Introduction
Angiotensin II (AT) is a potent vasoconstrictor and hypertensive drug. It acts directly on the receptors for angiotensin type 1, but also stimulates secretion of vasopressin (an antidiuretic hormone acting on V1 receptors) and ACTH (thereby increasing cortisol synthesis), and may improve adrenergic transmission (norepinephrine, epinephrine, dobutamine – acting non-selectively on a1 receptors) and stimulate aldosterone secretion [1]. This therefore results in potentiation of the effects of vasoconstrictive drugs from different groups.
AT is a drug registered for the treatment of severe hypotension in vasoplegic shock [2]. In clinical practice, it is most commonly used in the adjunctive treatment of septic shock and vasoplegia after extracorporeal circulation. The results of the ATHOS-3 study showed that its clinical effect (increase in blood pressure, reduction of the dose of previously used vasoactive drugs) is significant [3]: an increase in mean arterial pressure (MAP) of at least 10 mm Hg or to a value of 75+ mm Hg was almost 8 times more frequent after the use of AT than in the control group (OR = 7.95; 95% CI: 4.76–13.3). AT was introduced as a second-line drug after any other hypertensive drug when a norepinephrine equivalent dose (NED) of 0.2 μg/kg/min was reached. In addition to the haemodynamic effect, statistically significant reductions in mortality were observed when AT was used in specific groups of patients with distributive shock: those with baseline elevated renin levels (HR = 0.56; 95% CI: 0.35–0.88) [4], those with acute kidney injury requiring renal replacement therapy (HR = 0.52; 95% CI: 0.3–0.87) [5], and when used at relatively low doses of norepinephrine (or its equivalent), i.e. ≤ 0.25 μg/kg/min (HR = 0.51; 95% CI: 0.27–0.94) [6]. This is a significant finding because a recently published meta-analysis including surgical patients did not document that the use of vasopressin (a widely used vasopressor) reduced the risk of death compared with the use of norepinephrine (OR = 1.60; 95% CI: 0.47–5.50) [7]. Also, another observational study found that the effect of AT was more beneficial when it was included at NED < 0.3 μg/kg/min [8].
The use of AT in cardiac surgery may be very beneficial. There is an observed increase in MAP and a reduction in the vasopressors already used, with minimal thromboembolic risk [9]. The rationale for including AT in cardiac surgery patients is that plasma renin activity increases after extracorporeal circulation and correlates with increased vasoplegia syndrome [10], and higher renin levels in turn correlate with a greater need for norepinephrine, but not for AT to achieve a pressor effect [11]. A limitation of the widespread use of AT among cardiac surgery patients is the lack of results comparing AT with vasopressin or norepinephrine in pulmonary hypertension.
Proposal for the use of AT in vasoplegia syndrome in cardiac surgery
Growing experience with the use of AT in cardiac surgery allows the first therapeutic algorithms to be created [12]. Clinical criteria for the application of AT include septic shock and vasoplegia after extracorporeal circulation (including during extracorporeal membrane oxygenation, ECMO). Assessment of cardiac function, haemodynamic response to vasopressors used to date, and the presence of features of pulmonary hypertension all need to be considered in making the decision. In a hypotensive patient, it is necessary to introduce a pulmonary artery (Swan-Ganz) catheter and perform a panel of measurements – cardiac output (CO/CI), systemic vascular resistance (SVR/SVRI) and pulmonary vascular resistance (PVR/PVRI) – before the drug is infused. It is important to exclude low cardiac output syndrome (e.g. cardiac index, CI < 2.2 l/min/m2); i.e. cardiac output should be optimised with inotropic drugs or veno-arterial ECMO (VA ECMO) before starting AT. We suggest excluding patients with severe pulmonary hypertension (e.g. mean pulmonary artery pressure, mPAP > 45 mm Hg or nitric oxide insufflation) from the therapy. The measurement of systemic resistance during VA ECMO should be calculated from the blood flow at the pump and MAP. Vitamin C (ascorbate), B1 (thiamine) or other drugs of unproven effect should not be administered during therapy [13].
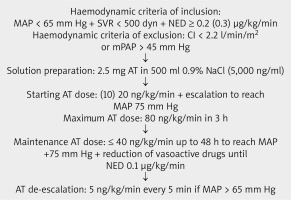
Haemodynamic criteria for AT infusion include: MAP < 65 mm Hg and/or a confirmed reduction in systemic resistance SVR < 500 dynes on haemodynamic calculation, despite the use of hypertensive medication at a norepinephrine equivalent dose (NED) of 0.3 μg/kg/min (e.g. combined dose of norepinephrine and adrenaline) (and hydrocortisone at a dose of 200 mg/day in the case of septic shock [13]), with normal vascular bed filling (e.g. cardiac filling on echocardiography, inferior vena cava respiratory diameter change, respiratory variation of pulse pressure) – as a second-line drug. If the patient has developed acute kidney injury requiring renal replacement therapy or high plasma renin activity is confirmed, AT should be considered at an NED dose of 0.2 μg/kg/min (patient 70 kg: dose 0.2 μg/kg/min ~ v = 10.4 ml/h norepinephrine 4 mg/50 ml) (Figure 1).
Preparation of the drug infusion and its dosage
A volumetric pump and a suitable set of drains are required to administer the drug. The drug should be prepared in a solution of 2.5 mg of AT in 500 ml of 0.9% NaCl (i.e. 5,000 ng/ml, giving an infusion for 48 h) [2]. The starting dose of the drug is 20 ng/kg/min (i.e. a 70 kg patient receives ~16.8 ml/h of solution). Alternatively, if the risk of peripheral ischemia is estimated to be high, one may choose a lower starting dose of 10 ng/kg/min (i.e. a 70 kg patient receives ~ 8.4 ml/h of solution). The maximum dose of the drug is 80 ng/kg/min in the first 3 h. The dose is individually adjusted until a MAP of 75 mm Hg is reached. The maintenance dose should be no more than 40 ng/kg/min and be continued up to a maximum of 48 h. When MAP +75 mm Hg is stabilised, reduction of the dose of norepinephrine (or other vasopressors) to 0.1 μg/kg/min is recommended, keeping the AT infusion at the speed of no greater than 40 ng/kg/min, and then it is suggested to reduce the AT dose by 5 ng/kg/min every 5 minutes when MAP > 65 mm Hg is stabilised. When MAP > 65 mm Hg cannot be achieved with AT requirements > 80 ng/kg/min during the first 3 hours of infusion, consider adding vasopressin (40 IU/40 ml per day) or methylene blue (10 mg of drug solution in 250 ml of 0.9% NaCl, 50 ml/h infusion) as third-line treatment.
Warnings
The summary of product characteristics [2] should be read before using AT. The use of the drug should be documented for potential adverse effects and, if they occur, reported immediately to the Office for Registration of Medicinal Products, Medical Devices and Biocidal Products or to the entity responsible for distribution of the drug [14].