Summary
This is the first study that examined changes in quality of life (QoL) after percutaneous closure of paravalvular leaks (PVL). It shows that a successful PVL closure procedure is asso-ciated with improvement in QoL indices assessed with MLHFQ and KCCQ questionnaires. Due to low number of failed cases it is currently not possible to establish the relationship between lack of procedural success and changes in QoL.
Introduction
Paravalvular leaks (PVLs) following surgical valve replacement are relatively common. It is estimated that they affect about 6% of patients with prosthetic aortic valves and 32% of patients with prosthetic mitral valves at the time of discharge after surgery [1]. PVLs are usually asymptomatic but in some cases cause symptoms that can be attributed to development of heart failure (similar to native valve insufficiency) and/or hemolysis [2, 3].
Patients with symptomatic PVLs in most cases (~90%) present with heart failure symptoms due to volume overload [4]. The left ventricular ejection fraction is often preserved. Diagnosis may be difficult and requires clinical vigilance, especially in PVLs around mechanical mitral valves, since the regurgitant jet may not be visible due to acoustic shadowing.
It has been established that presence of heart failure is associated with diminished quality of life (QoL) [5]. The World Health Organization defines QoL as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. It is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, personal beliefs, social relationships and their relationship to salient features of their environment” [6]. In a clinical scenario of a heart failure patient quality of life assessment aims to describe health-related QoL. The health-related quality of life (HRQoL) of patients with HF reflects the impact of HF on their daily lives and provides information that cannot be obtained by physical examination or laboratory assessment. Evaluation of QoL in patients with heart failure should not be omitted since there are data indicating that poor QoL correlates with more hospitalizations and higher mortality [7]. QoL seems to be extremely important for patients with heart failure since it has been shown that some patients may even be willing to trade survival for improved QoL [8].
Today percutaneous closure of paravalvular leaks offers a less invasive approach which is associated with lower periprocedural mortality compared to surgical techniques [9]. Surprisingly, technical success (successful delivery of the closure device into the intended location, no valve interference, no major complications and reduction of regurgitation to no greater than mild), which is achieved in 77–93.5% of cases (depending on operator experience), is lower than clinical success, which ranges from 67 to 77% at follow-up (no reinterventions for the underlying condition, improvement in symptoms, functional status and QoL) [10, 11]. QoL assessment has never been included as part of the routine follow-up after percutaneous closure of PVLs in any of the available studies.
In our study we decided to determine whether percutaneous closure of paravalvular leaks is related to improvement in QoL during follow-up. To assess QoL status we decided to use the Minnesota Living with Heart Failure Questionnaire (MLHFQ) and Kansas City Cardiomyopathy Questionnaire (KCCQ). The MLHFQ is a validated, disease-specific, self-administered questionnaire [12]. It consists of 21 questions that concentrate on the impact of heart failure on QoL. The KCCQ measures symptoms, physical and social limitations and quality of life in patients with heart failure. It contains 23 items that can be attributed to 7 domains. All scores are represented on a scale from 0 to 100 points where a lower score indicates more severe symptoms whereas a score of 100 implies no symptoms or limitations and an excellent quality of life [13]. The impact of percutaneous paravalvular leak closure on quality of life has never been examined. The following hypotheses were adopted:
Material and methods
This study was approved by an ethics committee (decision number: KNW/0022/KB1/90/I/12). Informed consent was obtained from all subjects involved in the study. The study was designed as a prospective registry of consecutive patients with mitral or aortic PVLs who were referred to our center for PVL assessment and met the following inclusion and exclusion criteria:
Inclusion: age > 18 years old, clinically significant PVL around prosthetic mitral or aortic valve (to be found clinically significant a subject with a PVL had to have heart failure symptoms – at least NYHA II and baseline NT-proBNP > 125 pg/ml), echocardiographic examination consistent with presence of a PVL with severity grade of moderate or higher, initial echocardiographic evaluation indicates that the PVL can be closed with a device of an appropriate size, able to understand and complete the MLHFQ and KCCQ questionnaires, subject was qualified for percutaneous PVL closure during a Heart Team discussion, subject is willing to participate in follow-up visits.
Exclusion criteria: signs of active infection, rocking valve, intracardiac mass, vegetation, tumor or thrombus, pregnancy, life expectancy less than 1 year in the opinion of the investigator, current participation in another interventional drug or device study, other comorbidities that significantly affect the QoL in the opinion of the investigator, other severe valvular heart disease.
Fifty-two patients were screened for participation in the registry during a 2-year period. Forty subjects met the inclusion criteria and did not meet any of the exclusion criteria. 12 patients were not included due to: rocking valve (1 subject), presence of other indications for cardiac surgery such as aortic aneurysm (2 subjects) and other severe valvular disease (2 subjects), lack of consent (3 subjects) and presence of other comorbidities that significantly affected the QoL (4 subjects). Study design is presented in Figure 1.
The initial evaluation, which consisted of physical examination, transthoracic (TTE) and transesophageal (TEE) echocardiographic examinations and laboratory tests (morphology, NT-proBNP, lactate dehydrogenase (LDH)) was conducted in an outpatient clinic. Each patient was discussed during a Heart Team meeting to determine the best course of action in each individual case (surgery or percutaneous PVL closure). Patients who were qualified for percutaneous PVL closure were admitted to the cardiology ward. Abovementioned blood tests and TTE were repeated. In addition, prior to the procedure, each patient was asked to complete the MLHFQ and KCCQ questionnaires. Percutaneous PVL closure procedures were performed under conscious sedation with sedatives administered as per unit protocol (fentanyl and diazepam intravenously) under RT-3DTEE and fluoroscopic guidance. All mitral PVLs were closed with a transseptal approach using steerable sheaths as described previously [11]. All aortic PVLs were closed using a transaortic retrograde approach. Prior to discharge each patient had another TTE. Follow-up visits were scheduled at 30 days, 6 months and 12 months after the procedure. During each follow-up visit the following procedures were performed: physical examination, TTE, laboratory tests (morphology, NT-proBNP, LDH). Each patient was also asked to complete the MLHFQ and KCCQ questionnaires. If any complication or worsening of PVL was suspected TEE was readily available and could be performed at the physicians’ discretion. The Medical University of Silesia obtained licenses to use the MLHFQ and KCCQ questionnaires for the purpose of this study.
Statistical analyses were conducted using the R Statistical language (version 4.1.1; R Core Team, 2021) on Windows 10 PRO 64 (build 19044). The significance level of the statistical tests in this analysis was set at α = 0.05. Normality of variables was tested using the Shapiro-Wilk test. In addition, the values of the measure of asymmetry (skewness) and shape (kurtosis) were considered. The distribution in which the skewness parameter did not exceed 2.0 and the kurtosis parameter was below 7.0 was considered normal. Parametric tests were used to test data that met the assumptions of normality; nonparametric tests were used for the remainder. For parametric tests with the number of groups above two, Fisher’s repeated measures one-way ANOVA with partial omega squared effect size was performed. Comparisons between pairs of outcomes were made using post-hoc Student’s t-tests. For nonparametric values with more than two groups, the Friedman rank sum test with Kendall’s coefficient of concordance was used. Comparisons between pairs of results were made using the post-hoc Durbin-Conover test. The statistics of the correlation test were based on Pearson’s product-moment correlation coefficient and followed a t-distribution with length (npairs – 2) degrees of freedom. An asymptotic confidence interval was given based on Fisher’s Z-transform.
Results
Patient demographics and medical history are depicted in Table I.
Table I
Patient demographics and medical history
Technical success (TS) was defined as successful delivery of the intended closure device without interference with the prosthetic valve. TS was achieved in 97.5% of cases. Procedural success (PS) was defined as TS and reduction of the PVL severity as assessed by periprocedural echocardiography to none or mild. Initially PS was achieved in 82.5% of cases (33 subjects). Out of 7 of the subjects in whom PS was not achieved 2 were qualified for another PVL closure attempt and subsequently underwent another procedure. In 1 of these patients another closure device was successfully placed, resulting in procedural success. Therefore overall PS was achieved in 34 (85%) cases. Results are presented separately for groups in which echocardiography confirmed no or trace residual PVL (echocardiographic success, PS achieved) and for groups with a mild or greater residual PVL (no echocardiographic success, PS not achieved). In cases classified as lack of PS moderate residual paravalvular regurgitation was described in 5 subjects and severe in 1 subject.
During follow-up there were 2 deaths in the group without PS, both due to heart failure and no deaths in the group with PS.Ttwo subjects in the PS group experienced worsening of hemolysis after PVL closure. In 1 case hemolysis was successfully treated with another procedure, and in the second case the subject required cardiac surgery. Procedural complications occurred in 4 subjects and consisted of 1 major vascular complication (hematoma with bleeding requiring surgical intervention) and 3 minor vascular complications (1 pseudoaneurysm and 2 hematomas treated conservatively). Overall 32 subjects in the PS group and 4 subjects in the group without PS attended all follow-up visits.
Influence of PVL closure on QoL measured by MLHFQ
Analysis showed that in the group of patients in which PS was achieved, there was a significant reduction in MLHFQ scores as early as 1 month after the treatment. The final score was significantly lower than the initial score and also lower than the score 1 month after the procedure (Figure 2). The resulting effect size was estimated as a “moderate decline.” In the subgroup without echocardiographic success, there was no significant difference between time points despite the decrease in scores mainly because of the small sample size (Figure 3).
Influence of PVL closure on KCCQ domains
Analysis showed that in the group of patients with procedural success there was a statistically significant increase in scores of all KCCQ domains except the self-efficacy score. On the other hand, no statistically significant difference was detected in KCCQ scores for the group without PS despite observed increases and decreases, mainly due to the small sample size. The results of changes in the quality of life and overall summary score domains are presented below. Due to limitations imposed by the journal on the number of figures that can be included in the article, graphical representations of changes in other KCCQ domains are not presented.
Quality of life domain
Analysis showed that in the group of patients with procedural success, there was a significant increase in quality of life scores as early as 1 month after the treatment. The final score was significantly higher than the initial score (Figure 4). The resulting effect size was estimated as a “large increase.”
Figure 4
Comparison of KCCQ quality of life mean scores in subgroup of patients with echocardiographic success

In the subgroup without echocardiographic success, there was no significant difference between the time points (mainly because of the small sample size) despite the decreases and increases in scores. The resulting effect size was estimated as “very small.” The final score was slightly higher than the initial score (Figure 5).
Overall summary score
Analysis showed that in the group of patients with procedural success, there was a significant increase in overall summary scores as early as 1 month after the treatment. The final score was significantly higher than the initial score (Figure 6). The resulting effect size was estimated as a “large increase.”
Figure 6
Comparison of KCCQ mean overall summary scores in subgroup of patients with echocardiographic success

In the subgroup without echocardiographic success, there was no significant difference between the two time points (mainly because of the small sample size) despite the decreases and increases in scores. The resulting effect size was estimated as “very small.” The final score was slightly higher than the initial score (Figure 7).
Influence of percutaneous PVL closure on NT-proBNP levels
Analysis showed that in the group of patients with PS, there was a significant decrease in NT-proBNP median concentrations as early as 6 months after the treatment (p < 0.05). The final score was significantly lower than the initial score (Figure 8). The resulting effect size was estimated as a “substantial decrease.” (Kendall’s coefficient = 0.64).
Figure 8
Comparison of NT-proBNP mean concentrations in subgroup of patients with echocardiographic success
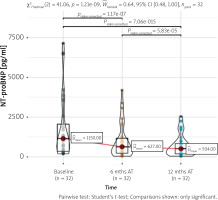
In the subgroup without echocardiographic success, there was no significant difference (p > 0.05) between the time points (mainly because of the small sample size). The resulting effect size was estimated as “slight” (Kendall’s coefficient = 0.06). The final score was lower than the initial score (Figure 9).
Influence of percutaneous PVL closure on LDH levels
Analysis showed that in the group of patients with PS, there was a significant decrease in median LDH concentration as early as 6 months after the treatment (p > 0.05). The final score was significantly lower than the initial score. The resulting effect size was estimated as a “slight decrease” (Kendall’s coefficient = 0.18).
In the subgroup without echocardiographic success, there was no significant difference (p > 0.05) between the time points (mainly because of the small sample size). The resulting effect size was estimated to be “small” (Kendall’s coefficient = 0.19). The final score was lower than the initial score.
Discussion
Current European guidelines for the management of valvular heart disease state that in the case of PVLs that lead to hemolysis or severe heart failure the preferred treatment option is surgical intervention (class I indication) and percutaneous treatment should be considered for patients at high or prohibitive surgical risk (class IIa) [14]. Indeed available data indicate that percutaneous PVL closure is not always successful, with clinical success ranging from 67% to 77% [15]. These rates are from relatively old studies when no dedicated PVL closure devices were available. Since that time the Occlutech PLD device has been released and novel interventional techniques have been introduced [10, 16]. Because of that, recent studies report a higher clinical success rate of 86.5% [17]. On the other hand, the surgical approach to PVL treatment is inherently associated with high mortality – rates of 7 to 11% have been reported [9]. In our study initial TS was achieved in 97.5% – in only one subject the operator was not able to deliver the closure device to the intended location. However, delivery of a device to the PVL channel is only part of the success, because a reduction in the degree of paravalvular regurgitation to no greater than mild is required to achieve improvement in heart failure symptoms [18]. In our registry procedural success defined in the abovementioned manner was achieved in 85% of cases.
For the purpose of quality of life assessment we chose the Kansas City Cardiomyopathy Questionnaire (KCCQ) and the Minnesota Living with Heart Failure Questionnaire (MLHFQ). These are the most commonly used tools to measure the quality of life in heart failure patients [19]. As mentioned in the introduction, the KCCQ contains 23 items that can be attributed to 7 domains. In addition, symptom frequency, physical limitations, social limitations, and quality of life can also be combined to create an overall summary score, which has been the primary health status outcome for the KCCQ in most trials [13]. All KCCQ scores are scaled from 0 to 100 and usually reported in 25-point ranges, where scores represent health status from very poor to poor (0–24) to good to excellent (75–100) [13]. A change of 5 points is considered to be clinically important and higher changes indicate greater improvement. The MLHFQ contains 21 questions with scores from 0 to 5 for each question. The overall score is obtained by summing individual scores and can range from 0 to 105. In the case of patients with HF it has been established that a score < 24 represents good QoL, 24–45 represents moderate QoL and > 45 represents poor QoL [19]. In our study successful percutaneous PVL closure improved QoL as measured by the abovementioned questionnaires. The mean MLHFQ score decreased from 49.78 to 30.84 at the 12-month follow-up in the group with PS, suggesting a significant improvement in QoL. However it should be noted that this mean value was still higher than 24, which indicates that the QoL of subjects with PS cannot be considered as ‘good’. This may be explained by various comorbidities that also influence the QoL such as chronic kidney disease, coronary artery disease and persistent atrial fibrillation. In the case of the results of the KCCQ questionnaire, improvement in scores of all domains was observed, as mentioned in the results section. In addition, the change in score of each domain was greater than 5 points. Since this was the first study to examine how percutaneous closure of PVLs influences the QoL, no comparison with other data is possible. However, both in patients with heart failure and those with valvular heart disease the KCCQ results are independently associated with risk of death or heart failure hospitalization [20]. Moreover, studies in which valvular regurgitation was corrected by transcatheter edge-to-edge mitral valve repair reported a significant and stable increase in mean KCCQ score during a 1-year follow-up [20, 21].
We also examined how percutaneous PVL closure would influence concentrations of NT-proBNP. Levels of NT-proBNP decreased significantly in the group of subjects with PS. NT-proBNP is a well-known prognostic marker in heart failure subjects. Its utility in patients with PVLs has not yet been established, but data from subjects with other moderate or severe valvular heart disease (except mitral stenosis) suggest that higher levels of NT-proBNP are associated with higher mortality [22].
Analysis also showed that in the group of patients with PS, there was a significant decrease in LDH median concentration as early as 6 months after the treatment. LDH is a marker of hemolysis and has to be assessed after every percutaneous PVL closure, because in some cases hemolysis develops de novo or worsens after the procedure [3]. Based on computational fluid dynamics simulations we recently reported that some degree of hemolysis is always present in the case of PVLs even when this pathology does not manifest clinically [23]. Therefore it is expected that successful closure should decrease LDH levels.
Our study has certain limitations that have to be acknowledged. By comparing only pre- and post-procedural QoL, bias from the placebo effect could be introduced. Unfortunately, the number of subjects in the group with no procedural success was low and therefore they could not be used as a comparator and no conclusions could be made regarding the influence of a failed PVL closure procedure on the QoL. It is however worth noting that there were some changes in the group without PS: the MLHFQ score was lower, and KCCQ quality of life and overall scores were higher at 12-month follow-up. Similarly, decreases in concentrations of NT-proBNP and LDH were noted. These observations can have various explanations. Firstly, two subjects died in the group with no procedural success and heart failure was the cause of both deaths. Since these 2 patients did not complete the 12-month follow-up, the results of their questionnaires were not analyzed. Secondly, all subjects had regular follow-up visits and the investigator was allowed to change pharmacological treatment at his own discretion. Therefore some improvement in QoL could be anticipated due to the higher standard of medical care that is usually offered to these patients. Furthermore, these small improvements in the group without PS may also be attributed to the placebo effect. Another limitation of the study is that the KCCQ questionnaires of only 29 subjects were analyzed, despite the fact that 32 subjects in the PS group completed the follow-up visits. This is due to the fact that the investigator failed to check whether the questionnaires were filled in correctly and in 3 cases there were errors in the KCCQ that excluded them from the analysis.














