The coexistence of non-small cell lung cancer (NSCLC) and thymoma is extremely rarely reported in the literature [1]. In recent years, in parallel with advances in minimally invasive surgical techniques, resection of both thymic and lung tumors can be performed with the video assisted thoracic surgery (VATS) method [2]. Here we present a case of a patient who underwent simultaneous surgical resection by VATS for both thymoma and squamous cell lung carcinoma.
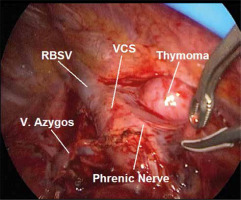
A fifty-seven-year-old female patient presented to us with cough complaint. Thorax tomography revealed a mass with 7 cm diameter at the right upper lobe and a thymic lesion at the anterior mediastinum (Figure 1 A). Histopathologic results of transthoracic Tru-cut biopsy were reported as squamous cell carcinoma and type AB thymoma. On positron emission tomography-computed tomography (PET-CT), pathologically increased uptake of 18F-FDG was detected at lung cancer and thymic tumor, with SUV-max 10 and 3 respectively (Figure 1 B). Invasive mediastinal staging was performed by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) and there was no nodal metastasis. The patient had no myasthenia gravis symptoms or signs. We planned simultaneous thymectomy and right upper lobectomy with mediastinal lymph node dissection in the same incision. A utility incision was made from the right anterior 4th intercostal space and a camera port incision was made at the right 8th intercostal space-posterior axillary line junction. Firstly, the chief surgeon performed the right upper lobectomy and mediastinal lymph node dissection procedure from the patient’s anterior, with pulmonary vein-pulmonary artery-bronchus sequencing. In this way, hilar, interlobar, paratracheal, subcarinal and pulmonary ligament lymph nodes were dissected. Then, for the thymectomy procedure, the chief surgeon was positioned behind the patient and the operating table was sided posteriorly. Thymic fat tissue over the pericardium was dissected with an energy device. Figure 2 shows intraoperative view of thymoma and surrounding structures. Thymic tissue was dissected with blunt and sharp dissections posteriorly to the vena cava and superiorly to the left brachiocephalic vein. The thymic vein that arose from the left brachiocephalic vein was clipped and divided. The thymectomy procedure was completed by advancing to the left hemithorax and sparing both phrenic nerves. Total time of surgery was 170 min and total blood loss was 135 ml. A 28 French sized chest tube was inserted from the camera port incision. The patient was discharged uneventfully on the postoperative 7th day. The final histopathological examination reported non-keratinized squamous cell carcinoma with 7.2 cm diameter and type AB thymoma with microscopic capsular invasion. There was no metastasis in lymph node dissection material. The patient received sequential chemoradiotherapy, 6 cycles of chemotherapy for lung cancer, and 45 Gy adjuvant radiotherapy for thymoma. There was no recurrence in follow-up of the patient. Informed consent was obtained from the patient for publication.
Figure 1
A – Chest computed tomography shows a large mass at the right upper lobe of the lung and a thymic mass at the anterior mediastinum. B – Pathologic increased uptake of 18f-FDG was detected at both lung cancer and thymoma on PET-CT (SUV max: 10 and 3 respectively)
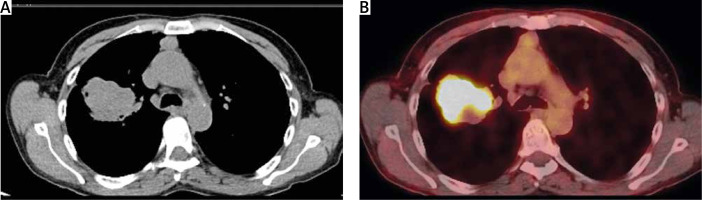
Figure 2
Intraoperative view of thymoma and surrounding structures
RBSV – right brachiocephalic vein, V. Azygos – azygos vein, VCS – vena cava superior.
Here we present simultaneous videothoracoscopic resection of both thymoma and NSCLC. Coexistence of these two malignancies has been reported exceedingly rarely in the English literature. In a case report presented by Dolci et al., the patient was 75 years old and had pulmonary symptoms [1]. In another article published by Moorjani the age of the patient was 57 and his complaint was exertional dyspnea [3]. Another patient reported in the literature was a 56-year-old woman presenting dyspnea and chest pain [4]. In a case series published by Deng et al. the median age was 63 and the majority of patients were female [2]. Our case was a 57-year-old female patient, consistent with the literature. Radiologically, it was noted that lung cancer accompanying the thymoma was right-sided in most of the previous case reports [1, 3–5]. Similarly, in our case lung cancer was detected in the right upper lobe. Generally, histopathologic examination of lung malignancies has been reported as adenocarcinoma in previous case reports. The histopathology of the thymic tumors were type AB thymoma in 2 cases and type B2 and B3 thymomas in the others [1, 3–5]. However, Xie et al. reported a case of thymic carcinoid tumor [6]. The type AB thymoma rate was 37.5%, and the lung adenocarcinoma rate was 75% in Deng’s case series [2]. Although the WHO classification of thymoma of our case was type AB, consistent with the literature, histopathological examination of lung cancer was squamous cell carcinoma, unlike previous case reports. Open surgical methods such as sternotomy and thoracotomy were preferred in previous publications for the surgical approach [2, 4]. Minimally invasive methods have been reported in related publications since 2014 [1, 2, 6]. We achieved simultaneously videothoracoscopic resection of both tumors by the same incision, similarly to current case reports. Since synchronous occurrence of thymoma and NSCLC is very rare, the issue of adjuvant therapy is not clear, especially in early stage tumors, and a separate evaluation should be made for each tumor stage [1]. In our case, the lung cancer stage was IIB according to the 8th TNM classification and cisplatin-etoposide-based adjuvant chemotherapy was administered. Additionally the thymoma stage was IIa according to the modified Masaoka classification and 45 Gy sequential radiotherapy was performed in the thymic region.
As a result, simultaneous thymectomy and lobectomy with mediastinal lymph node dissection can be performed successfully for patients with synchronous lung cancer and thymoma. In this way, adverse effects associated with repetitive anesthesia sessions and the delay in the treatment of malignancy will be prevented.






