Introduction
Thyroid cancer is one of the most common cancers among women in Korea and bilateral axillo-breast approach (BABA) thyroidectomy is a minimally invasive surgical technique widely used for thyroid cancer with great cosmetic effects. Minimally thyroidectomy has two surgical techniques, the bilateral axillo-breast approach and transaxillary approach. In Korea, both techniques are safe and widely used by endocrine surgeons [1]. However, in BABA thyroidectomy, postoperative pain at the flap site is one of the most clinically significant issues complained of by many patients. To reduce postoperative pain, analgesics are administered to the flap site perioperatively. Ryu et al. [2] reported that 55 patients undergoing BABA thyroidectomy had anterior chest pain. Although patient-controlled intravenous analgesia (PCIA) after surgery shows strong analgesic effects, high doses can have a higher incidence of adverse events such as nausea, vomiting, excessive sedation, and dizziness. Therefore, analgesia with lower doses would be beneficial for postoperative pain. However, studies evaluating the safety of low-concentration ropivacaine infiltration in thyroidectomy are lacking.
Ropivacaine infiltration with local analgesic into the surgical flap site is an inexpensive method that reduces the use of additional analgesics and is effective, with a reduced rate of major adverse events. Ropivacaine is a long-acting analgesic agent widely used in surgical anesthesia and acute pain management. A systemic review examining the effect of ropivacaine infiltration in thyroidectomy concluded that ropivacaine infiltration into the surgical flap site was effective in reducing pain. With relatively low adverse event rates, ropivacaine is injected for postoperative pain control in various types of surgery. In recent years, evidence has supported the effectiveness of ropivacaine infiltration into the surgical site. It can be delivered in various ways, such as by diluted infiltration, sprayed at the flap site without dilution, and continuous infiltration, according to operator preference, without major concerns for serious adverse events. Jarna et al. [3] reported that ropivacaine has been used successfully for decades via routes that included neuraxial, perineural, intravenous, and infiltration. In the case of thyroidectomy, the method of ropivacaine infiltration depends upon the preference of the surgeon. Whether ropivacaine infiltration occurs pre-incisionally or postoperatively is also controversial.
However, high concentrations of ropivacaine can produce adverse events in the central nervous system and cardiovascular system. Toxic blood concentrations can depress cardiac conduction and lead to cardiovascular events. Thyroidectomy can be vulnerable to motor nerve blocks because the recurrent laryngeal nerve is exposed. Since a motor nerve block can be induced at high concentrations, high concentrations of ropivacaine that would result in serious adverse events should be avoided. Thus, if possible, it is better to use a lower dose of ropivacaine. To date, limited studies have compared postoperative outcomes between high and low concentrations of ropivacaine in thyroidectomy patients.
Aim
Therefore, in this study we performed a retrospective review of patients who underwent BABA thyroidectomy performed by a single surgeon. The safety of low-concentration ropivacaine infiltration was evaluated by comparing adverse events in patients who received low-concentration ropivacaine infiltration with those who received high-concentration ropivacaine infiltration, and determining the efficacy of pain control by pre-incisional ropivacaine infiltration after propensity score matching (PSM) analysis.
Material and methods
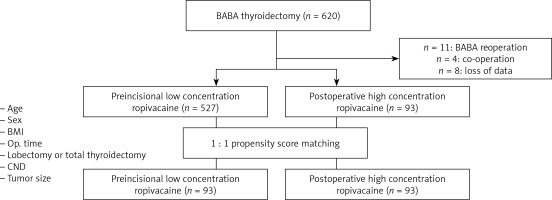
This retrospective study was approved by the local ethics committee, the Institutional Review Board of Samsung Medical Center (No. 2022-02-007). The study included patients who were 20–79 years of age. We reviewed medical data from a database of adult patients who underwent BABA thyroidectomy at Samsung Medical Center between June 1, 2017, and October 31, 2021. We classified the patients into two groups based on the ropivacaine infiltration dose: the pre-incisional low-concentration ropivacaine infiltration group and the postoperative high-concentration ropivacaine infiltration group. Patients were excluded if they had undergone reoperation on the same site, if data were missing, or if they had undergone two operations on the same day. The demographic data (age, weight, height) and clinical characteristics (operation methods/type, central neck dissection, extent of surgery, tumor size) of all patients were analyzed. Any information related to personal identification was deleted before analysis.
The primary outcome was the incidence of ropivacaine-related adverse events (nausea, vomiting, dizziness, bradycardia, urinary retention, and allergic reactions) during the hospital day. The hypothesis was that low-concentration ropivacaine would lead to a lower incidence of ropivacaine-related adverse events. Bradycardia was defined as a slow heart rate of fewer than 60 beats per minute in the resting state. Nausea, vomiting, and dizziness were retrospectively reviewed through the nurse’s notes in the electronic medical record.
The secondary outcomes were the total amount of opioids consumed during the hospital day and pain intensity indicated by visual analog scale (VAS) scores during the first 24 postoperative hours and other postoperative outcomes. We compared VAS scores between the two groups to compare the pain control effect between pre-incisional low-concentration ropivacaine infiltration and postoperative high-concentration ropivacaine infiltration. To investigate the total amount of opioids used, we used an opioid conversion calculator and changed the dose of injected opioids to that of hydromorphone.
All patients underwent BABA robotic or endoscopic thyroidectomy. Thyroid surgery was performed according to a standardized procedure by a single surgeon. In the group of patients with injections of pre-incisional low-concentration ropivacaine-epinephrine, the surgeon injected 150 mg of ropivacaine and 1 mg/ml of epinephrine diluted 1 : 200,000 that was mixed with 100 ml of normal saline into the flap site before the incision was made. The group of patients with injections of high-concentration ropivacaine received only 1 mg/ml of diluted epinephrine infiltration into the flap site before the incision was made and 150 mg of undiluted ropivacaine into the flap site after surgery. Thus, the low concentration of ropivacaine was half that of high-concentration ropivacaine.
After the surgery, pain scores were assessed using the VAS (0, no pain; 10, worst imaginable pain). In the post-anesthesia care unit (PACU), patient VAS scores were obtained immediately after surgery. Opioid was administered when the pain score at rest was 4 or higher. In the ward, patient pain scores were evaluated every 6 h. During the hospital day, the patients in both groups received oral acetaminophen at 650 mg three times a day for postoperative pain management.
Statistical analysis
PSM was used to reduce or minimize selection bias and confounding biases. Propensity scores were estimated by multivariable logistic regression, which included seven variables (age, sex, body weight index, operation time, surgery method (lobectomy or total thyroidectomy), central neck dissection, and tumor size) that might affect postoperative outcomes. We performed 1 : 1 matching within a caliper with 0.2 SD of the value, excluding unmatched cases. Demographic and clinical parameters were assessed by calculating frequencies (%) for the categorical variables and means ± standard deviation for continuous variables. Student’s t-test or the Mann-Whitney U test was used for continuous variables and proportions. The χ2 test or Fisher’s exact test was used for the categorical variables. Comparisons of VAS scores between the groups were performed using repeated measures analysis of variance (ANOVA). For all tests, a p-value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 27.0 (IBM Corp., Armonk, NY, USA).
Results
Between June 1, 2017, and October 31, 2021, after excluding 13 patients (Figure 1), a total of 620 patients in the pre-incisional low-concentration ropivacaine infiltration group (n = 527) and the postoperative high-concentration infiltration group (n = 93) were statistically analyzed. Table I shows the demographic characteristics, clinical characteristics, and surgical outcomes of the study population before and after PSM. PSM minimized differences for most variables.
Table I
Baseline demographic and clinical characteristic
Before PSM, more patients (n = 418) (79.3%) in the low-concentration ropivacaine group underwent endoscopic thyroidectomy, whereas more male patients (n = 14) (15.1%) underwent BABA thyroidectomy in the high-concentration ropivacaine group. There were no significant differences in age, body weight index, operation time, central node dissection, or tumor size between the two groups after PSM.
As primary outcomes, the incidence of ropivacaine-related adverse events was compared between the two groups. The results are shown in Table II. The number of hospital days was quite high because, in Korea, most of the medical expenses charged to patients are paid by insurance, so patients prefer to stay in the hospital for a long time. Neither hospital day, the amount of drainage, nor the incidence of hypocalcemia was significantly different between the two groups. Regarding ropivacaine-related adverse events, the incidence of postoperative nausea and vomiting, headache, dizziness, and urinary retention was not significantly different between the two groups. However, the high-concentration ropivacaine group showed more bradycardia than the pre-incisional low-concentration ropivacaine group (25 (26.9%) vs. 14 (15.1%), p = 0.048). The incidence of serious adverse events was similar and low in both groups.
Table II
Postoperative outcome after propensity score matching
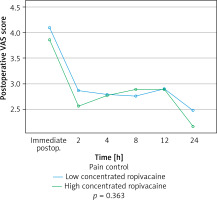
Table III and Figure 2 show pain-related outcomes. As a secondary outcome, PACU pain scores (VAS scores) were obtained to evaluate the immediate postoperative pain control effect in the pre-incisional low-concentration ropivacaine group. In the PACU, immediate postoperative pain scores were similar between the two groups. In addition, after converting the total opioid dose to a hydromorphone dose using an opioid conversion calculator, the total opioid consumption during the hospital day showed no significant difference between the two groups. Postoperative pain scores in the first 24 h after surgery were not significantly different between the two groups (p = 0.363). The highest score was found immediately postoperatively and the lowest was found 24 h postoperatively.
Discussion
Although ropivacaine is an effective analgesic agent at a relatively low dose, patients can experience adverse events. Ropivacaine infiltration is a simple and easy technique for postoperative pain control. Avoiding unnecessarily high doses is strongly recommended to prevent adverse events. Ropivacaine can affect the cardiovascular and central nervous systems. It can induce arrhythmia and sensory and motor nerve blocks. In the case of thyroidectomy, the recurrent laryngeal nerve is exposed during the procedure when the thyroid is removed. Thus, recurrent laryngeal nerve palsy should be kept in mind when using high-concentration ropivacaine infiltration. Many surgeons use postoperative high-dose ropivacaine infiltration and we previously used postoperative high-dose ropivacaine at Samsung Medical Center. However, after receiving advice from the anesthesiologist that high-dose ropivacaine could affect the motor nerves, we changed to using low-dose ropivacaine. Ropivacaine shows characteristic analgesic effects 30 min after administration, which are maintained for 2–6 h. Therefore, we decided that preoperative infiltration rather than postoperative infiltration would help reduce pain immediately after surgery and started to use preoperative low-dose ropivacaine infiltration.
To the best of our knowledge, this was the first study to evaluate the efficacy and safety of low-concentration ropivacaine infiltration compared to high-concentration ropivacaine infiltration for thyroidectomy. Several clinical studies have confirmed the efficacy of ropivacaine infiltration at the flap site during thyroid surgery. Kang et al. [4] reported that 3 ml/kg ropivacaine infiltration at the flap site with normal saline can successfully reduce the postoperative VAS score in 34 patients. Lee et al. [5] compared pre-incisional infiltration with 225 mg of ropivacaine in normal saline in 73 patients undergoing BABA thyroidectomy. They found that pre-incisional ropivacaine infiltration effectively reduced postoperative pain without vital sign disruption. Bae et al. [6] described a postoperative infiltration technique, which resulted in successful pain control in patients who underwent BABA thyroidectomy.
Comparisons between infiltration and non-infiltration in other types of surgery have also been made. Several studies have attempted to evaluate the pain control efficacy of ropivacaine in procedures other than thyroidectomy. Ye Tian explored the analgesic effects of ropivacaine for transversalis fascia plane (TFP) block during laparotomy. Wang et al. [7] reported that ropivacaine infiltration at the drainage exit site decreased the degree of postoperative acute pain after mastectomy. Cavallaro et al. [8] stated that trocar site infiltration was effective for postoperative pain management after laparoscopic adrenalectomy. Beguinot et al. [9] observed that ropivacaine infiltration in the surgical site reduced acute postoperative pain in patients undergoing mastectomy for breast carcinoma.
However, whether the pre-incisional or postoperative infiltration of ropivacaine is effective for postoperative pain control in thyroidectomy remains controversial. The superiority of the pre-incisional infiltration of ropivacaine remains unclear. In our study, we confirmed that pre-incisional infiltration had a painkilling effect similar to that of postoperative infiltration.
A few previous studies have compared different doses of ropivacaine in various types of surgery. Liang et al. [10] compared different concentrations of ropivacaine infiltrations for patients with laparoscopic cholecystectomy and suggested that high-concentration ropivacaine is not necessary for infiltration and that dilution was needed. Niiyama et al. [11] compared the continuous infiltration of 0.2% ropivacaine with a single infiltration of 0.75% ropivacaine in patients undergoing microtia reconstruction surgery. Lee et al. [12] also compared low-concentration ropivacaine and high-concentration ropivacaine in transverse abdominis plain blocks in pediatric open inguinal hernia repair. Han et al. [13] and Tian et al. [14] reported the analgesic effects of different ropivacaine concentrations in patients undergoing hip replacement and laparotomy. Previous studies reported that 0.75% ropivacaine was within the safety limits. However, the optimal dose of ropivacaine remains unknown. We tried to compare different ropivacaine infiltration doses in our study.
Finally, our study had several limitations. First, it had a retrospective design with a limited sample size. Although we tried to minimize this limitation by PSM, some biases due to data error might remain. In addition, the statistical power might be insufficient due to the limited sample size. Second, differences in injection timing could generate some biases. Third, the two populations were separated in time. Changes in general patient management have occurred over time. Moreover, the effectiveness of ropivacaine might be different for populations with different genders, ages, and extent of surgery. To overcome these limitations, a randomized controlled study needs to be conducted.
Nonetheless, this study has implications for clinical use. Our results can help surgeons alleviate postoperative pain by using 0.75% ropivacaine with epinephrine infiltration without much concern for serious adverse events. Our results also revealed that pre-incisional low-concentration ropivacaine infiltration could be used more safely than high-concentration ropivacaine infiltration in regard to adverse events. Moreover, patients given pre-incisional low-concentration ropivacaine infiltration reported pain scores similar to patients given postoperative high-concentration ropivacaine. Thus, it was not inferior to high concentrations for postoperative pain control and had a capacity similar to high-concentration ropivacaine infiltration for controlling postoperative pain. Moreover, the total opioid consumption was not higher in the pre-incisional low-concentration group than in the postoperative high-concentration group. In light of our findings, pre-incisional low-concentration ropivacaine infiltration has many advantages and can be useful in the perioperative period.