Penetrating injuries to the thoracic cavity constitute a relatively frequent occurrence in hospital emergency departments, often stemming from incidents involving bullets, knives, or other sharp objects. The severity of such thoracic injuries is contingent upon both the mechanism of injury and the specific intrathoracic organ affected [1]. Conversely, the retention of a foreign body subsequent to a penetrating thoracic trauma is a rare clinical phenomenon. Diagnosis of these retained foreign bodies can pose challenges, with instances where these objects remain asymptomatic within the thoracic cavity. Nevertheless, early diagnosis and intervention are imperative to preempt potential complications [2]. This study presents a case involving a patient who, following self-inflicted thoracic trauma with a broken bottle, was transferred to our hospital in a stable condition. Radiological examination identified a retained bottle fragment, prompting intervention through minimally invasive video-assisted thoracic surgery (VATS) for its extraction. The present case underscores the significance of prompt diagnosis and targeted intervention in managing such unique clinical scenarios. A 19-year-old male patient presented with a self-inflicted stab wound to the anterior chest wall, inflicted during a dispute with his partner (Figure 1). In a remote location, he sought medical assistance from a local nurse, revealing an open sucking chest wound on the right anterior chest wall, situated medio-cranially to the nipple. Following the application of a 3-sided occlusive dressing, the patient was subsequently transported to the regional hospital. Chest X-ray assessment revealed a pneumothorax on the right side, prompting the insertion of a chest tube and closure of the chest wound with sutures. A computed tomography (CT) scan of the thorax was subsequently requested due to a suspicious opacity observed over the right-sided costodiaphragmatic angle on X-ray. The CT scan (Figures 1 and 2 A, B) revealed a triangular-shaped foreign body located in the right base of the pleural space. The patient was subsequently transferred to our unit, where a right-sided VATS procedure was performed. Intraoperatively, a shard of the beer bottle (Figure 2 C) was identified and safely removed using ring forceps. The pleural cavity underwent thorough irrigation with warm saline, and prophylactic antibiotics were administered. The postoperative course remained uneventful, with chest drain removal on day 3, leading to the patient’s discharge from the hospital. Follow-up after 2 weeks revealed a healed wound and incision sites, as well as a normal chest X-ray. This case underscores the successful application of VATS in the comprehensive management of a penetrating thoracic trauma involving a retained foreign body. Chest stab wounds, resulting from various sharp objects such as knives, daggers, and sharp glass, present diverse wound shapes and intrathoracic injuries depending on the penetrating object’s shape and the injury mechanism [1]. Intrathoracic foreign bodies are systematically categorized based on their location within the thoracic region [3]: intrapulmonary site, endobronchial site, within the thoracic cavity outside the lungs and bronchi.
Figure 1
A – Schematic representation of the injury mechanism illustrating the penetration of the thoracic cavity by a sharp broken bottle. B – Sagittal reconstruction of the CT scan reveals the residual broken glass fragment in the thoracic cavity (arrow)
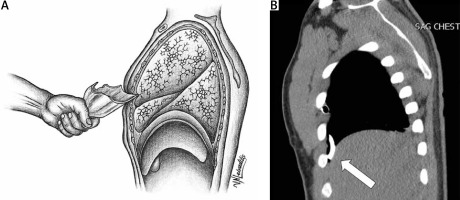
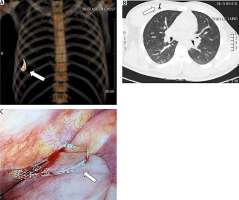
Figure 2
A – 3D reconstruction depicting the location of the retained broken glass foreign body in the thoracic cavity (arrow). B – Transverse CT scan view displaying the penetrating injury in the anterior thoracic wall (arrow). C – Intraoperatively observed intrathoracic glass fragment during thoracoscopy
Notably, foreign bodies in the mediastinum are excluded from this classification [3]. Thoracic trauma, particularly involving tracheobronchial foreign bodies, ranks among the most common emergencies, carrying an international mortality rate of 0.42% [4]. Injuries to the visceral pleura and lung parenchyma may lead to life-threatening complications such as tension pneumothorax, emphasizing the significance of immediate three-sided wound dressing in the initial aid stage [5]. Intercostal vessel or intrapulmonary vessel injuries pose risks of hemothorax and hypovolemic shock [1]. In emergency departments, chest X-rays are routinely performed after initial clinical evaluations of patients with thoracic penetrating trauma, offering valuable information [1, 2]. Glass, however, presents distinct radiographic characteristics, influencing its visibility on X-rays based on location, depth, surrounding tissue, and object density. This complexity often necessitates the application of CT scans for enhanced sensitivity in detecting these objects [3, 6, 7]. Digital image processing has further demonstrated the capability to visualize even minute glass fragments undetectable by plain radiography [8]. For hemodynamically stable patients, thoracic CT scans have become the gold standard, essential for evaluating intrathoracic organ injuries and detecting free foreign bodies [1, 9, 10]. The expanding use of ultrasound in trauma centers has facilitated the early diagnosis of traumatic pneumothorax, hemothorax, and, potentially, intrathoracic foreign bodies upon patient admission to the emergency department [11]. Flexible bronchoscopy is recommended as the primary procedure for managing adults with tracheobronchial foreign bodies [9, 12]. The treatment of hemodynamically stable patients with free intrathoracic foreign bodies poses a clinical challenge, navigating clinicians through a therapeutic dilemma. Aggressive extraction is discouraged for smaller asymptomatic metal pieces, measuring 2 cm or less [7, 8]. However, extraction is warranted for larger metal pieces and non-metal objects, such as sharp glass fragments [7]. The formation of fibrous tissue around foreign bodies may limit inflammatory reactions, reducing the risk of infection and obviating the need for unnecessary surgery [2]. Conversely, freely moving foreign bodies within the thorax may pose risks of injuring other intrathoracic structures or leading to infections that necessitate surgical removal [10, 13]. Thoracoscopy, particularly VATS, has emerged as a fast, feasible, and effective method for foreign body removal from the thoracic cavity, often obviating the need for thoracotomy [3]. VATS, characterized by its minimally invasive nature, has become the standard of care in thoracic trauma operations. It allows simultaneous evaluation and management of complications, diaphragm injuries, and pleural cavity drainage through port insertions, resulting in reduced postoperative pain and shorter hospital stays [8]. In the present case, a diagnostic and therapeutic minimally invasive VATS procedure was successfully performed, enabling the simultaneous inspection of intrathoracic organs and the removal of a glass fragment. The meticulous washing of the chest with warm saline and the administration of perioperative prophylactic antibiotics proved effective in minimizing the risk of infection and contributed to a favorable postoperative course. This case underscores the utility of VATS in managing penetrating thoracic trauma involving retained foreign bodies. Looking ahead, advancements in imaging technologies, such as improved CT capabilities and the expanding role of ultrasound, hold promise for enhancing the diagnostic accuracy and efficiency in cases of intrathoracic foreign bodies. Additionally, continued research into the long-term outcomes and potential complications associated with conservative management versus aggressive extraction strategies will further guide clinicians in navigating the complexities of treating patients with retained intrathoracic foreign bodies. The integration of evolving technologies and evidence-based practices will likely continue to shape the landscape of thoracic trauma management, offering refined approaches for optimizing patient outcomes. This case report sheds light on several crucial learning points in the context of penetrating thoracic trauma involving retained foreign bodies. Firstly, it underscores the potential retention of fragile materials such as glass as foreign bodies within the thoracic cavity, highlighting the importance of considering diverse materials when assessing intrathoracic injuries resulting from assaults. Secondly, the significance of a comprehensive understanding of the injury’s history and the mechanism of injury is paramount. The careful consideration of these factors plays a pivotal role in guiding the diagnostic process, aiding in the identification of potential intrathoracic foreign bodies. Thirdly, the case underscores the pivotal role of surgery, particularly thoracoscopy, as the first-line treatment for cases involving retained intrathoracic foreign bodies. Thoracoscopy not only facilitates a thorough inspection of intrathoracic structures but also enables the safe removal of the foreign body. Furthermore, the meticulous approach of thoracoscopy contributes to minimizing the risk of perioperative infections, emphasizing its role as a comprehensive and effective therapeutic intervention. In conclusion, the present case underscores the importance of a multidimensional approach in managing cases of penetrating thoracic trauma with retained foreign bodies. Integrating knowledge about the nature of materials used in assaults, understanding the injury’s history, and prioritizing surgical interventions such as thoracoscopy collectively contribute to optimal patient outcomes. The lessons gleaned from this case provide valuable insights for clinicians involved in the care of patients with similar thoracic injuries.






