procedure with both accesses are shown in Figure 1. In the Antegrade Group, the CFA was explored at the 4th hour after the procedure in 1 patient who had a hematoma and decreased hemoglobin level at the intervention site (inguinal region) in the post-procedure period, and the arterial defect was repaired primarily and the patient was discharged on the 6th post-procedure day. No mortality or major amputation was detected in any patient whose study data were evaluated during the study period. During the follow-up period after the procedure, the walking distance increased in all patients. The mean follow-up period of the patients during the study period was 2.11 ±1.13 months (1 to 6 months).
Table II
Success rates and complication development data of groups
Discussion
Symptomatic PAD is typically observed in SFA as diffuse and complex lesions or occlusions, and it has been well documented that the disease and its adverse outcomes are on the rise as life expectancy, and the incidence of diseases such as diabetes mellitus and obesity in the etiology, are increasing [12, 13]. It has been reported that the femoropopliteal segment is affected in a significant portion of the patients with PAD and that these lesions tend to be diffuse and severe [14, 15] and most of these are TASC-II class C and D [3]. While peripheral arterial bypass grafting is often considered the best treatment modality for symptomatic PAD, it is also associated with significant morbidity [13]. Meanwhile, with the advancement of new techniques and devices for endovascular interventions [16], endovascular treatment has ultimately become recognized as the primary option for many patients with PAD [17]. It is reported that a new anatomical scheme which is named GLASS for the threatened limb is proposed in the GVG and it incorporates two new and important concepts: the target arterial tract and estimated limb-based patency. In the GVG, the severity of the disease was classified by the WIfI score and the primary treatment options of the disease were expressed by considering the WIfI score and GLASS anatomical classification (1-4) together [6]. The mean GLASS class of the patients in our study was determined as 2.31 ±0.66, while there were 11 (91.6%) patients in the Retrograde Group with a lesion in GLASS class 2-3, and 29 (87.8%) patients in the Antegrade Group. However, 84.4% of the patients in our study had DM, and ankle-brachial index (ABI) values were not recorded and evaluated in the study due to possible errors that may occur in ABI measurement in the presence of DM and severe calcifications.
Although the standard access route for endovascular revascularization of SFA occlusive disease is antegrade intervention via the femoral arteries (contralateral or ipsilateral) [12], the ipsilateral approach has been reported to be challenging, notably in obese patients and patients with proximal SFA lesions. It has also been demonstrated that the contralateral antegrade approach complicates the technique in patients with narrow iliac bifurcation [15]. Incidents of antegrade failure have been reported in 2 to 20% of cases, but these cases are usually associated with failures of passage in lesions requiring subintimal recanalization or failed reentry into the true lumen [18]. Additionally, it has been noted that re-occlusion is a significant risk, particularly with long subintimal passes, and although special devices have been developed for such lesions, their use has been limited [12, 19, 20].
Over time, there have been developments in the intervention technique and efforts have been made to increase the chances of endovascular revascularization of occlusive arterial lesions from different access locations, and it has been reported that the RPA technique is a safe and effective access option to improve the success rates of percutaneous transluminal arterial procedures in failed antegrade interventions [12, 21] and allows successful revascularization in approximately 85-95% of patients [14]. Although failed antegrade attempts have been reported as the main indication for retrograde access, CFA stenosis/occlusion, short SFA stump (< 5 mm), long segment occlusions, tandem lesions, obesity, and previous inguinal surgery are other indications [3, 22, 23]. In later anatomical and radiological studies of the RPA technique, high success rates and low complication rates were reported, although it was not widely used due to the high complication rates and difficulties in accessing the intervention site when it was first introduced 30 years ago, as well as difficulties in accessing the intervention site [12, 14, 24, 25]. In our study 42.2% of lesions were in TASC II class C-D and in the Retrograde Group the TASC II class C-D lesion rate was found to be 75%, which was higher than in the Antegrade Group (30.3%). Similarly, in Retrograde Group patients of our study, we preferred the RPA technique due to anatomical incompatibility, long segment SFA occlusions, short SFA stump, and failed antegrade interventions.
It has been stated that carefully performed PA puncture is safe in the absence of disease in the popliteal segment [12, 14, 26] and technically, popliteal access can be performed under the guidance of fluoroscopy or ultrasound and in the prone or side-lying position [23]. Also, there are studies stating that the ultrasound-guided RPA technique results in a high technical success rate without complications. It has been stated in some publications that technical success, defined as entering the PA under DUS guidance and performing SFA recanalization, occurred in all patients. Another study reported that endoluminal recanalization was accomplished in the majority of patients through popliteal access (n = 26), while SFA recanalization was only achieved in 2 cases by using subintimal access [3]. In our study, we used the technique of performing an intervention in the prone position and with ultrasound guidance in the entire group of RPA patients, and although not included in the study, in 1 of 13 interventions with this technique, the PA lumen could not be entered and passed due to diffuse popliteal disease. All Retrograde Group patients (n = 12) were able to undergo endoluminal revascularization (without subintimal passage), and no regional complications occurred as a result of the intervention.
In general, it is reported in the literature that retrograde intervention techniques are successful at a rate of 67% to 100%, that each center uses techniques according to its experience since there is no standard protocol, and that this affects success rates [14, 27]. It is also stated that RPA access has some advantages related to stenosis morphology, that it is associated with a lower rate of subintimal transition, that the distance between the point of intervention and the occluded segment is shorter, and thus the pushability is higher [27].
In a study reporting 93 patients who underwent endovascular revascularization with the RPA technique, it was reported that balloon dilatation failed in 7.53% of the cases and femoropopliteal bypass grafting was performed in these cases [14]. In our study, none of the 12 patients who underwent endovascular revascularization with the RPA technique required early femoropopliteal bypass grafting. Moreover, no significant difference was found between the two groups in this regard. We think that the reason for this is that we use the retrograde intervention technique in cases that we think are not suitable for antegrade intervention or we cannot perform endovascular revascularization with antegrade intervention. There are publications reporting a patency rate of 100% at the 1st month after the procedure in patients who underwent revascularization with the same method [3]. In another study of 16 patients who underwent endovascular revascularization with the RPA technique for occlusive SFA disease, it was reported that the access was successful in all cases, the success rate was 94%, one uncomplicated perforation occurred, the limb salvage rate was 100%, and no local site complications occurred [28]. Consistent with the literature, in our study, 100% lesion crossing success was achieved (via the endoluminal route) with the RPA technique, and successful endovascular revascularization was performed in all cases with a lesion crossing and no access site complications occurred. However, although there was no significant difference between the two groups in terms of endovascular revascularization rates, hematoma-bleeding occurred in the early post-procedure period in 1 patient in the Antegrade Group as an access site complication, and the patient underwent exploration + CFA repair in the 4th hour after the procedure. The early limb salvage rate was 100% in all patients in our study, including the RPA group, and minor amputation was performed in 1 patient in the Retrograde Group. This patient had Fontaine stage 4 and a gangrenous toe lesion before the procedure. It has also been reported in the literature that in addition to balloon angioplasty in cases of endovascular revascularization using the RPA technique, stent implantation was required in 71.4% of cases, and atherectomy was required in 5.3% of cases [12, 26] and the rate of stent implantation was reported as 94.5% in another publication [13, 14]. Also, in our study, the need for stent implantation in addition to balloon angioplasty was 91.6% and the rate of atherectomy was 66.6% in the RPA group. When evaluated in terms of the number of stents implanted between the two groups in our study, no significant difference was found, but there was a higher rate of stent implantation in the RPA group (Antegrade Group = 45.4%, Retrograde Group = 91.6%), which may be due to the longer and calcific lesions in the RPA group or the dissections that developed. Although there was no numerical difference in terms of the number of stents implanted, the mean number of stents implanted per patient was 1.33 ±0.65 in the Retrograde Group and 0.48 ±0.56 in the Antegrade Group. The use of stents in patients revascularized with the RPA technique was similar to the literature, and atherectomy was more prevalent in the RPA group (66.6%) than in the literature and the Antegrade Group (27.2%). We believe that this is due to the fact that patients in the RPA group had longer segment occlusions and more complex lesions that were more calcified.
In one of the comparative studies conducted between non-RPA and RPA techniques in the literature, it was stated that in 91 patients who underwent endovascular revascularization due to chronic total occlusion of SFA, there was more HT in the RPA group, and primary success rates were better (97.2% in the RPA group and 78.2% in the non-RPA group) despite more long segment occlusion and the puncture location, and major and total complication rates were similar [14, 24]. However, in another study performed on 148 patients, it was reported that endovascular revascularization with RPA had a significantly lower technical success rate (80.4% in the RPA group and 93.8% in the CFA group), the rates of major extremity preservation were lower in endovascular revascularization with RPA (74.5% in the RPA group and 83.5% in the CFA group) and patency rates were reported to be 70.3% in the CFA group and 83.1% in the RPA group [14, 29]. Meanwhile, in a multivariate analysis, the RPA technique was an independent factor in primary patency loss, and RPA and CFA access had similar complication rates [18]. Again, complication rates have been reported between 2.5% and 5.2%, and one study reported that no early or late complication was detected [14]. Likewise, in our study, although the rates of successful revascularization and patency and post-procedure limb preservation were similar in the two groups, the rates of complications such as dissection and bleeding secondary to the procedure were lower in the RPA group (dissection: Antegrade Group = 21%, Retrograde Group = 8%, and bleeding: Antegrade Group = 3%, Retrograde Group = 0%).
Our study has limitations such as being a single-center study with a retrospective design, a relatively small number of patients, and a short follow-up period, complete lack of 1-year follow-up and no ABI comparison before and after the procedure, and the decision to use the RPA technique depends on the vascular surgeon performing the procedure.