Temporary epicardial pacing wires (TEPWs) have been routinely inserted in all patients undergoing cardiac surgery since the 1960s. The main purposes were, and still are, therapeutic and diagnostic, as they are mainly used to recognize and treat ventricular and/or atrial rhythm disturbances that may be a complication of cardiac interventions and to sustain the possible hemodynamic instability during post-operative intensive care [1]. However, their necessity is often discussed as their use is linked to several but unlikely complications such as cardiac tamponade and hemorrhage at the time of removal [2], or infection, wound dehiscence and migration when retained [3].
The indications for insertion of the TEPWs are several: conduction abnormalities such as AV block, prolonged AV delay, bifascicular block; bradycardia and tachycardia, especially atrial fibrillation, which is common in the period following cardiac surgery; and the need to place both atrial and ventricular wires is often dependent on the patient; furthermore, the pacing system should be checked and reassessed routinely based on the patient’s condition. The removal must be done carefully by gentle and constant traction; if too much traction is needed as they may have been caught in a tight suture, they should be cut as close to the skin as possible due to the risk of tamponade immediately after the removal procedure. For this reason, it is necessary to observe the patient and perform echocardiography a few hours after the removal [1]. Although there is a risk of hemorrhage and cardiac tamponade, to cut the wires flush with the skin is not a procedure free of adverse events such as infection and migration.
An 89-year-old woman with severe aortic stenosis and aneurysm of the ascending aorta, with medical history of hypertension, dyslipidemia, obesity and chronic renal failure, underwent aortic valve replacement with a Sorin Mitroflow 21 bioprosthesis and of the ascending aorta with an Intervascular 28 prosthesis, requiring circulatory arrest during the procedure on September 2014. In the immediate post-operative period, due to massive bleeding and hemodynamic instability, it became necessary to conduct a surgical revision of the mediastinum. Two right atrial and two right ventricular epicardial pacing wires were inserted at the moment of the intervention and were not removed during the revision of the mediastinum; on the 6th postoperative day (POD), at the time of removal, only the ones placed on the right ventricle were removed without resistance, while the ones on the right atrium were cut flush with the skin. On the 8th POD, the patient presented strong chest pain, erythema and drainage from the distal third of the sternotomy wound associated with sternal instability; on the 10th POD she became feverish and blood cultures tested positive for Proteus mirabilis and Staphylococcus epidermidis. Despite antibiotic targeted therapy there was progressive enlargement of the dehiscence and vacuum assisted closure (VAC) therapy was started. Several swabs of the wound were performed, and when they tested negative for bacterial growth, the patient underwent reconstruction of the dehiscent wound through partial mobilization of pectoralis muscles. The remaining in-hospital stay and follow-up were uneventful and the wound perfectly healed. Four years later, she came back due to the appearance of a painful swelling at the distal third of the sternotomy wound, approximately 30 mm wide; thus, empirical antibiotic therapy was started as well as serial medications of the swelling. A week after the antibiotic therapy was started, the swelling in her upper abdomen increased in volume and started to drain purulent fluid; another swab was performed and tested positive for Proteus mirabilis; therefore targeted antibiotic therapy with ciprofloxacin (500 mg/day) was started (Figure 1).
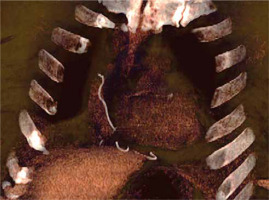
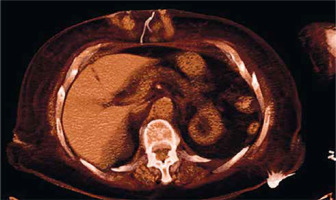
The patient did not develop fever but her blood count showed the normal range of hemoglobin, 11 g/dl, increase of white blood cell count, 12,500 per µl, and C-reactive protein level of 70 g/l. As the swelling kept draining and growing despite antibiotic therapy and serial medication, the patient was hospitalized once again in January 2019 to remove the granuloma surgically. During the post-operative follow-up the wound initially presented with a superficial dehiscence that eventually reached the deep edges of the wound; therefore a computed tomography (CT) scan was performed and it revealed the presence of a foreign body in the patient’s mediastinum which appeared to be the retained TEPWs (Figures 2–4).
Figure 2
Computed tomography (CT) scan images of the retained wires in the subcutaneous tissues of the patient (axial plane)
It was then decided to schedule her admission in order to remove the retained wires safely, but eventually, 7 days before the hospitalization the epicardial wires exited spontaneously through her upper abdomen by doing gentle compression of the area by herself. A few days after the extrusion, the wound healed completely with only a few medications needed (Figure 5).
The insertion of temporary epicardial pacing wires is common practice in cardiac surgery as they are found to be helpful in the immediate post-operative care of the patient by sustaining hemodynamics, optimizing cardiac function, to avoid brady-arrhythmias and conduction blocks, which may be common especially in valve replacement procedures, or even tachy-arrhythmias, both potentially life-threatening. The pacing wires may be sutured both to the right atrium and the right ventricle, but in certain circumstances, based on the rhythm and hemodynamics of the patient at the end of the cardiopulmonary bypass, they can be placed just upon one of the right cardiac chambers. The main reason for not positioning the TEPWs is not only related to the actual need of a safe way to treat post-operative arrhythmias, but it is also related to the risks related to their removal. The removal should be done approximately on the 4th–5th POD, when the hemodynamic and rhythm stability of the patient is assessed. The procedure consists in a gentle but constant traction, but it can lead to damage of the cardiac chambers at the moment of detachment, damage of venous/arterial grafts [4] or even of the tissues through which the wires will pass during the removal. This can cause mainly bleeding, which sometimes can be massive and lead to cardiac tamponade, with the necessity of a surgical revision of the mediastinum in order to drain the pericardial effusion, repair any damage sustained during the extraction and also to stop the bleeding. This is the main reason why the procedure should be done carefully, paying attention to any resistance encountered during the traction, monitoring the rhythm of the patient and being able to decide at any moment whether to keep applying traction or to cut the wires flush with the skin and let them retract inside. However, cutting the TEPWs flush with the skin is not a procedure free of risks, as the retained epicardial wires can cause infection and can migrate, probably due to the constant movement of the heart and the diaphragm. In the literature several cases of migrating retained pacing wires have been reported: some migrated into the aortic arch [4], others into abdominal aortic aneurysms [5] and the left heart [6]. There are also case reports of accidental encounter of TEPWs during elective colonoscopy [7], stomach migration causing dyspepsia [8] and wires exiting from the jaw of a patient [9, 10]. Sometimes the retrieval is by accident; other times the retention and migration can lead to more serious consequences, as in the clinical case reported by Horng et al. [11], in which the retained wires migrated to the upper lobe of the right lung of the patient, causing severe dyspnea. Furthermore, 2 cases of prosthetic valve endocarditis caused by retained wires were reported [11, 12]. In the case of our patient, the wires did not actually lead to major events for the patient, and their spontaneous exit solved the wound healing problems related to their retention. In our center we routinely insert atrial and ventricular or epicardial TEPWs in valve surgery; in patients undergoing coronary artery bypass graft surgery procedures we usually insert two ventricular temporary pacing wires, although it depends on the rhythm at the end of the cardiopulmonary bypass, as it may be necessary to insert both atrial and ventricular wires, and although removal is the preferable option, in a small percentage of cases (2%), due to resistance to traction, we cut them flush with the skin. In our experience the small percentage of patients with retained TEPWs do not have infective issues such as mediastinitis or local wound dehiscence. In conclusion, although their removal is not free of risk for the patient, cutting the TEPWs flush with the skin is not always a safe procedure; it should then be recommended to make a safe and cautious attempt at their removal before deciding to cut them, as one cannot know the fate of the epicardial wires throughout the life of the patient [13].