Introduction
Non-melanoma skin cancers are the most common cancers in the world, and squamous cell carcinoma (SCC) of the skin accounts for the second highest percentage after basal cell carcinoma (BCC) [1–3]. The risk of SCC increases with age and in sun-exposed skin [4, 5].
Recent studies show that the incidence of SCC is increasing faster than that of BCC, and in addition to this, SCC is more prone to both locoregional and distant spread compared to BCC [3]. Large tumours arising in the head area exposed to strong sunlight in immunocompromised patients are more susceptible to metastases [6]. However, the overall low rate (0.4%) of metastatic stage prevented the development of effective treatment strategies until a few years ago [7].
Early SCC has a good prognosis with a 5-year survival rate of ≥ 90% after treatment [3, 7, 8]. Moreover, at an advanced stage SCC can cause significant damage to organs, resulting in disfigurement and loss of function. Treatment of advanced SCC is often complicated, requiring extensive surgery followed by adjuvant therapy.
Although surgery is the mainstay of local treatment of skin cancer, radiotherapy (RT) is used as the primary treatment in cases where surgery would cause significant aesthetic and/or functional deficits or depending on individual patient preferences [9, 10].
Radical RT regimens for skin cancers usually consist of daily treatments for several weeks [11]. However, such RT regimens may not be acceptable to patients who are unable to make many daily trips for weeks due to economic, social, or physical constraints. If left untreated, SCC will continue to progress and cause distressing symptoms such as impaired function, severe pain, and ulceration associated with cancer, bleeding, and infection.
One popular approach in the palliative treatment of head and neck cancers in North America is the QUAD SHOT regimen. This approach was introduced in the alleviation of pelvic malignancies in the Radiation Therapy Oncology Group (RTOG) 8502 phase II study in 1980 [12].
The regimen administered 3.7 Gray (Gy) twice daily for 2 consecutive days (total 14.8 Gy/cycle), repeated every 3 to 6 weeks, for a total of 44.0 Gy over 3 cycles. If the patient did not achieve complete regression after the third cycle of RT, and the patient tolerated the previous cycles well, the next cycle could be administered without exceeding the dose to organs at risk.
The cyclical nature of the RT regimen allowed the response to treatment to be assessed after each course, at which time a decision was made to continue the next course. The biologically equivalent dose administered in the QUAD SHOT regimen is below the threshold for inducing acute mucositis, and the interval between treatment cycles allows for mucosal recovery before the next cycle.
In the RTOG 8502 study, the results were as follows: complete remission (10%); partial remission (22%); no change (24%); progression (10%); and unknown (27%). Overall response rate and overall tolerability achieved adequate results with an adequate safety profile (G3 toxicity in only 5% of patients, no G4 toxicity). The median local control was limited with progression-free survival of 3.1 months. In addition, this regimen allows patients to complete the entire cycle in 2 days, reducing the travel burden and time required in the healthcare facility for palliative treatment. The purpose of this study was to review a single institutional experience of the RTOG 8502 QUAD SHOT regimen using volumetric modulated arc therapy (VMAT) for incurable non-melanoma skin cancer.
Material and methods
The clinical material comprised a group of patients treated at the Radom Oncology Centre in the years 2019–2022, who underwent the RTOG 8502 QUAD SHOT regimen (14.8 Gy/4 fractions, twice daily with a 6 h interval, on 2 consecutive days). Courses were repeated every 4 weeks 3 times using VMAT. Between December 2019 and December 2022, nine patients with skin cancer were treated with at least one cycle of the QUAD SHOT regimen. Treatment plans included the use of VMAT with 6 MV photons generated by a linear accelerator. Two daily fractions of 3.7 Gy were administered at least 6 hours apart on 2 consecutive days, for a total of 14.8 Gy in 4 fractions. The treatment regimen was repeated every 4–5 weeks for a total of 3 cycles. Eligible patients had a histologically confirmed malignancy of primary skin cancer origin. They were ineligible for surgery due to the extent of the disease, serious comorbidities, fitness, or refusal to undergo conventional treatment. The patients were disqualified from surgery but met the indications for RT. During the treatment, a subjective response of the patient was observed in the form of less pain and better well-being. Additionally, there was an objective response after each cycle, and smaller volumes for RT were planned. Tumour response, symptom relief, and toxicity were assessed every 4–5 weeks prior to the next treatment cycle for eligibility for treatment when tumour regression occurred. Tumour response was assessed by physical examination and computed tomography (CT) scan to plan the next cycle. Symptom relief was defined as a subjective reduction in the presented symptoms [13, 14]. Overall response was defined as tumour response or symptom relief. Toxicity was assessed using the Common Terminology Criteria for Adverse Events version 5.0. Acute toxicity was defined as occurring up to 3 months after the end of treatment. All treated patients noticed improvement and less bleeding.
Two to three weeks after the first QUAD SHOT RT, patients noticed that SCC decreased significantly and bleed less, which motivated them to continue the next cycle. Subsequent cycles of the QUAD SHOT regimen were scheduled on new non-contrast CT scans for dose planning for residual lesions. Successfully, patients completed the second and third QUAD SHOT every 4–5 weeks, resulting in a continuous decrease in SCC. Two patients received 2 cycles, and 7 patients received 3 cycles. Grade 2 toxicity was observed in 4 (44.4%) patients, no grade ≥ 3 or late acute toxicity was observed.
Before starting treatment, all patients signed an informed consent form for treatment at the Radiotherapy Department of Radom Oncology Centre and the publication of their image.
Results
A total of 9 patients were included in the study – 7 (77.78%) women and 2 (22.22%) men, aged 60–98 years (median age 79.08), who were treated for skin cancer: SCC in 6 patients and BCC in 2 patients. One patient received RT to 2 areas for SCC and BCC in 2 other areas of the body. The grade of malignancy was G2 (4 cases), one case was grade G1, and in the remaining cases the grade of malignancy was not specified.
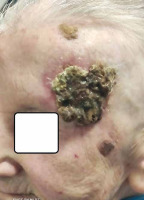
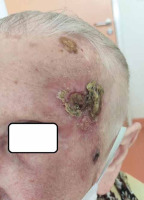
The irradiated areas were as follows: 2 cases – nose skin; 2 cases – cheek; one case the area of the superciliary ridge with the eyelid; one case the forehead; one case the skin of the temples; one case the skin of the sternum; one case the skin of the shoulder blade. All patients were disqualified from surgery due to serious chronic diseases or lack of consent. Most of the patients were WHO 2 (5 cases – 55.6%), and the rest were defined as WHO 1 (3 patients) and WHO 3 (one patient). One patient underwent 3 cycles in 2 areas, with a total of 6 treatment cycles. Six patients received 3 treatment cycles. The remaining 2 patients received 2 cycles of RT, but due to the deterioration of their general condition and exacerbation of chronic diseases, they were not qualified for the third cycle. Photographs demonstrating the response in the 2 patients, along with the dose distribution and volume irradiated during successive cycles of RT (Figs. 1–14). A comparison of the irradiated areas (PTV) during successive courses of RT in the patients presented in the photographs is shown in Table 1.
Fig. 2
Patient 1st – the treatment planning volume before the first course of radiotherapy. Clinical target volume = 290.198 cm3, planning target volume = 401.249 cm3
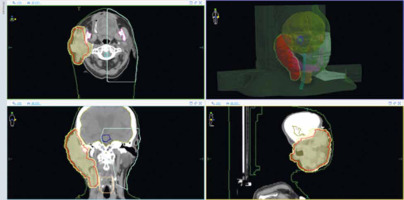
Fig. 4
Patient 1st – the treatment planning volume before the 2nd course of radiotherapy. Clinical target volume = 234.146 cm3, planning target volume = 331.219 cm3
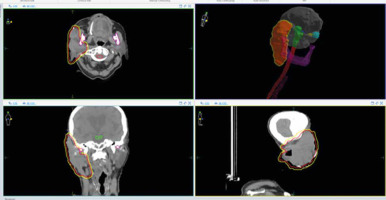
Fig. 6
Patient 1st – the treatment planning volume before the 3rd course of radiotherapy. Clinical target volume = 125.628 cm3, planning target volume = 269.844 cm3
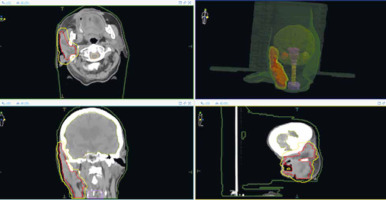
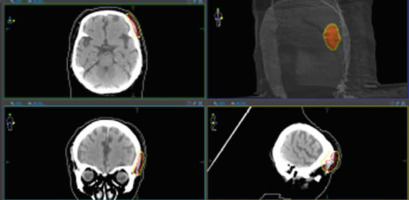
Fig. 9
Patient 2nd – the treatment planning volume before the 1st course of radiotherapy. Clinical target volume 1 = 61.967 cm3, planning target volume 1 = 124.922 cm3
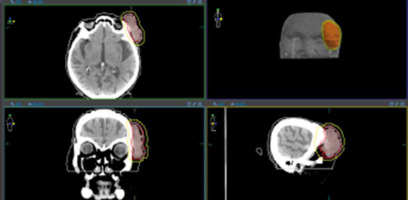
Fig. 11
Patient 2nd – the treatment planning volume before the 2nd course of radiotherapy Clinical target volume 1 = 13.022 cm3, planning target volume 1 = 45.129 cm3
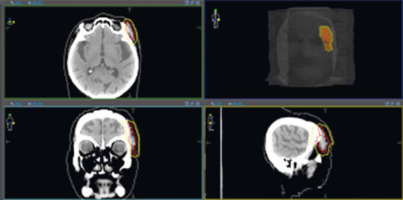
Fig. 13
Patient 2nd – the treatment planning volume before the 3rd course of radiotherapy Clinical target volume 1 = 6.977 cm3, planning target volume 1= 20.421 cm3
Discussion
Although definitive multi-week RT courses for skin cancer have shown excellent local tumour control and aesthetic results (particularly in facial changes), prolonged daily RT regimens can be a huge challenge for patients with a lack of socioeconomic support, physical impairment, or non-adherence to a daily treatment regimen.
Both, intensive dose rate modulation (IMRT) and VMAT RT similarly cover a large volume of cancer. Compared to conventional fixed-field IMRT irradiation, VMAT provides more conformal coverage of tumour volume with similar dose for organs at risk (OAR). In addition, the treatment time using VMAT is significantly shorter than conventional IMRT. Approximate treatment times are 2–4 and 10–15 minutes for VMAT and IMRT, respectively [15]. The introduction of VMAT into the palliative RT regimen may provide a good response to treatment with reduced toxicity.
Short-term palliative daily RT regimens (20–30 Gy in 5–10 fractions) for skin cancer in the head and neck region demonstrated only a small percentage of symptom relief (50–60%) with high acute grade 3 or higher (grade 3+) mucositis (62%) and dermatitis (56%) [16, 17].
Among RT regimens, QUAD SHOT requires only 2 consecutive days of hospital visits per cycle. Based on a proprietary study, excellent local tumour control (53–77%) and symptom relief (56–85%) with minimal side effects (grade 3+, 6–9%) have been demonstrated in cancer patients [13,16–19]. While the biologically effective dose with QUAD SHOT appeared to be lower than other multi-week RT regimens, repeated QUAD SHOT demonstrated excellent tumour responses: 100% with QUAD SHOT × 3; 44–50% for schemes smaller than QUAD × 3 [18].
With advanced technology (such as IMRT RT or proton therapy), highly conformal QUAD SHOT regimens can allow for a higher radiation dose to the tumour, saving OAR compared to 2- or 3-dimensional RT techniques. However, there is limited information regarding radiation dose limits in the OAR during 3 or more QUAD SHOT cycles.
The main advantages of the QUAD SHOT regimen include high tolerance to low-toxicity RT, shortened treatment time, and excellent local tumour control, as well as reduced symptoms compared to other prolonged palliative RT regimens [13, 16–19].
Practically, the QUAD SHOT scheme allows planning of the next CT to achieve a target volume for each subsequent treatment cycle in order to take into account the tumour response from previous QUAD SHOT cycles, which can reduce the radiation dose to critical organs, resulting in further reduction of toxicity.
The flexibility of QUAD SHOT treatment based on the patient’s general condition and tumour response is also one of the important clinical considerations. Some patients with tumour progression or general health deterioration due to other comorbidities rather than RT-related toxicity are advised not to receive an additional QUAD SHOT cycle, to avoid ineffective treatment or unnecessary treatment-related side effects. While receiving less than 3 QUAD SHOT cycles may still offer an acceptable rate of symptom relief (55–67%), we know that the best symptom relief (nearly 89%) was seen in patients who received 3 or more QUAD SHOT cycles [13, 18, 19].
Our observations and results suggest that the QUAD SHOT regimen using VMAT is one of the strongest candidates for palliative RT regimens, with good response to treatment and low toxicity. When choosing a palliative treatment method, palliative RT should always be considered, to alleviate or prevent locoregional symptoms. The risk of severe toxicity should be considered and avoided [11].
Conclusions
This is a retrospective study based on a relatively small number of patients. There is a possibility of selection bias, which may affect treatment and analysis results. We did not assess the effect of palliative RT on improvement of overall survival, but the only goal of palliative treatment, as improvement of the quality of life in the form of less infiltration, less bleeding, and less pain, was observed in all treated patients. In Poland, we can consider systemic treatment in the first line with the use of an inhibitor of the Hedgehog pathway (vismodegib) in patients who have progressed after RT or who have contraindications to RT. Second-line treatment is available for patients with immunotherapy (cemiplimab) who have progressed or are intolerant to a Hedgehog pathway inhibitor.
A prospective study with a larger cohort should be conducted to further assess the value of introducing modern advanced RT techniques to the QUAD SHOT regimen for patients with skin cancer.