Introduction
Chronic spontaneous urticaria (CSU) is a chronic skin disease with the potential for natural remission. It is defined as itchy wheals and/or angioedema for at least 6 weeks. Within these patients, angioedema is characterized by an abrupt, pronounced erythematous or skin-colored swelling of local subcutaneous or submucosal tissue. It might be painful rather than itchy. Angioedema might persist for 72 h, and wheals typically resolve within 24 h. For most patients, symptoms can differ by the extent of the areas affected, the severity, and clinical presentation [1, 2]. The diagnosis of CSU is based on medical history and physical examination. It is necessary to learn about the onset time, symptom duration, frequency, timing, characteristics of lesions, different symptoms, family disease history, and previous therapies. It is important to acknowledge potential causes and triggers [1, 3]. The prevalence of CSU is 0.5–5%, and the female-to-male ratio is 2 [3–5]. It is considered that CSU is more common in adults with peak ages between 20 and 40 years old. The etiopathogenesis is complex with inflammation as one of the most important factors, but immune, hormonal, and genetic abnormalities are taken into consideration [6]. Unlike inducible urticarias, in CSU, the appearance of clinical manifestations is spontaneous and not evoked by physical and/or environmental stimuli, such as cold, heat, pressure, solar light, exercise, or contact with water [7, 8]. The risk of CSU is statistically significantly higher in patients with obesity, anxiety, and malignancies [9]. Urticaria might reduce the quality of a patient’s life and has been associated with disorders such as anxiety, depression, and sleep difficulties [10].
Cigarette smoking is one of the world’s major addictions. The average percentage of smokers in Poland is 26% [11]. The popularity of smoking depends on the gender of the respondents. One-third of men (31%) smoke cigarettes, 26% of whom smoke regularly. It is in contrast to women, of whom 21% smoke and 17% smoke regularly. The respondents between 45 and 54 years of age (35%) and between 55 and 64 (32%) smoke most often. In all age groups, men smoke more than women [12]. Both active and passive smoking may lead to the development of various diseases such as cardiovascular diseases, cancers, strokes, chronic obstructive pulmonary disease, rheumatoid arthritis, or Crohn’s disease. On the other hand, active or passive smoking may have a protective effect on ulcerative colitis, autoimmune hypothyroidism, or CSU [9, 12]. Asking about addictions, including smoking, is a routine element of a thoroughly conducted medical history. Some literature data indicate that smoking is a factor contributing to the exacerbation of urticaria symptoms. However, there are studies indicating a possible protective effect of smoking on the risk of CSU and other inflammatory and allergic processes through multiple mechanisms [9, 13, 14].
The neutrophil-to-lymphocyte ratio (NLR) is a good marker of inflammation and overall survival. It might be helpful in many diseases such as atherosclerosis, myocardial infarction, diabetes mellitus, or CSU. Some studies suggest that NLR may be used as an indicator of omalizumab treatment response in CSU patients. It represents both acute and chronic inflammation as well as adaptive immunity [15–20].
Taking into consideration that inflammation is involved in the pathogenesis of CSU, in the light of possible protective effect of smoking – our study aimed to check the prevalence of smokers in our CSU patients and to assess their profile of NLR as a marker of inflammation. Considering smoking as a protective factor, we hypothesized that the percentage of smokers in CSU patients should be lower in comparison to the general population. We were also expecting to find normal levels of NLR in smoking patients and higher in the non-smoking group.
Aim
To check the prevalence of smokers in our CSU patients and to assess their profile of NLR as a marker of inflammation.
Material and methods
In our research, we have analyzed the archival data of consecutive patients admitted to the Allergology Department of University Hospital in Opole from 2018 to 2021. The inclusion criterion was the diagnosis of CSU. The diagnosis was established according to the international EAACI/GA2LEN/EuroGuiDerm/APAAACI guideline [1]. Each patient underwent an extensive interview. Family history of similar conditions, previous episodes of urticaria, and any other allergic or autoimmune disorders were also noted. Laboratory investigations were made, i.e.:
complete blood count (CBC): to evaluate basic hematological neutrophils (NEU), lymphocytes (LYM), and NLR.
C-reactive protein (CRP): these were measured to assess systemic inflammation, which can point to underlying infections or autoimmune disorders.
Thyroid function tests: given the association between thyroid autoimmunity and CSU, anti-thyroid peroxidase (anti-TPO) levels were assessed to rule out.
IgE levels: total serum IgE was tested to identify any immediate hypersensitivity reactions.
Each patient admitted to the Department underwent a chest X-ray and ultrasonography of the abdomen. Patients were screened for infections that could mimic or exacerbate urticaria, including viral hepatitis, Helicobacter pylori, and other chronic infections. A detailed review of recent medication use was also conducted to rule out drug-induced urticaria. Physical triggers such as pressure, temperature changes, water contact, vibration, and sunlight were systematically evaluated through patient history and, when necessary, provocation tests, to rule out inducible forms of urticaria.
Patients with a history of mastocytosis, asthma, corticosteroid intake, or use of non-steroid anti-inflammatory drugs 7 days before admission were excluded. There were 2 patients excluded from the study because of the lack of information on smoking history. Overall, 68 adult patients were included. The group was divided by gender and smoking. 52 patients from the studied group were females, and 16 were males. The youngest person was 20 years old, and the oldest was 89. The average age of respondents was 52.
Results
73.5% of the respondents were non-smokers, and the remaining 26.5% were smokers. Among the group of women, 40 of them (76.9%) denied smoking. The remaining 12 (23.1%) women who smoked were between 20 and 69 years old (mean age: 50). Out of the male group, 10 patients (62.5%) denied smoking. The smokers’ age ranged between 32 and 67 years old (mean age 49).
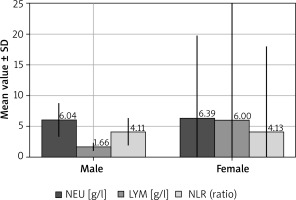
In the female group, irrespective of smoking, statistically significant different levels of NEU, LYM, and NLR were found compared to males (Figure 1).
Figure 1
Levels of neutrophils (NEU), lymphocytes (LYM) and neutrophil-to-lymphocyte ratio (NLR) in chronic spontaneous urticaria (CSU) patients (p < 0.05)
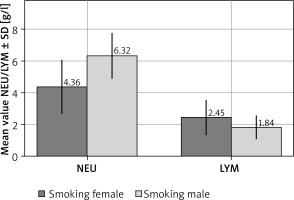
No statistical difference was found between smokers and non-smokers regarding the level of NEU, LYM, or NLR. Compared to males, females had significantly different levels of LYM in the group of non-smokers (Figure 2) and NEU in the group of smokers (Figure 3).
Figure 2
Levels of neutrophils (NEU) and lymphocytes (LYM) in non-smoking chronic spontaneous urticaria patients. NEU (p = 0.4), LYM (p < 0.05)
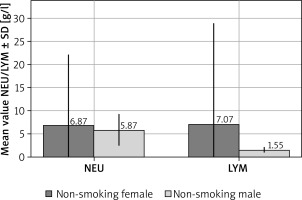
Figure 3
Levels of neutrophils (NEU) and lymphocytes (LYM) in smoking chronic spontaneous urticaria patients. NEU (p < 0.05), LYM (p = 0.34)
Whether females were smoking or not, they had quite different levels of NLR (Figure 4). No statistical difference was found between smokers and non-smokers regarding the level of CRP (Figure 5).
Figure 4
Levels of neutrophils (NLR) in chronic spontaneous urticaria patients considering smoking and gender. NLR (p < 0.05)
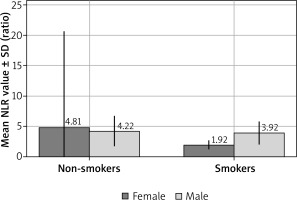
Figure 5
Levels of C-reactive protein (CRP) in chronic spontaneous urticaria patients considering smoking and gender. CRP (p > 0.05)
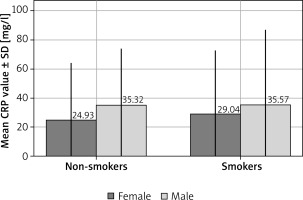
There were no statistical differences between smokers and non-smokers without distinction of gender in the level of CRP, NEU, LYM, and NLR.
Discussion
In our studied group the prevalence of smoking was 26.5%, whereas the average percentage of smokers in Poland is 26% [11]. The percentages are quite similar in our CSU patients and in the general population of Poland.
We did not find a statistical difference in NLR between smoking and non-smoking CSU patients, but there was a statistically significant difference in the level of NLR in female smoking vs. female non-smoking patients. NLR was slightly higher (with statistical significance) in the female group compared to males, regardless of smoking.
NLR is an increasingly used indicator of inflammation. In our study, we chose it as the factor for assessing inflammation due to its simplicity, ease of calculation, and frequent performance of CBC tests for various indications. This choice allows for a direct assessment of inflammation, especially in clinical settings where rapid assessment is crucial, without the need to perform more complex calculations required by indicators such as the Systemic Inflammation Response Index (SIRI) or the Systemic Immune-Inflammation Index (SII). The normal value of NLR is not fully established, but according to studies, it is 1–3 (2–3 is also sometimes indicated as the “grey zone”) and depends on age and gender [20]. Females between the ages of 30 to 49 tend to have higher NLR, whereas males between the ages of 60 to 69 have higher NLR [4, 21, 22]. In our research, the group of women consisted of 52, of whom 40 were non-smokers. Females who smoke ranged from 20 to 69 years of age. Non-smoker females ranged from 20 to 89 years of age.
Taking NLR values of 1-3 as the normal range, the only group within the proposed range is smoking women (non-smoking females NLR was 4.81, whereas smoking females NLR was 1.92).
We hypothesize that elevated lymphocyte levels in non-smoking females may be associated with the immunomodulatory effects of estrogen, which favors a Th2-dominant immune response [23]. Estrogen induces the proliferation and activation of T and B lymphocytes, which may account for the higher LYM levels observed in this group [24]. However, these differences are likely the result of a complex interplay of hormonal influences, differential cytokine receptor expression, and other sex-specific immunological factors. The increased neutrophil counts observed in smoking males may be attributed to the pro-inflammatory effects of smoking, which, in conjunction with androgen-stimulated hematopoiesis, may lead to enhanced neutrophil mobilization [25]. Smoking-induced cytokine release, including TNF-α and IL-6, further promotes neutrophil production and activation, which could explain the higher NEU levels in males compared to females [26].
Nowadays nicotine is used in the experimental treatment of many diseases such as ulcerative colitis, Alzheimer’s disease, and Parkinson’s disease. The protective effect of this alkaloid is proven in some studies in conditions such as ulcerative colitis, rheumatoid arthritis, and chronic spontaneous urticaria. Scientific data support the anti-inflammatory effect of nicotine, but the mechanism behind it is still not entirely known [12, 22, 27–29]. The increase in NLR is noticeable when it comes to smokers – neutrophil/lymphocyte ratio increases in correlation with pack/year [30].
In contrast to NLR we did not find statistically significant differences between levels of CRP (Figure 5), which was used as another inflammatory marker. An elevated level of CRP can be found in many diseases associated with inflammation, for example in autoimmune and allergic diseases. In the course of CSU, CRP can also be elevated during the onset of disease symptoms.
The limitations of our study were the lack of a control group, a small research group, lack of other inflammatory parameters such as ESR or fibrinogen, and the fact that we could not confirm if the patients were active or passive smokers by performing laboratory tests. What is more, we did not analyze the data in terms of severity and duration of the disease (e.g. by collecting Urticaria Activity Score or Urticaria Control Test), which could be interesting to be done in further studies.
It can be concluded that the prevalence of cigarette smoking in our CSU patients is similar to the general population. The statistical analysis performed does not confirm the claims from the literature data that smoking reduces the course and the incidence of chronic spontaneous urticaria. Significant differences in NEU, LYM, and NLR between males and females and lower NLR in smoking female patients need further investigation and might support the concept of inflammation as an important factor (trigger) in CSU pathogenesis.
A better understanding of the mechanism of CSU formation allows faster detection of this disease and the implementation of appropriate treatment, so further studies are required.








