Introduction
Effective lung nodule (LN) management remains a clinical challenge. In one recent study of 2,537 patients with 7,008 LNs, just 5.5% of these patients were ultimately found to have lung cancer [1]. When LNs are over 8 mm in diameter, they are malignant in 62–72% of cases and it is recommended that patients undergo lung biopsy or regular computed tomography (CT) or positron emission tomography (PET)/CT follow-up [2–4]. Respective diagnostic yields associated with CT-guided lung biopsy and PET/CT analyses of LNs, however, are reportedly just 78.9–86.7% and 64.2–84.1% [5–7]. At present, video-assisted thoracic surgery (VATS) approaches are the standard means by which LNs are diagnosed [4].
Preoperative CT-guided localization is commonly used to ensure the accuracy of the VATS-guided wedge resection of LNs [8–10]. Coils, specialized liquids, and hook-wire (HW) localization materials are commonly used in this context [9]. While coil-based approaches are often associated with the lowest complication rates, coil localization procedures are complex, resulting in a longer duration for the localization procedure [9, 11]. Each material is associated with specific benefits and associated risks, with HW placement and percutaneous liquid injection being the most successful strategies that do not necessitate expertise or the use of specialized equipment [12]. Few studies to date, however, have compared these two techniques.
Aim
This study was developed to compare the relative safety and efficacy of preoperative HW and indocyanine green (IG)-based localization procedures in LN patients.
Material and methods
This single-center retrospective analysis was approved by the ethics committee of Ningbo First Hospital (No. 2022RS068). As the study was retrospective, the requirement for written informed consent was waived.
Study design
In total, 41 LN patients underwent CT-guided HW localization prior to VATS between December 2017 and December 2020. In January 2021, our hospital replaced HW with IG as a localization material. Overall, 53 LN patients underwent CT-guided IG localization prior to VATS in the period from January 2021 to September 2021.
Patients were eligible for inclusion in this study if they met the following criteria: a) a maximal long-axis diameter ≤ 15 mm; b) a LN-pleura distance ≤ 30 mm; and c) an intermediate-to-high risk of malignancy based on the results of radiological and clinical evaluations [2]. Patients were excluded if they exhibited: a) a maximal long-axis diameter < 5 mm; b) calcified LNs; c) LNs that had decreased in size upon CT-based follow-up; or d) severe comorbidities.
HW localization
A 16-row CT (Siemens, Berlin, Germany) instrument was used to perform HW localization under local anesthesia with the following settings: 120 kV tube voltage, 100 mA tube current, 2 mm thickness, 0.6 s gantry rotation time, and 1.1 pitch.
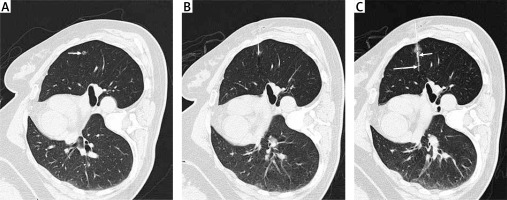
Patient positioning was determined based on the location of the target LN(s) (Photo 1 A). A needle pathway was selected so as to minimize the distance between the skin and the LN, after which a 21G introducer needle (Argon Medical Devices, Inc, TX, USA) was inserted into the lung parenchyma until the tip of the needle was within 10 mm of the target nodule (Photo 1 B). After CT-based confirmation of optimal needle positioning, the HW was released. Postoperative CT imaging was used to confirm appropriate HW localization and to detect any procedure-related complications.
IG localization
The needle puncture procedures were identical to those for the HW localization procedure. After the needle tip was appropriately positioned, the IG agent (2.5 mg/ml, 0.3 ml) was slowly injected. Postoperative CT imaging was used to detect any procedure-related complications.
VATS resection
VATS wedge resection (WR) procedures were performed under general anesthesia within 3 h following localization. A 3–5 cm incision in the chest wall was made, after which WR was performed based on HW visualization or IG fluorescence (Photo 2 C). The WR range was at least 2 cm from the localized area of the lung. Rapid intraoperative pathological analyses of the resected LN sample were then conducted. When LNs were confirmed to be invasive lung cancers, lobectomy and systematic lymph node resection were performed. The systematic lymph node dissection was performed according to the National Comprehensive Cancer Network guideline [13].
Endpoints
The technical success rate for the localization procedure was the primary endpoint for the present study, while secondary endpoints included the duration of the localization procedure, localization-related complication rates, WR technical success rates, surgical types, intraoperative blood loss, final patient diagnoses, and duration of hospitalization.
LN was defined as an intraparenchymal lung lesion of less than 3 cm in diameter, with no associated atelectasis or adenopathy [7]. HW localization was considered to be a technical success when the HW was visible and was not dislodged, while IG localization was considered to be a technical success when the IG fluorescence was visible on the lung surface and had not diffused away from the injection site. WR technical success was defined by the presence of the target LN within the resected tissue segment. Lung hemorrhage was defined as an emerging area of consolidation developed in the track of the puncture in the lung parenchyma [13, 14].
Statistical analysis
SPSS 16.0 (SPSS Inc., IL, USA) was used for all analyses. Quantitative are given as means ± standard deviation (SD) and analyzed via t-tests. Categorical data are given as n (%) and analyzed via χ2 tests. Risk factors associated with the occurrence of localization-related complications were identified through the use of univariate and multivariate logistic regression analyses, with those variables exhibiting a p-value < 0.1 in univariate analyses being incorporated into the multivariate model. P < 0.05 was the threshold of significance.
Results
Patient characteristics
Baseline patient data are compiled in Table I. A total of 41 patients in the HW group underwent the HW-based localization of 42 LNs, while the 53 patients in the IG group underwent the IG-based localization of 55 LNs. There were no significant differences in patient or LN characteristics when comparing these two groups.
Table I
Baseline data between 2 groups
Localization procedure success rates
The respective rates of successful localization in the HW and IG groups were 97.6% (41/42) and 100% (55/55) (p = 1.000, Table II). HW dislodgement was responsible for the only instance of unsuccessful localization in the HW group. The duration of the HW localization procedure (14.9 ±6.4 min) was significantly longer than that of the IG localization procedure (11.2 ±5.5 min) (p = 0.003, Table II).
Table II
Data of localization
Table III
Predictors of pneumothorax
Localization-related complications
The total complication rate was significantly higher in the HW group than that in the IG group (46.3% vs. 18.9%, p = 0.004, Table II). Rates of pneumothorax in the HW and IG groups were 22.0% (9/41) and 9.4% (5/53), respectively (p = 0.091, Table II), while respective lung hemorrhage rates in these groups were 29.3% (12/41) and 13.2% (7/53) (p = 0.054, Table II). In no instance did these complications impact the VATS procedures.
In univariate analyses, both upper lung lobe LN location (HR = 0.338, 95% CI: 0.098–1.164, p = 0.086) and IG-based localization (HR = 0.367, 95% CI: 0.113–1.191, p = 0.095) were identified as protective factors associated with pneumothorax incidence, while a prolonged localization procedure duration was a risk factor associated with a pneumothorax incidence (HR = 1.167, 95% CI: 1.057–1.288, p = 0.002). Of these factors, a multivariate analysis revealed that only localization procedure duration was independently associated with pneumothorax risk (HR = 1.170, 95% CI: 1.050–1.303, p = 0.004) (Table III), while localization materials were unrelated to the incidence of this complication (HR = 0.689, 95% CI: 0.187–2.608, p = 0.592). No risk factors were related to lung hemorrhage incidence in univariate analyses.
VATS procedures
VATS WR technical success rates were comparable in both the HW and IG patient groups (97.6% vs. 100%, p = 1.000), as was the VATS procedure duration (79.9 ±40.1 min vs. 84.1 ±42.2 min, p = 0.623) and intraoperative blood loss (22.3 ±21.0 ml vs. 26.7 ±18.5 ml, p = 0.800) (Table IV). One patient did not undergo VATS WR due to HW dislodgement, and this patient underwent lobectomy directly. The final diagnosis of this patient was mini-invasive adenocarcinoma. In no patients was the procedure converted to thoracotomy.
Table IV
Data of VATS and final diagnoses
A total of 9 patients (4 in the HW group, 5 in the IG group) were diagnosed with invasive adenocarcinomas based on the WR, all of whom underwent subsequent lobectomy with systematic lymph node dissection. None of these 9 patients had lymph node metastasis. The data of the surgical types are shown in Table IV. Details regarding final patient diagnoses are compiled in Table IV. There were no significant differences in the duration of postoperative hospitalization when comparing the HW and IG groups (7.9 ±3.6 days vs. 7.8 ±2.0 days, p = 0.793).
Discussion
The intraoperative identification of small LNs when performing VATS procedures represents a major technical challenge, necessitating the appropriate preoperative localization of these nodules to maximize success rates for VATS-guided WR procedures and to shorten the associated operative duration. Several localization materials and strategies have thus been developed for use in patients scheduled to undergo VATS-based LN resection, with each material exhibiting specific advantages and limitations [9]. In the present study, the relative efficacy and safety of HW- and IG-based LN localization approaches were compared.
Patients who underwent HW and IG localization procedures both exhibited high, comparable technical success rates with respect to localization outcomes, suggesting that both of these approaches can effectively enable LN localization. The 97.6% success rate for patients in the HW group was consistent with the 94–100% technical success rates reported previously [12, 14]. One recent meta-analysis calculated a pooled HW localization technical success rate of 98% [9], with HW dislodgement being the most common cause of localization failure, as occurred in 1 patient in the present study cohort.
As a liquid localization material, IG can be readily injected. Consistently, the localization duration for patients in the IG group was significantly shorter than that of patients who underwent HW localization (11.2 ±5.5 min vs. 14.9 ±6.4 min; p = 0.003). Methylene blue is another frequently utilized localization material [15–17], but IG exhibits superior localization utility given that it is more readily visible when imaged with high-resolution near-infrared instruments [16]. In this study, the technical success rate for IG localization was 100%, suggesting that the 0.3 ml injection volume used for these patients was sufficient [18]. When an excessive IG volume is injected, this can contribute to IG overflow, but prior reports have suggested that injection volumes below 0.3 ml may not be sufficient to facilitate appropriate localization [18]. The success of this approach was also associated with the smooth injection of IG into the target site in patients, as excessively rapid injection can also contribute to IG overflow.
Complications associated with localization procedures are an important consideration when selecting the optimal localization approach. In theory, HW procedures have a higher chance of causing complications owing to the rigidity of the HW apparatus. Although the differences in pneumothorax and lung hemorrhage rates did not reach statistical significance, we found a significantly higher total complication rate in the HW group than that in the IG group (46.3% vs. 18.9%, p = 0.004). Therefore, IG localization may exhibit better safety than HW localization.
The pneumothorax rate in patients undergoing the HW localization in this study (22.0%) was lower than the 33–38% rates reported previously [12, 19, 20]. This may be attributable to the limited sample size in this analysis, or to the mean LN-pleura distance of 8.8 ±7.2 mm for patients in the HW group, such that most localized LNs were subpleural, contributing to lower rates of pneumothorax and lung hemorrhage. Univariate and multivariate logistic regression analyses revealed a longer duration of localization to be independently associated with the risk of pneumothorax. Although localization materials were not found to be independently related to pneumothorax incidence, given that IG localization was associated with a shorter average localization procedure duration, this may indirectly contribute to lower pneumothorax rates.
WR resection success rates, VATS procedure duration, blood loss, and duration of postoperative hospitalization were comparable in both patient groups, suggesting that the choice of localization materials does not impact subsequent VATS procedures. The rate of invasive adenocarcinomas in this study was 9.3%. This rate was lower than that (30.3–58.8%) in many previous studies [4, 13–15]. This finding may be attributed to the fact that a majority of the LNs (77.3) were pure ground glass nodules (GGNs). The rate of invasive adenocarcinomas among the pure GGNs was not high (13.9%) [21].
There are certain limitations to this analysis. For one, this was a retrospective study that is susceptible to selection bias, although the comparable baseline characteristics in both groups may have helped to partially mitigate such bias. Second, HW and IG localization procedures were performed during different periods of time, and the experiences and skill levels of the operators performing these procedures were not identical. Third, no risk factors were identified as being associated with lung hemorrhage incidence in this analysis. Future large-scale clinical trials will be essential to expand on these analyses.
Conclusions
These data suggest that both HW and IG localization approaches can yield similar efficacy outcomes when used for preoperative LN localization. However, IG localization may exhibit better safety than HW localization. Among the LNs, there may be a small number of patients with LN requiring lobectomy.