Pulmonary artery sarcoma (PAS) is an extremely rare neoplasm arising from mesenchymal cells of the pulmonary artery [1]. PAS was first described in 1923, its incidence is about 0.001% to 0.03% and it is characterized by a very poor prognosis [2]. Early and correct diagnosis is crucial. Unfortunately misdiagnosis is quite common due to overlapping clinical characteristics with pulmonary embolism (PE) or chronic thromboembolic pulmonary hypertension (CTEPH), leading not only to delayed therapeutic management but also to unnecessary (and associated with hemorrhagic risks) thrombolytic and anticoagulation therapy [3].
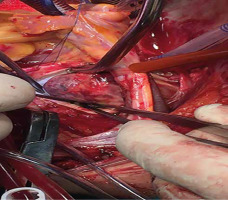
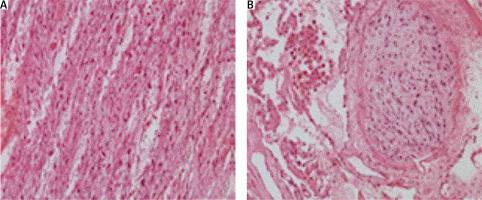
A 68-year-old woman was referred to our Cardiothoracic Department with a case of chronic pulmonary thromboembolic disease in order to undergo pulmonary endarterectomy. She had a history of dyspnea one year ago with gradual deterioration during the last 3 months. A few days before, she was admitted to the Pneumonology Department suffering from thoracic pain. D-dimer levels were mildly elevated. She underwent a chest computed tomography (CT) scan which revealed an inhomogeneous mass arising into the medial bronchopulmonary segment with irregular borders. Triplex vascular ultrasound was performed twice and was negative for deep venous thrombosis. CT pulmonary angiography was suggestive for pulmonary embolism based on the following signs: filling defects in right main bronchus expanded peripherally to medial and lower lobe. Ventilation/perfusion lung scan showed normal ventilation with complete absence of perfusion of the right lung. Dilated right ventricle and estimated systolic pulmonary artery of 39 mm Hg were the main echocardiographic findings. She underwent an elective cardiothoracic surgical procedure with the use of a cardiopulmonary bypass under deep hypothermia (lowest 19°C). Intraoperatively, material from the right pulmonary artery was obtained and examined in frozen sections (Figure 1). The main finding is a mass protruding in the lumen of the pulmonary artery and filling its branches in a mold-like manner (Figure 2). The frozen sections (Figure 3) demonstrated a malignant neoplasm with sarcomatous features. It consisted of highly pleomorphic cells with evident mitotic activity, in an edematous or slightly myxoid background. The cells were either spindle-shaped with enlarged, elongated nuclei, or round to oval-shaped with vesicular nuclei. There were also scattered multi-nucleated cells with lobular nuclei. Subsequently, a right pneumonectomy was performed. Duration of mechanical ventilation was 20 hours and ICU stay lasted 3 days. The patient was discharged on the 6th postoperative day without complications. She underwent chemotherapy and survived 11 months.
Figure 2
Mass protruding in the lumen of the pulmonary artery and filling its branches in a mold-like manner
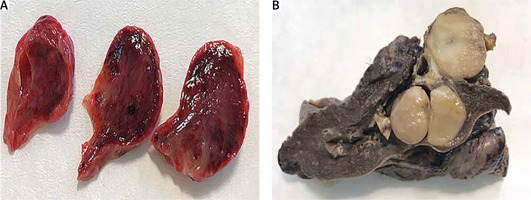
Figure 3
The frozen section (200×) demonstrates malignant neoplasm with sarcomatous features. The tumor seemed to originate from the intima of the pulmonary artery
Intimal sarcoma of the pulmonary artery was first described by Moritz Mandelstamm in 1923 [4]. The true incidence of pulmonary artery intimal sarcoma is unknown, because it is most often misdiagnosed. A high level of suspicion is required due to resemblance in clinical presentation to acute or chronic pulmonary embolism (dyspnea, chest pain, cough, hemoptysis). Hemodynamic instability is suggestive for PE while IPAS is characterized by more long standing symptoms. Diagnosis is based on contemporary imaging examinations and more accurately on histopathologic studies. Contrast-enhanced CT scan is the initially performed study in most cases. Delayed contrast enhancement in CT angiography, especially in the venous phase, is a helpful radiographic diagnostic sign [5]. The role of 18F-fluorodeoxyglucose positron emission tomography in the diagnosis of PAS is a matter of debate but is suggestive for treatment response evaluation [6, 7]. Histologic examination is the most reliable tool for the correct diagnosis. Preoperative biopsies carry high risk of complications. More specifically, MDM2 and PDGFRA amplifications represent the major histopathologic findings [8]. Radical resection including with clear margins should be the management goal. In many cases pneumonectomy is the appropriate surgical decision. Better prognosis has been reported in combined radical resection with chemotherapy [9]. Also, improved survival was the result of radiation therapy and chemotherapy after surgical resection [10, 11]. In the case of extensive disease palliative pulmonary endarterectomy should be considered since this surgical technique results in symptomatic relief [12]. Distant metastases are quite common, affecting 16–25% of patients [13]. Despite medical innovations and a radical surgical approach, prognosis remain very poor with a reported mean survival of 12–18 months.