Summary
The study aimed to evaluate the performance of the PRECISE-DAPT score in predicting long-term prognosis in atrial fibrillation (AF) patients with non-ST-elevation myocardial infarction (NSTEMI). A total of 526 AF patients were included in the study, and all-cause mortality occurred in 52.6% of them. A higher PRECISE-DAPT score, shorter duration of P2Y12 inhibitor therapy, decreased left ventricular ejection fraction, and a history of diabetes mellitus were associated with increased all-cause mortality in the multivariate logistic regression model. The study concluded that a high PRECISE-DAPT score was associated with higher long-term all-cause mortality in AF patients presenting with NSTEMI.
Introduction
Atrial fibrillation (AF) is a common and persistent arrhythmia in adults that can lead to substantial mortality and morbidity [1, 2]. The management of AF has evolved, with a shift away from attempts to prevent recurrence and toward control of the heart rate [3–6].
However, maintaining a normal heart rhythm may be beneficial in preventing severe cardiovascular events and may be necessary for patients with prominent symptoms of AF [7, 8]. Moreover, sinus rhythm maintenance has been associated with reductions in death and cardiovascular events [9, 10].
AF and non-ST-elevation myocardial infarction (NSTEMI) may accompany each other. In patients with NSTEMI, AF is associated with an increased short-term mortality difference among the predefined types of AF [11]. Poçi et al. reported that any AF associated with acute coronary syndrome (ACS) almost doubled the long-term mortality risk [12].
Regardless of its presentation, AF should be recognized as a noteworthy risk factor in patients with NSTEMI, given the well-established influence of clinical risk factors such as previous or new heart failure, hypertension, diabetes, stroke, and age on risk assessment and prognosis. As it is crucial to determine which ACS patients will have a poor long-term prognosis, early risk stratification has the utmost importance in predicting outcomes in AF patients presenting with NSTEMI. The PRECISE-DAPT score, which predicts bleeding risk in patients undergoing stent implantation and subsequent dual antiplatelet therapy (DAPT), was developed to predict bleeding risk in patients treated with DAPT after percutaneous coronary intervention (PCI). This score is calculated by five parameters (age, white blood cell count, hemoglobin level, creatinine clearance, and history of spontaneous bleeding) and patients with a score of > 25 are deemed to have a high risk of bleeding [13]. The current guidelines recommend using the PRECISE-DAPT score for bleeding risk stratification, and a score of > 25 indicates that the DAPT period should be shorter than 3 to 6 months in patients with a score of < 25 [14–16]. In a recent study, a high PRECISE-DAPT score was associated with higher long-term all-cause mortality in patients with acute myocardial infarction (AMI) [17, 18].
Aim
Thus, the aim of the present study is to assess the performance of the PRECISE-DAPT score in predicting the long-term prognosis in AF patients presenting with NSTEMI.
Material and methods
This is a retrospective, observational study consisting of 526 consecutive AF patients presenting with NSTEMI who were discharged from a high-volume single center between April 2013 and December 2022. NSTEMI was diagnosed according to the ESC NSTEMI guidelines, and AF was classified as either persistent or permanent, or paroxysmal. New-onset AF was not included in the study. New-onset AF was defined as AF that was first detected upon admission or during hospitalization. The absence of AF was defined as no prior history or detection of AF during admission or hospitalization.
The PRECISE-DAPT score, age, creatinine clearance, white blood cell count, hemoglobin, and previous bleeding history were calculated for each case using a web calculator (http://www.precisedaptscore.com). Clinical, biochemical, interventional, ECG, and transthoracic echocardiography data were obtained from the hospital’s electronic data set. Echocardiography was performed to determine left ventricular ejection fraction (LVEF). All patients underwent emergency PCI. The decision regarding the treatment of non-IRA lesions (medical follow-up, single or multi-stage procedures) was at the discretion of the relevant physician. All patients were prescribed medications, including the initiation and duration of dual antiplatelet therapy and anticoagulation therapy, at the discretion of the relevant physician upon discharge. In our study, physicians have the option to prescribe dual antiplatelet and anticoagulant therapies based on the guidelines of the European Society of Cardiology (ESC) for AF in the patient population ranging from 2013 to the present. For patients up to 2016, the recommendations for dual antiplatelet and anticoagulant therapies from the ESC 2010 AF guidelines were followed, while for patients after 2016, the recommendations from the ESC 2016 AF guidelines were utilized. Patients who were on ticagrelor and prasugrel and patients treated with complex PCI such as bifurcation and chronic total occlusion stenting were excluded from the study. Also, patients with a history of previous severe thrombocytopenia, chronic bleeding diathesis, cirrhosis with chronic bleeding, cirrhosis accompanied by portal hypertension, active malignancy and intracranial bleeding were excluded from the study. Patients received triple therapy up to the sixth month, followed by single antiplatelet therapy (acetylsalicylic acid or clopidogrel, based on physician preference) and warfarin treatment according to the 2010 AF guidelines or any new generation oral anticoagulant according to the 2016 AF guidelines from the sixth to the twelfth month. After the twelfth month, patients received warfarin treatment according to the 2010 AF guidelines, or any new generation oral anticoagulant according to the 2016 AF guidelines.
Patient follow-up for all-cause mortality continued until December 2022, with the death status and/or date of death acquired through meticulous retrieval from the patients’ medical records, consultation with the respective attending physicians, or by means of telephone communication with the patients. The study design received approval from the local ethical committee and adhered to the principles outlined in the Helsinki Declaration.
Statistical analysis
The data were analyzed using SPSS software (Version 23.0, SPSS, Inc.). The normality of continuous variables was evaluated. This evaluation included visually inspecting the distribution (histograms, probability plots) and using analytical methods (Kolmogorov-Smirnov/Shapiro-Wilk’s test). Levene’s test was performed to evaluate homogeneity. Continuous variables were expressed as mean ± standard deviation in the table, while categorical variables were given as percentages. The difference in categorical variables between groups was evaluated using the χ2 or Fisher’s exact test (when the χ2 test assumptions were not valid due to low expected cell counts). Means of parameters showing normal distribution were compared using the one-way ANOVA test. Univariate analysis was performed to compare the groups with (+) and without (–) mortality. Parameters showing a statistically significant difference (p < 0.05) in the mortality (+) group were first evaluated by univariate Cox logistic regression analysis. Using the parameters that were significant in this analysis, a multivariable Cox regression analysis (enter method) was performed. In the multivariable analysis, the 95% confidence interval range was observed. Then, the sensitivity and specificity of the factors that independently predicted the mortality (+) group were calculated by ROC analysis. The value at which the PRECISE-DAPT score showed the highest sensitivity and specificity was taken as the cut-off value, and long-term survival was compared by Kaplan-Meier analysis.
Results
A total of 212 (40.3%) women and 314 (59.7%) men, with a mean age of 65.2 ±12.7, were included in the study. The median follow-up period was 5.3 (3.8–7.2) years. Mortality was identified in 278 (52.6%) of the patients. The patients were divided into two groups, mortality (–) and mortality (+), and were subjected to univariate analysis (Table I). In the mortality (+) group, there were higher rates of diabetes mellitus, history of hypertension, increased PRECISE-DAPT score and white blood cell count at presentation. Additionally, there were higher rates of in-hospital drug-eluting stents (DES) and P2Y12 inhibitor use for more than 1 year, lower rates of prescription of angiotensin-converting enzyme (ACE) inhibitors (ACEI)/angiotensin receptor blockers (ARBs), and statins at discharge, lower eGFR and hemoglobin levels, and lower LVEF levels.
Table I
Clinical and demographic characteristics of patients with or without mortality during the follow-up period
[i] ACEI/ARB – angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, ASA – acetylsalicylic acid, BB – β-blocker, BMI – body mass index, CABG – coronary artery by-pass grafting, CAD – coronary artery disease, CCB – calcium channel blocker, CHF – congestive heart failure, COPD – chronic obstructive pulmonary disease, CX – circumflex artery, CVA – cerebro-vascular accident, DES – drug-eluting stent, DM – diabetes mellitus, HT – hypertension, INR – international normalized ratio, LAD – left anterior descending artery, LVEF – left ventricular ejection fraction, NOAC – non-vitamin K antagonist oral anticoagulants, PAD – peripheric artery disease, PCI – percutaneous intervention, PPI – proton pump inhibitors, RCA – right coronary artery, SD – standard deviation, WBC – white blood cells.
When parameters with statistically significant differences between the two groups were evaluated by univariate Cox regression analysis, diabetes mellitus history, statin, ACEI/ARB use, DES implantation, P2Y12 inhibitor duration, eGFR values, hemoglobin levels and LVEF were the factors that remained significant. Applying these parameters to a multivariable Cox regression analysis (enter method), diabetes mellitus (HR = 1.359, 95% CI: 1.055–1.750; p = 0.018), P2Y12 inhibitor duration (HR = 0.394, 95% CI: 0.301–0.516; p < 0.001), PRECISE-DAPT score (HR = 1.026, 95% CI: 1.010–1.042; p = 0.001), and in-hospital LVEF levels (HR = 0.976, 95% CI: 0.966–0.986; p < 0.001) were found to be independent predictors of long-term all-cause mortality (Table II).
Table II
Univariate and multivariable Cox proportional regression analysis results of groups with and without mortality during the follow-up period
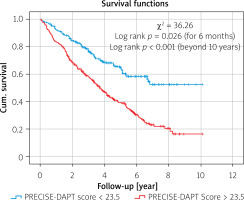
We evaluated the sensitivity and specificity of the independent predictors of mortality using ROC analysis (Figure 1). The AUC level of the PRECISE-DAPT score was 0.706 (p < 0.001). When the PRECISE-DAPT score was > 18.5, the sensitivity was 80.6%, the specificity was 50.5%, the positive predictive value was 62.3%, and the negative predictive value was 71%. These values were 72.2%, 59.7%, 69.5%, and 77.5%, respectively, when the PRECISE-DAPT score was > 23.5. We used the 23.5% cut-off value to evaluate the first 6-month and long-term survival by Kaplan-Meier analysis (Figure 2), which resulted in a χ2 of 36.26, first-month p = 0.026, and log-rank p < 0.001. The mortality rate between groups was observed to differ from the first 6 months of the follow-up periods.
Discussion
In this study, we found that a high PRECISE-DAPT score is a significant independent predictor of long-term mortality in AF patients presenting with NSTEMI. To the best of our knowledge, this is the first study reporting that long-term mortality is significantly higher in AF patients presenting with NSTEMI and a high PRECISE-DAPT score, regardless of co-morbidities, coronary artery lesions, revascularization procedures, or medications at discharge. Furthermore, a shorter duration of P2Y12 inhibitor therapy, decreased LVEF, and a history of diabetes mellitus (DM) were all associated with an increased risk of all-cause mortality after adjusting for other factors.
In individuals with AF, various prognostic factors have been identified that can affect long-term outcomes. These include comorbidities such as diabetes mellitus, a history of heart failure, myocardial infarction, and demographic and clinical baseline characteristics such as age, smoking, and low ejection fraction [19–21]. Moreover, AF can lead to ACS and bring a deterioration of cardiac function and an increased risk of complications such as congestive heart failure, stroke, and ventricular arrhythmias [22]. A study by Poçi et al. found that patients with persistent or permanent AF have a poorer prognosis than other forms of AF following an ACS event. However, no significant differences were observed in long-term follow-up [12]. The study also reported that more than half of patients with any AF died within 10 years [12]. Our research also demonstrated similar long-term mortality rates. However, no parameter can accurately determine which patients are at higher risk for long-term outcomes.
While the assessment of risks in clinical practice can be intricate and challenging, the utilization of simplified risk scoring systems may offer greater practicality. The PRECISE-DAPT score serves as a readily calculable tool that enables swift risk classification without incurring additional costs. Although originally developed for predicting bleeding risk in patients undergoing DAPT after PCI, the PRECISE-DAPT score does not specifically encompass long-term mortality prediction. Nevertheless, several studies have revealed compelling associations between the PRECISE-DAPT score and cardiovascular events. Notably, Long et al. found an independent correlation between the PRECISE-DAPT score and the severity of coronary stenosis in individuals with ACS [23]. Furthermore, in patients with ST-elevation myocardial infarction (STEMI), the PRECISE-DAPT score emerged as an independent predictor of in-hospital mortality following primary PCI [24]. Additionally, there have been reports indicating that a higher PRECISE-DAPT score is linked to the presence of AF [25].
In our study, we chose to include eGFR and hemoglobin as additional variables in the multivariate model, alongside the PRECISE-DAPT score, due to their potential impact on the outcomes of interest. Prior bleeding and WBC were not included in the multivariable analysis because they did not show a significant effect on mortality in the univariate analysis. These variables provide valuable information related to renal function and anemia, which have been recognized as important factors in cardiovascular disease and treatment response. By incorporating eGFR and hemoglobin into the model, we aimed to assess their independent contributions to the outcomes, while considering the comprehensive risk stratification provided by the PRECISE-DAPT score.
One of the reasons for including eGFR in the analysis is its established association with adverse cardiovascular events. Impaired renal function, as reflected by lower eGFR values, has been consistently linked to increased cardiovascular morbidity and mortality. Reduced eGFR is associated with heightened platelet activation, inflammation, oxidative stress, and endothelial dysfunction, which collectively contribute to a prothrombotic state and higher risk of adverse outcomes. Therefore, incorporating eGFR as a variable in the multivariate model allows us to evaluate its impact on the outcomes independently of the PRECISE-DAPT score, potentially providing additional insights into the relationship between renal function and the efficacy of DAPT.
Similarly, the inclusion of hemoglobin in our analysis is warranted due to its role as a marker of anemia, which has been associated with poor cardiovascular outcomes. Anemia can induce tissue hypoxia, leading to increased cardiac workload and impaired oxygen delivery, ultimately exacerbating myocardial ischemia and compromising overall cardiovascular health. Additionally, anemia is often related to comorbidities such as chronic kidney disease and inflammation, which can further impact platelet function and response to antiplatelet therapy. By including hemoglobin as a variable, we can assess the independent effect of anemia on the outcomes of interest, while considering its interplay with the PRECISE-DAPT score. Consequently, we included eGFR and hemoglobin as additional variables in the multivariate model, along with the PRECISE-DAPT score, to comprehensively assess their potential contributions to the outcomes of interest. Although eGFR and hemoglobin showed a significant association with mortality in the univariate analysis, their independent effects on mortality were not significant in the multivariable analysis. Nonetheless, their inclusion in the model is valuable for risk stratification and capturing shared underlying mechanisms.
Previous studies have also shown that decreased LVEF and a history of DM are independently associated with increased mortality [20, 21]. In our study, we compared the prognostic value of the PRECISE-DAPT score to these factors and found that the score had superior prognostic ability, as demonstrated by ROC analysis.
In patients with AF who have undergone PCI for NSTEMI, adding DAPT to anticoagulation increases the risk of bleeding. Therefore, it is important to carefully manage these patients with a focus on minimizing bleeding risk. Premature discontinuation or shorter duration of P2Y12 inhibitor therapy increases the incidence of stent-related complications, including stent thrombosis, which can cause acute myocardial infarction. A shortened P2Y12 duration impairs endothelialization after stent placement, potentially leading to delayed healing, persistent inflammation, and an increased risk of late stent thrombosis. Additionally, underlying patient characteristics, such as complex coronary artery disease or higher plaque burden, combined with inadequate platelet inhibition, further amplify mortality risk. It is important to consider the potential impact of treatment duration on mortality outcomes in our study [26, 27]. Although our study did not specifically analyze treatment duration as a variable, it warrants attention and should be evaluated in future research. The optimal duration of treatment for certain conditions, such as NSTEMI and AF, remains a topic of ongoing debate and investigation. Factors such as patient characteristics, comorbidities, bleeding risk, and clinical guidelines can influence the selection of treatment duration. One key aspect of this management is determining the optimal duration of DAPT, for which the PRECISE-DAPT score can be instrumental. Additionally, suppose the score can predict long-term outcomes in patients with AF after NSTEMI. In that case, it can provide personalized medical care, such as maintaining normal sinus rhythm. Recent studies have shown that maintaining normal sinus rhythm can lead to better outcomes in patients with AF [9, 10]. In short, the PRECISE-DAPT score helps determine the optimal duration of DAPT. It may also be promising to regulate the early treatment of high-risk patients, which can help reduce long-term mortality in AF patients with NSTEMI [28].
Although our study excluded patients with complex coronary interventions, it is important to recognize the impact of PCI complexity on treatment decisions. Complex coronary lesions, such as calcified or bifurcation lesions, present unique challenges and require careful consideration when selecting antiplatelet therapy and determining treatment durations. For patients with complex lesions, achieving optimal stent deployment and minimizing complications can be challenging. Tailoring antiplatelet therapy and treatment durations based on the complexity of the procedure is crucial [29, 30].
Bleeding scores, such as the PRECISE-DAPT score used in our study, have shown utility beyond PCI. They can be valuable in risk stratification and treatment decision-making for other cardiovascular diseases and acute coronary syndromes without PCI. These scores have been associated with adverse outcomes and can guide the selection of antiplatelet regimens in different treatment modalities [31, 32].
This study has several limitations. Firstly, the study design was single-center and retrospective, which inherently introduces the potential for bias and confounding factors. The lack of randomization and the reliance on medical records for data collection may have influenced the results. Therefore, caution should be exercised in interpreting the findings, as they may not be applicable to other populations or healthcare settings. Secondly, it was conducted at a single tertiary center. Thirdly, while consecutive patients were enrolled, there may be a selection bias. Finally, another important limitation of this study is the potential influence of changes in clinical guidelines over the study period. The study spanned nearly a decade, from 2013 to 2022, during which significant updates and revisions in clinical guidelines for the management of NSTEMI and AF were implemented. These changes might have affected the consistency and validity of the study outcomes. Variations in treatment strategies, diagnostic criteria, and risk stratification approaches could have influenced patient management and outcomes over time. Therefore, it is crucial to consider that the results of this study are reflective of the clinical practices and guidelines in effect during the study period.
Conclusions
In patients with AF and NSTEMI, an elevated PRECISE-DAPT score demonstrated a significant association with increased long-term all-cause mortality. Consequently, the utilization of the PRECISE-DAPT score not only aids in identifying individuals at high risk of bleeding but also provides valuable prognostic information regarding unfavorable long-term outcomes during follow-up.