Introduction
Gastroesophageal reflux disease (GERD) is a common condition that negatively affects the quality of life [1–4]. The frequency in western societies is stated as 10–30% in some studies [5]. Helicobacter pylori (H. pylori) is an important infection factor that colonises the antrum and corpus in the gastric mucosa in humans and causes disease in a wide spectrum. In a study, it was found that H. pylori was protective in terms of the development of oesophagitis [6]. There are results showing that H. pylori infection has no protective role against GERD [7–9], even though infection due to this organism may cause reflux disease or exacerbate previously existing reflux disease [8]. However, there are also studies showing that the risk of developing GERD increases with H. pylori eradication therapy [10]. Results are contradictory, and therefore studies investigating the relationship between H. pylori and GERD have increased even more.
Aim
This study aims to investigate the relationship between symptoms and demographic data with endoscopic results of patients presenting with gastrointestinal complaints and the relationship between histological and topographic characteristics of H. pylori gastritis and the presence and severity of oesophagitis according to the biopsy results obtained from their endoscopy.
Material and methods
Our study included patients admitted to the outpatient clinic of the adult Gastroenterology Department of Kahramanmaras Sutcu Imam University Medical Faculty Hospital between September 2014 and February 2015 with dyspeptic complaints. Those who had previously received eradication therapy for H. pylori, had a history of previous gastrointestinal surgery/cancer, had diseases that could affect the study such as connective tissue disease (scleroderma etc.), and those with coagulopathy were excluded from the study. In total, 113 patients with heartburn and/or regurgitation complaints once a week or more were included in the GERD group and 58 patients with dyspeptic complaints other than these symptoms were included in the non-reflux group.
Approval for the study was granted by the local Ethics Committee (decision no. 29.09.2014/159-06), and the study was conducted according to the 1975 Declaration of Helsinki. The protocol of the study was explained to the patients, and their consent was obtained. Staging was performed according to Los Angeles (LA) classification if reflux oesophagitis was detected during oesophagogastroduodenoscopies (EGD). Two biopsies were taken from all patients within a 2-cm area adjacent to the pylorus in the antrum and from the large curvature in the corpus using standard-sized biopsy forceps. Histopathological evaluation was performed according to the Sydney system.
Statistical analysis
SPSS for Windows 21.0 statistical software was used for statistical calculations. The results were given as mean ± standard deviation (SD). Student’s t-test was used to compare numerical data. The χ2 test was used where appropriate to compare proportional data, and p < 0.05 was considered statistically significant.
Results
There were 113 patients in the GERD group and 58 patients in the non-reflux group. The mean age was 40 ±14 years in the GERD group and 49 ±16 years in the non-reflux group. The demographic data of the patients are summarised in Table I.
Table I
Demographic characteristics of the patients
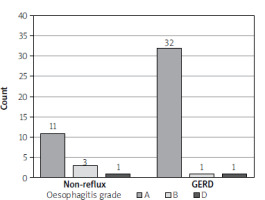
Endoscopic results were classified as antral gastritis, pangastritis, atrophic gastritis, gastric ulcer, and duodenal ulcer. No significant differences were found between the 2 groups in terms of endoscopic results (p > 0.05). Oesophagitis was detected in 34 (30%) patients in the GERD group and in 15 (25%) patients in the non-reflux group; however, this difference was not statistically significant (p > 0.05). There was no difference between the groups in terms of grading (p > 0.05) (Figure 1). In addition, no patients with stage C oesophagitis were found in either group.
Biopsy samples were examined for the presence of H. pylori, which was detected in 125 (73%) patients in total – 85 (75%) patients in the GERD group and in 40 (69%) patients in the non-reflux group. In the biopsy samples, the presence of H. pylori in the antrum and corpus, inflammation, activation, metaplasia, and atrophy grading were compared in both groups. Activation and inflammation in the antrum were more common in the GERD group compared to the non-reflux group whereas the rate of gland atrophy in the corpus was found to be higher (Table II).
Table II
Evaluation of gastritis parameters between groups
The relationship between the presence of H. pylori and gender was examined. Among the H. pylori-positive patients, 77 (75%) of the females and 48 (71%) of the males were infected with H. pylori and the difference was not statistically significant (p > 0.05). No significant relationship was found between the presence of H. pylori and educational status, smoking, alcohol habit, and chronic disease (p > 0.05). No significant relationship was found between endoscopic results and the presence of H. pylori when endoscopic results were classified as antral gastritis, pangastritis, atrophic gastritis, gastric ulcer, and duodenal ulcer (p > 0.05). Oesophagitis was present in 36 (29%) patients in the H. pylori-positive group and in 13 (28%) patients in the H. pylori-negative group; however, it was not statistically significant (p > 0.05). There was no significant relationship between H. pylori and grade according to LA classification (p > 0.05). The relationship between gastritis parameters and the presence of H. pylori was examined. Chronic active gastritis was observed more frequently in the H. pylori-positive group in the corpus (Table III).
Table III
The relationship between gastritis parameters and the presence of H. pylori
Discussion
Osophagitis was detected in 35% of 1421 patients diagnosed with GERD in a multicentre GERD study conducted in Turkey. It is stated that GERD is as common in Turkey as in the west, but it is generally mild [11]. Oesophagitis was detected 30% of the reflux group, and 94% were grade A in our study. There was no difference between the groups in terms of oesophagitis frequency. In addition, no significant difference was found between both groups in terms of hiatal hernia and oesophagitis grade. These results support the GORHEN study.
An inverse relationship was found between reflux oesophagitis and H. pylori in 2 separate studies involving the European and Korean populations [12–19]. Yalaki et al. found that H. pylori was lower in the group with reflux oesophagitis [20]. Contrary to these studies, it is also reported that Hp is not associated with reflux oesophagitis [21–23]. The symptoms of 64 patients before and after H. pylori eradication treatment were evaluated in a prospective study. It was observed that the symptoms did not change after eradication, and it was concluded that this situation was independent of H. pylori status [24]. It was shown in another study that H. pylori eradication did not affect the diagnosis and severity of oesophagitis [25]. The prevalence of H. pylori was 73% in our study, which is consistent with the literature. H. pylori was detected at a rate of 75% in the reflux group and 69% in the non-reflux group. There were no statistically significant differences.
H. pylori infection may induce both antrum-dominant and corpus-dominant gastritis, and gastric acid secretion may be affected by the severity and localisation of gastritis. In a study including 30 patients with a clinical diagnosis of GERD, the frequency of oesophagitis was found to be 23%, the frequency of H. pylori in the antrum was 73%, and the frequency of H. pylori in the corpus was 63% [26]. Dinçer et al. examined gastritis parameters and found that the prevalence of H. pylori was 63%, and the prevalence of H. pylori was lower in patients with intestinal metaplasia in cardia [27]. Ataseven et al. found that there was no significant relationship between the presence, severity, and distribution of H. pylori and oesophagitis stage. Chronic active gastritis and chronic atrophic gastritis were observed more frequently in the antrum compared to the corpus [28]. H. pylori was found to be lower in patients with GERD, antral gastritis was more common, and inflammation was more severe in a study involving the Asian population [29]. Nobakht et al. found no relationship between H. pylori and GERD in their study, but antral gastritis was significantly higher in the GERD group [30]. There was no relationship between H. pylori positivity in both the antrum and corpus and the presence and severity of oesophagitis in our study. Neutrophil activation and chronic inflammation in the antrum were more common in the GERD group compared to the non-reflux group whereas the rate of gland atrophy in the corpus was found to be higher. However, it was not statistically significant. Intestinal metaplasia was similar between both groups. Chronic active gastritis was detected more in the antrum and corpus in the H. pylori-positive group, and atrophic gastritis was detected more frequently in the antrum in the H. pylori-negative group when the relationship between gastritis parameters and the presence of H. pylori was examined.
Conclusions
The frequency of H. pylori in patients with GERD was found to be similar to that reported in the literature. No difference was observed between the antrum and corpus in terms of H. pylori frequency in the GERD group. Activation and inflammation in the antrum were more common in the GERD group compared to the non-reflux group whereas the rate of gland atrophy in the corpus was found to be higher. It was concluded that the type of histological gastritis that H. pylori creates rather than its presence may be associated with GERD. However, similar studies with a larger numbers of patients are required.