Introduction
Vitiligo is an acquired disorder characterized by the progressive loss of functional melanocytes, resulting in depigmented macules and patches on the skin [1]. It affects a significant portion of the world’s population, with no specific gender or geographic predilection [2]. The onset of vitiligo can occur at any age, but it is most commonly seen between 20 and 30 years old [3]. Although up to 30% of vitiligo patients may have a family history of the condition, its inheritance pattern is complex and multifactorial [4]. The clinical presentation of vitiligo can be classified into different types, including segmental vitiligo, characterized by unilateral macules in a segmental or band-shaped distribution, and non-segmental vitiligo, characterized by bilateral macules with an acrofacial or scattered symmetric pattern [2]. Another classification scheme involves localized and generalized types, with further subcategories based on the extent and distribution of the depigmented lesions [5, 6]. While the exact cause of vitiligo remains unknown, various theories have been proposed. The autoimmune hypothesis suggests an association between vitiligo and other autoimmune disorders as patients often have comorbidities such as thyroid disease, diabetes mellitus, and alopecia areata [7]. Other potential mechanisms include oxidative stress, immune system dysfunction, cytotoxic T-cell-mediated melanocyte destruction, neurogenic factors, and genetic susceptibility [8, 9]. However, further research is necessary to fully comprehend the underlying pathogenesis. Diagnosis of vitiligo primarily relies on the clinical presentation of depigmented macules and their distribution. Wood’s lamp examination can be helpful, particularly in individuals with lighter skin tones, for visualizing hypopigmented areas [10]. Treatment options for vitiligo aim to restore melanocytes to the affected skin areas. Topical agents such as potent corticosteroids or topical calcineurin inhibitors are often the first-line treatment as they can induce repigmentation and halt disease progression [11]. Systemic therapies like psoralen plus ultraviolet A (PUVA) or narrowband ultraviolet B (NB-UVB) phototherapy can be effective for certain patients [12]. Excimer laser treatment, combined with topical calcineurin inhibitors or corticosteroids, has shown promising results in improving vitiligo lesions, particularly on the face [13]. Topical tacrolimus, a calcineurin inhibitor, has also been utilized in vitiligo treatment by modulating the immune response and potentially promoting melanocyte growth and migration [14]. Amid the COVID-19 pandemic caused by the SARS-CoV-2 virus, extensive research has focused on various aspects of the disease. While the primary emphasis has been on respiratory symptoms and complications, emerging evidence suggests potential associations between COVID-19 and dermatological conditions. One such condition of interest is vitiligo, a chronic autoimmune disorder characterized by depigmented patches on the skin.
Aim
This article aims to explore the current understanding of the association between vitiligo and COVID-19.
Material and methods
This was a cross-sectional comparative study of 90 patients with vitiligo, with the patients divided into 2 groups: one group having vitiligo and infected by COVID-19 confirmed by PCR, and the other group not infected by COVID-19 collected previously in 2018 (before the COVID-19 pandemic). The data were collected from March 2021 To May 2022 at Al-Sadar teaching hospital, in Al Basra province. Inclusion criteria: all patients with vitiligo, while excluding any patients having vitiligo and another infection. Wood’s test was used to confirm the diagnosis of vitiligo (VASI score).
Statistical analysis
The data collected for all patients in both groups were: age (years), gender, site of vitiligo, no. of lesions, and family history of vitiligo. Utilizing SPSS 22, frequency and percentage were utilized for categorical data, while mean and standard deviation were utilized for continuous data. The χ2 was used to evaluate the relationship between categorical variables.
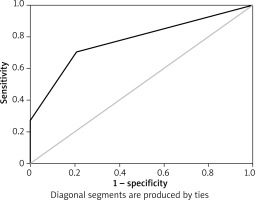
The T test was used to assess differences between the mean and median of continuous variables. ROC curve was also used to demonstrate a more sensitive and specific cutoff point. P-value less or equal to 0.05 was considered significant.
Results
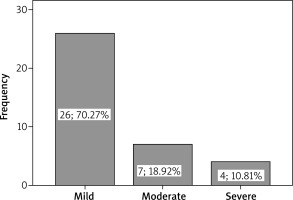
As shown in Figure 1, in the patients having vitiligo and COVID-19 infection, the severity of infection was the following; 70.27% – mild infection, 18.92% – moderate infection and 10.81% – severe infection.
There is a significant difference in mean age, duration and VASI score according to both groups of study, the age of patients with vitiligo+COVID-19 was lower than the age of patients who have vitiligo only. VASI in patients having vitiligo + COVID-19 was also lower than patients having vitiligo only as shown in Table 1.
Table 1
Differences in mean age, duration and VASI score according in both groups
| Variables | Group | N | Mean | Std. deviation | P-value |
|---|---|---|---|---|---|
| Age [years] | With | 37 | 18.57 | 17.22 | 0.045 |
| Without | 53 | 24.75 | 11.62 | ||
| VASI | With | 37 | 71.62 | 25.79 | 0.0001 |
| Without | 53 | 94.81 | 10.23 |
As shown in Table 2, there is a significant association between gender, site, lesion number in both groups: more females (60.6%) had vitiligo and were infected with COVID-19. Also most common site of vitiligo in patients with COVID-19 infection was lower limbs (66.7%) and then head and neck (55.3%). While 100% of patients had vitiligo and COVID-19 infection, they had five, seven and eight lesions. There was no significant association between family history in both groups.
Table 2
Association between gender, site, lesion number in both groups
According to Figure 2 and Table 3, as shown in ROC curve, more sensitive and specific cutoff point of VASI score in patients having vitiligo and infected with COVID-19 was 87.5 (70% sensitivity, 80% specificity).
Discussion
The relationship between vitiligo and COVID-19 is an emerging area of research, and several studies have investigated the potential association between these two conditions. However, there is limited specific research on this topic. Immune dysregulation: Both vitiligo and COVID-19 involve immune dysregulation. COVID-19 is known to cause an immune response and nflammation, which can potentially act as a trigger for vitiligo flares or new-onset cases [14]. Psychological Impact: The psychological impact of the COVID-19 pandemic, including stress and anxiety, can influence the course of autoimmune diseases like vitiligo. Psychological stress has been associated with the onset and exacerbation of vitiligo [15]. The pandemic-induced stress may have a similar effect on vitiligo. There is limited research currently available on the specific relationship between vitiligo and COVID-19 severity. However, a few studies have investigated the association between autoimmune disorders and COVID-19 severity, which may provide some insight. In a retrospective study conducted in Wuhan, China, it was found that patients with autoimmune diseases were at a higher risk of developing severe COVID-19 and requiring intensive care unit (ICU) admission [16]. Similarly, a systematic review and meta-analysis of 17 studies found that patients with autoimmune diseases were at an increased risk of contracting a severe form of COVID-19 [16, 17]. However, another study found no association between systemic autoimmune diseases, including vitiligo, and COVID-19 severity or mortality [18]. The study included 160 patients with autoimmune diseases and COVID-19; 33 patients had vitiligo. The severity of COVID-19 was determined based on clinical and laboratory data, and the study found that the majority of patients experienced mild COVID-19 symptoms. Vitiligo is a chronic skin disorder characterized by depigmented patches on the skin due to the destruction of melanocytes. COVID-19 is a novel infectious disease caused by the SARS-CoV-2 virus that has affected millions of people worldwide. The co-occurrence of vitiligo and COVID-19 has been reported in several studies, and there is evidence to suggest that there is a significant difference in age, duration, and VASI score between patients with vitiligo + COVID-19 and those with vitiligo only. Several studies have investigated the relationship between COVID-19 and vitiligo. In a study conducted by Salama and colleagues, they reported that the prevalence of vitiligo in COVID-19 patients was significantly higher than in the control group. In addition, they found that the mean age of COVID-19 patients with vitiligo was significantly lower than those without vitiligo [19]. This finding is consistent with other studies that have reported a higher prevalence of COVID-19 in younger patients with vitiligo [20]. The duration of vitiligo appearance is also an important factor that has been studied in relation to COVID-19. A study by Chatterjee et al. found that the duration of vitiligo appearance was significantly shorter in COVID-19 patients with vitiligo than in those without vitiligo. This may suggest that COVID-19 may accelerate the progression of vitiligo or that patients with a shorter duration of vitiligo may be more susceptible to COVID-19 [21]. The VASI (Vitiligo Area Scoring Index) score is a measure of the extent and severity of vitiligo. A study by Tsai et al. reported that the VASI score was significantly lower in COVID-19 patients with vitiligo than in those without vitiligo. This finding may suggest that COVID-19 may have a protective effect on vitiligo or that patients with less severe vitiligo may be more susceptible to COVID-19 [22]. While there are several studies that have reported a significant difference in age, duration, and VASI score between patients with vitiligo+COVID-19 and those with vitiligo only, there are also studies that have reported conflicting results. For example, a study by Li et al. found no significant difference in age, duration, or VASI score between COVID-19 patients with vitiligo and those without vitiligo [23]. Similarly, a study by Christensen et al. reported no significant difference in the prevalence of vitiligo between COVID-19 patients and the general population [24]. The presented findings suggest that there is a significant association between gender, site, lesion number, and the presence of both vitiligo and COVID-19 infection. Specifically, the data reveal that a higher proportion of females (60.6%) with vitiligo are infected with COVID-19. Moreover, the majority of patients with both conditions have vitiligo lesions on their lower limbs (66.7%), followed by the head and neck (55.3%). Additionally, it was observed that patients with both vitiligo and COVID-19 infection had five, seven, or eight lesions. These results are consistent with some studies that have suggested that females may be more vulnerable to COVID-19 infection than males due to differences in immune response and hormonal factors [25]. Furthermore, other studies have demonstrated a higher prevalence of COVID-19 infection in individuals with underlying autoimmune conditions, such as vitiligo [26]. The observation that the lower limbs are the most common site of vitiligo lesions in patients with COVID-19 infection may be due to the fact that the virus primarily affects the respiratory system, which is supplied by blood vessels in the lower extremities [27]. However, these findings contradict some studies that have reported no significant association between gender and COVID-19 infection [28]. Additionally, while the association between vitiligo and COVID-19 infection has been noted in some studies, others have reported no such association [29]. Moreover, the lack of a significant association between family history and both conditions is inconsistent with some studies that have suggested a genetic predisposition to COVID-19 infection [30] and vitiligo [31]. It is important to note that the presented results are based on a single study and should be interpreted with caution. Further research is needed to confirm these findings and to explore the underlying mechanisms that may contribute to the observed associations. Additionally, the sample size of the study is not mentioned, which could impact the generalizability of the results. To summarize, the presented findings suggest a significant association between gender, site, and lesion number, and the presence of both vitiligo and COVID-19 infection. While some studies support these findings, others do not. More research is needed to confirm these results and to elucidate the underlying mechanisms that may contribute to the observed associations.
Conclusions
The study observed patients with both vitiligo and COVID-19 infections and found that 70.27% had a mild infection, 18.92% had a moderate infection, and 10.81% had a severe infection. Patients with both conditions were younger, had a shorter duration of vitiligo, and had a lower VASI score than patients with vitiligo only. Females were more likely to have both conditions, and the lower limbs were the most common site for vitiligo in these patients. There was no significant association between family history in both groups.