Spontaneous coronary artery dissection (SCAD) is an increasingly recognized, non-iatrogenic, non-traumatic, non-atherosclerotic disease presenting as an acute coronary syndrome [1, 2]. The dissection can recur and involve not only coronary but also visceral, cerebral and cervical arteries [3]. The predictors for recurrence remain unspecified. However, one study suggested fibromuscular dysplasia (FMD) and migraine as potential risk factors [4].
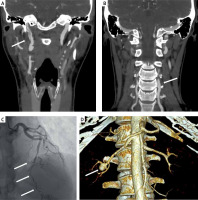
A 37-year-old woman with a history of migraine was admitted to hospital due to headaches in the occipital area associated with increased blood pressure, which started 10 days earlier and exacerbated 2 days before admission. During the hospitalization, she was diagnosed with arterial hypertension. Computed tomography (CT) angiography showed multivessel dissection: right internal carotid artery (RICA) dissection with the length of 45 mm (Figure 1 A), and 9 mm left vertebral artery (LVA) dissection (Figure 1 B). The patient was treated with antithrombotic (heparin) and antiplatelet (aspirin) drugs. After 20 days, control CT angiography demonstrated progression of the dissection with significant stenosis of the RICA true lumen. Therefore, flow-diverter stent implantation was performed. The patient was treated with dual antiplatelet therapy (DAPT).
Figure 1
A – Spontaneous dissection of the right internal carotid artery – computed tomography angiography. B – Spontaneous dissection of the left vertebral artery – computed tomography angiography. C – Spontaneous dissection of left anterior descending artery and second diagonal branch – invasive coronary angiography. D – Fibromuscular dysplasia in the right renal artery with coexisting renal artery aneurysm – computed tomography angiography
After 7 months the patient remained asymptomatic but follow-up cerebral arteriography showed persisting blood flow into the false RICA lumen. Consequently the second stent was implanted, and DAPT was continued. The next 6-month period of follow-up was uneventful; therefore, clopidogrel was discontinued and 150 mg of aspirin was recommended for 3 years.
In January 2018, she presented to hospital with ST-elevation acute coronary syndrome. Coronary angiography showed long spontaneous LAD dissection (mid-distal segment, type 2 b dissection) also involving the proximal segment of the second diagonal branch with complete (TIMI grade 3) flow in both arteries (Figure 1 C). SCAD was treated conservatively. Two weeks later, screening for vascular abnormalities revealed right renal FMD with renal artery aneurysm 14 × 10 × 11 mm. Computed tomography angiography performed 1 year later revealed complete LAD healing and no progression of renal artery aneurysm enlargement (Figure 1 D). Left ventricle ejection fraction in echocardiography was normal. Antinuclear antibodies were not present. The clinical course has remained uneventful to date.
Our case report presents a rare case of a patient with spontaneous multivessel cervical dissection involving RICA and LVA followed by SCAD after 18 months. Spontaneous artery dissection can occur suddenly and could be considered as one of the possible diagnoses in every young, middle-aged woman presenting symptoms suggesting myocardial infarction or stroke. The patient who has already experienced one artery dissection should be aware of the potentially increased risk of further episodes. Screening for extracoronary arteriopathies, including FMD and aneurysms, is recommended.








