Introduction
In the early stages of development, lung cancer first manifests in the form of pulmonary nodules (PNs) [1–3]. The advent of extensive low-dose computed tomography (CT)-based screening strategies has led to a marked increase in the rate of stage I lung cancer development and a corresponding drop in cancer-associated mortality [4]. In subjects exhibiting PNs ≤ 8 mm in diameter, regular CT-based follow-up is recommended [5], whereas biopsy is recommended for all PNs larger than this size [5]. The diagnosis of PNs, however, is ultimately based on pathological diagnosis following surgical resection.
Video-assisted thoracoscopic surgery (VATS)-assisted wedge or segmental resection procedures have been widely utilized to diagnose PNs, as they allow for more limited resection such that the entirety of the PN can be removed while minimizing damage to the lungs [6–8]. These limited resection procedures can also achieve curative efficacy for lung tumors that have yet to become invasive [9]. Certain types of PNs including smaller nodules, deeper nodules, and ground glass nodules (GGNs), however, tend to be difficult to visualize or palpate during VATS procedures. In these cases, preoperative PN localization is required as a means of increasing the success rate of VATS-based limited resection procedures, minimizing the need for conversion to thoracotomy [10].
As it is quick, simple, and associated with a high success rate, CT-guided hook-wire (HW) localization is the most common strategy used in this context [11]. The HW approach, however, was developed for breast nodule localization [12], and its use for PN localization thus entails certain drawbacks. The rigid construction of the HW often subjects patients to discomfort. In addition, the HW can become dislodged when patients move or change position as it only includes a single hook at the distal end [11], with a 6% dislodgement rate having been reported in one recent meta-analysis [11]. In an effort to address these issues, anchored needle (AN) localization was developed as an alternative approach to identifying the locations of PNs [13]. Relative to HW localization, the AN approach entails a device with an anchor-like shape that consists of 4 claws rather than a hook, allowing for greater stability. AN approaches also utilize smooth sutures rather than steel wire when connecting the anchor, potentially improving post-localization comfort for patients [9]. However, there has been a lack of research assessing the relative clinical efficacy of HW- and AN-based PN localization.
Aim
The present study was thus designed to compare the safety and efficacy of preoperative CT-guided HW and AN localization strategies for patients with PNs.
Material and methods
This retrospective analysis was approved by both participating institutions, which waived the requirement for informed consent.
Patients
Between January 2020 and December 2021, consecutive patients with PNs who underwent preoperative CT-guided localization via a HW- or AN-based approach with subsequent VATS resection were included in this study. To be eligible for study inclusion, patients needed to exhibit: (a) PNs ≤ 30 mm in size; (b) PNs lacking a corresponding definite pathological diagnosis; and (c) PNs considered to exhibit a high risk of malignancy based on the Lung-RADS assessment [1]. Patients were excluded if: (1) the distance between the PN and the pleura was > 4 mm; (b) PNs were < 6 mm in size; (c) they exhibited typical metastatic PNs; or (d) they exhibited severe comorbidities.
CT-guided localization
Two radiologists with over 5 years of CT-guided interventional experience performed all procedures with a 16-row CT instrument (Siemens, Berlin, Germany) and the following settings: 120 kV, 150 mA, and 1 mm thickness. Patients were positioned as appropriate based on target PN locations, and the needle pathway was selected based on the shortest path between the skin and the target PN that avoided the ribs, lung bullae, and large blood vessels. Local anesthesia was used during all localization procedures.
HW localization was performed with a HW and a 21-gauge, 10-cm-long cannula (Argon Medical Devices, Inc, Athens, TX). Based on the chosen needle pathway, an introducer needle was inserted into the lung parenchyma, and repeated CT scanning was performed to confirm that the positioning and direction of the needle tip were correct. The needle tip was then maneuvered until it was within 1 cm of the target nodule, and the HW was released after confirming the needle tip position (Photos 1 A–C).
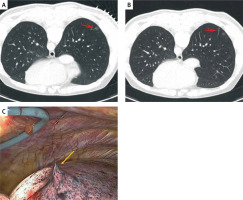
Photo 1
Procedures of CT-guided HW localization. A – CT image shows the GGN (arrow) at the right lower lobe. B – The HW (arrow) was placed near the GGN for localization. C – The HW (arrow) could be seen during the VATS procedures
AN localization was performed with an AN using a 20-gauge and 10- or 15-cm long cannula (Senscure, Ningbo, China). Needle punctures were performed in a manner identical to the approach used for HW localization. During AN placement, the removal of the safety buckle and the pressing of the pusher were performed to release the anchor into the lung parenchyma surrounding the target nodule. The needle was then withdrawn while leaving the tri-colored suture connected with the anchor remaining in the needle track. As the tri-colored suture length exceeded the distance between the tip of the needle and the pleura along the puncture path, the distal suture end remained outside of the pleura (Photos 2 A–C).
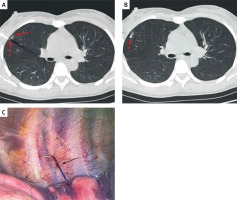
Photo 2
Procedures of CT-guided AN localization. A – CT image shows the needle tip (long arrow) placed near the GGN (short arrow). B – The anchor claw (arrow) was placed just beside the PN for localization. C – The tri-colored suture (arrow) could be seen during the VATS procedures
For patients with multiple PNs in need of localization, a one-stage CT-guided localization procedure was performed for all target nodules. All patients were evaluated via an additional CT scan to detect any localization-related complications.
VATS procedures
VATS-guided wedge or segmental resection was routinely performed within 3 h after localization under general anesthesia. During VATS procedures, surgeons were able to easily identify the localization markers and to palpate them with their fingers. Based on the distance between the target PN and the target localization marker on CT examination, surgeons were able to confirm the position of the target nodule. A cutting suture device was used to perform either wedge or segmental resection based upon the distance between the pleura and the target PN. Specifically, wedge resection was performed other than in cases with a margin of > 2 cm from the edge of the PN, in which case segmental resection was performed.
Resected PNs were sent to the Department of Pathology for rapid pathological examination. In cases where invasive lung cancer was diagnosed, additional lobectomy and lymphadenectomy were conducted. Further lobectomy was not performed in any other cases. In patients with mini-invasive lung cancer, lymph node sampling was performed.
Definitions and endpoints
Technical success for CT-guided localization procedures was defined by the ability to visualize the selected localization materials (HW or AN) during VATS resection procedures without their becoming dislodged and by the presence of the target PN within the resected lung parenchyma segment. The CT-guided localization duration was measured as the period between the initial and final CT scans. Pain severity associated with the localization procedure was measured with a visual analog scale (VAS, 0–10). VATS procedure duration was measured from first incision to wound closure.
The technical success rate of CT-guided localization procedures was the primary endpoint for this study, while localization duration, VAS scores, incidence of localization-related complications, VATS duration, blood loss, surgical type, and final diagnoses were secondary outcomes.
Statistical analysis
SPSS 16.0 (SPSS, Inc., IL, USA) was used for all statistical analyses. Continuous data that were and were not normally distributed were respectively reported as means ± standard deviations and medians (Q1; Q3), and were compared using Student’s t-test or the Mann-Whitney U test. The χ2 test or Fisher’s exact test was used when analyzing categorical data. Risk factors related to the incidence of pneumothorax and pulmonary hemorrhage were identified through a logistic regression approach, with those variables exhibiting a p-value < 0.1 in univariate analyses having been included in the multivariate analysis. P < 0.05 was selected as the threshold to define significance.
Results
Patient characteristics
In total, 98 patients (105 PNs) and 93 patients (107 PNs) underwent CT-guided HW and AN localization procedures, respectively (Table I). The HW and AN groups included 91 and 82 patients, respectively, who underwent localization of a single PN, and 7 and 11 patients, respectively, who underwent localization of multiple PNs.
Table I
Comparison of baseline characteristics between groups
Localization outcomes
The rates of successful localization in the HW and AN groups were 95.2% (100/105) and 99.1% (106/107), respectively (p = 0.117, Table II). Technical failure impacted 5 patients (5 PNs) in the HW group as a consequence of HW dislodgement, and 1 patient (2 PNs) in the AN group owing to pneumothorax following the successful localization of the first PN, after which the needle tip was unable to penetrate the pulmonary parenchyma, leading to localization failure. A significantly higher dislodgement rate was thus observed in the HW group (4.8% vs. 0.0%, p = 0.029). Both groups exhibited similar localization duration (p = 0.745), but the mean VAS score for the HW group was significantly lower than that for the AN group (p = 0.001).
Table II
Comparison of localization-related data
Localization-related complications
Pneumothorax impacted 21 (21.4%) and 15 (16.1%) patients following HW and AN localization, respectively (p = 0.349). Univariate analyses indicated that the localization of multiple PNs (p = 0.028) and changing location (p = 0.01) were significantly associated with pneumothorax incidence, although neither remained significant upon subsequent multivariate analysis (p = 0.672 and 0.158).
Pulmonary hemorrhage affected 29 (29.6%) and 23 (23.7%) patients who underwent HW and AN localization, respectively (p = 0.354), and univariate analyses failed to identify any risk factors associated with this complication.
VATS outcomes
With the exception of 1 patient who underwent HW localization, all VATS-guided limited resection procedures were successful (Table II). While technical failure impacted the localization outcomes for 5 patients in the HW group, 4 were ultimately able to undergo limited resection successfully as the point of bleeding caused by the puncture needle was still visible in the visceral pleura during the VATS procedure. For this same reason, the 1 patient in the AN group who experienced technical failure was also able to undergo limited resection. There were no instances of conversion to thoracotomy. Surgery types are presented in Table II. The median VATS duration (60 min vs. 80 min, p = 0.002) and blood loss levels (10 ml vs. 20 ml, p = 0.001) in the HW group were significantly lower than those for the AN group. The final diagnoses are presented in Table III.
Table III
Comparison of VATS related data
Multiple PN localization
Subgroup analyses based on the localization of multiple PNs are presented in Table III. In total, HW localization was performed for 7 patients with 14 PNs, while AN localization was performed for 11 patients with 25 PNs. The respective rates of successful localization in these groups were 100% and 96% (p = 1.000), and these groups exhibited comparable procedural durations for both localization (19.0 min vs. 20.0 min, p = 0.649) and VATS (140.0 min vs. 90.0 min, p = 0.586) procedures. AN localization was associated with a lower median VAS score as compared to HW localization (3 vs. 4, p = 0.015). Comparable pneumothorax (42.9% vs. 36.4%, p = 1.000) and pulmonary hemorrhage (42.9% vs. 45.5%, p = 1.000) rates were observed in the HW and AN groups (Table IV).
Table IV
Subgroup analyses based on multiple PN localization
Discussion
Here, the relative clinical efficacy and safety of CT-guided HW and AN approaches to PN localization were compared. While both groups exhibited similar rates of localization success, a significantly lower dislodgement rate was detected in the AN group relative to the HW group, and the only AN case that experienced technical failure was not the result of dislodgement. AN-based localization was also associated with lower levels of pain as compared to the HW-based approach. As such, the use of an AN may represent a more stable and more comfortable alternative to using a HW system for the CT-guided localization of PNs.
Based on these analyses, AN-based approaches to PN localization appear to offer certain advantages over the use of a HW approach. The utilized anchor claw consists of four blunt tips shaped like fish hooks, enabling more reliable fixation than that achieved with the HW system. In addition, this approach uses a soft suture in contrast to the hard steel wire necessary for HW localization, thus improving patient tolerance and placing fewer restrictions on patient activity, as confirmed in several prior studies in which this metal wire was replaced with a suture [13–15].
The present results revealed that the safety profiles and HW- and AN-based localization procedures were comparable. This is in contrast with a previous report wherein pneumothorax rates were similar in the HW and AN groups (31.3% vs. 27.2%, p = 0.397), whereas AN-based localization was associated with a significant reduction in pulmonary hemorrhage incidence (16.9% vs. 37.5%, p = 0.003). No risk factors related to pneumothorax or pulmonary hemorrhage incidence were identified in the present study, and these inconsistent findings may be attributable to the relatively small sample size.
While 6 patients in this study experienced technical failure with respect to their localization procedures, only 1 patient was ultimately unable to undergo VATS-guided limited resection. For those patients who underwent successful localization, resection can be readily performed with the guidance of the localization marker. However, even in some instances of technical failure, limited resection can still be performed provided the puncture site can be identified intraoperatively [16], although this may prolong the VATS procedural duration. The median VATS duration in the AN group in the present study was significantly longer than that for the HW group (80.0 min vs. 60.0 min, p = 0.002), potentially because the AN group included more patients with multiple PNs as compared to the HW group.
Subgroup analyses were also conducted specifically for those patients who underwent localization procedures for multiple PNs. In these patients, no differences were observed between groups with the exception of pain scores, which were better for patients who underwent HW localization. This may be attributable to the limited sample size for patients with multiple PNs. Preoperative localization procedures for multiple PNs, however, are vital as they can enable the resection of multiple nodules in a one-stage VATS procedure [17, 18].
As an alternative approach, CT-guided coil localization is often performed for patients with PNs [11]. Relative to the HW approach, coil localization strategies are reportedly associated with significantly decreased complication rates [19]. Coil localization procedures, however, are more complex than AN or HW localization given the shape of the coil and the need to deploy its distal end adjacent to the nodule while its proximal end extends outside of the visceral pleura [16]. In some reports, AN localization has been established as a time-saving alternative to coil localization for patients with PNs [16, 20].
There are some limitations to this study. For one, this is a retrospective analysis, and as such it is subject to a high potential for bias. Additional randomized controlled trials will be necessary to validate these findings. In addition, these patients were operated on at two centers, and this may have introduced additional sources of bias owing to variations in the operative experience levels of staff at these institutions. Thirdly, neither of the materials in this study was suitable for localizing the hilar PNs. However, the preoperative localization technique was developed for localizing the peripheral PNs [10]. In the previous studies, whatever the localization materials were, they were only suitable for localizing the peripheral PNs [1, 2, 9]. Lastly, the number of patients with multiple PNs was relatively small, underscoring a need for further confirmation of the results for these patients.








