Introduction
Minimally invasive surgery is now a standard option for the treatment of colorectal cancer and efforts to minimize parietal trauma, surgical stress, and scarring after surgery have drawn interest to single-port surgery among laparoscopic surgeons. However, single-port laparoscopic surgery for left-sided colorectal cancer has its unique challenges, including the relative loss of triangulation due to straight instruments being parallel to the laparoscope, the in-line vision, the clashing of instruments, and the steep learning curve to master the procedure. In particular, using the staplers to transect the rectum is the most difficult and time-consuming part of single-port laparoscopic surgery for rectal or rectosigmoid colon cancer. While it is difficult to make a right angle between the bowel and the cartridge of the stapler in pure single-port laparoscopic surgery, laparoscopic single-port + one-port surgery can facilitate appropriate endo-stapling with triangulation in a narrow pelvic cavity [1–3]. However, these approaches for left-sided colon cancer remain challenging, even for experienced laparoscopic colorectal surgeons.
The single-site instrumentation package for the Da Vinci robot Single-Site system (Intuitive Surgical, Sunnyvale, CA) was particularly designed to overcome the limitations of single-port laparoscopic surgery. The two curved tools intersect each other but are “repositioned’’ by software to fit the surgeon’s corresponding hands on the console; this surgical platform represents a means to safely perform these procedures in an intuitive fashion with the dominant hand for right-handed surgeons. The main difference between the conventional robotic approach and the Single-Site platform is the use of semiflexible instruments with, however, the loss of wristed instrumentation.
Recently, the da Vinci Single-Site platform plus one additional port robotic surgery, or between single plus one-port robotic surgery (SPORS) was introduced for the treatment of various diseases [4–8]. Besides minimizing collisions between surgical instruments and the camera, the SPORS approach allows easier creation of triangulation and more precise lymph node dissection around the central vascular trunk by the use of wristed instrumentation and enables safer rectal transection through an additional port, thus maintaining the cosmetic advantage of single-port surgery. In our previous study, we reported initial experiences with SPORS for the treatment of left-sided colon cancer [9].
In general, survival was considered the most important endpoint of studies addressing patients with colorectal cancer, until recently. Functional results, as well as quality of life and cosmesis, are now considered important surgical outcome measures. Body image – a person’s perception of, satisfaction with, and attitude towards his or her own body – has been broadly investigated in patients undergoing thyroidectomy, appendectomy, cholecystectomy, and bowel resection [10–14]. However, limited data are available on the cosmetic consequences of scarring in patients undergoing laparoscopic or robotic surgery with different port accesses for colorectal cancer.
Aim
The aim of the present study was to compare the clinical and cosmetic outcomes of SPORS with those of multi-port laparoscopic surgery (MPLS), which is presently the standard surgical treatment for colon cancer.
Material and methods
Patients
Between August 2014 and January 2016, 386 patients underwent colonic resection for left-sided colon cancer. The exclusion criteria of this retrospective study were open surgery (n = 121), multi-port robotic surgery (n = 25), distant metastasis (n = 22), synchronous or other previous malignancies (n = 11), emergency operation due to perforation or obstruction and combined resection of adjacent organs due to locally advanced lesions (n = 35), and patients who were unable to complete surveys (n = 61). After applying the exclusion criteria, 36 patients who underwent SPORS and 61 who underwent MPLS were included in this study. Left-sided colon cancer was defined as a tumor located in the area between the proximal splenic flexure and rectosigmoid junction detected by preoperative evaluation. In this study, three colorectal surgeons with experience in both techniques, MPLS and SPORS, performed the operation. In determining the surgical method, patients selected the surgical method after explanation of the advantages, disadvantages, and costs of both approaches because robotic surgery is not covered by public health insurance and is more expensive than laparoscopic surgery. In general, patients with private insurance tended to opt for robotic surgery.
Evaluation parameters
Information on patient demographics included age, sex, body mass index, American Society of Anesthesiologists physical status classification, tumor location, previous abdominal surgery, preoperative obstruction, and preoperative carcinoembryonic antigen (CEA) level from a prospectively collected colorectal cancer database. The collected perioperative details included total operative time, total length of incision, conversion, pain score in the numeric rating scale, time to sips of water and soft diet initiation, length of in-hospital stay, time to urinary catheter removal, postoperative morbidity, and histopathologic results. Conversion of SPORS was defined as an interruption of the robotic approach, followed by laparoscopic or open surgery at any time to complete the surgical procedure, except for anastomotic procedures. Conversion of MPLS was defined as an interruption of the laparoscopic approach, followed by open surgery at any time. Postoperative pain was measured using the numeric pain rating scale, with endpoints labeled as “no pain” (score of 0) and “worst possible pain” (score of 10) on postoperative days 1 and 2. Postoperative pain was managed using intravenous patient-controlled analgesia or continuous wound infiltration according to surgeon preference. Tumor stage was determined in accordance with the American Joint Committee on Cancer 8th edition staging system. The strategy of adjuvant chemotherapy followed the National Comprehensive Cancer Network guidelines. The study protocol was approved by the institutional review board of Dongsan Medical Center (IRB number 2020-06-050), and informed consent was obtained from all patients.
Surgical techniques
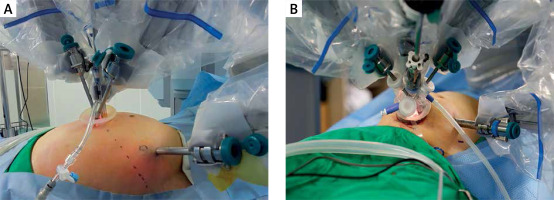
The standard operative procedure, including tumor-specific mesorectal excision and D3 lymphadenectomy, was the same in both groups. For SPORS, a single 25-mm vertical incision was made through the umbilical skin for single-port insertion and an additional 12-mm incision was made for the conventional robotic port in the right lower quadrant, in accordance with the previously reported SPORS techniques at our center [15]. Regarding single port, we used the Single-Site port (Intuitive Surgical, Sunnyvale, CA) or Glove port (Nelis, Bucheon, Korea) as access ports. For MPLS, we used five ports: two 12-mm ports – one (at the umbilicus) for a camera and the other (above the umbilicus, right side, midclavicular line) as a working port. The three remaining ports, 5-mm each, were placed in each remaining quadrant (Figure 1). An extraction site was created by extending the periumbilical or transumbilical incision for camera insertion.
Patient Scar Assessment Questionnaire scores at 12 weeks postoperatively
The patients completed the Patient Scar Assessment Questionnaire (PSAQ) at 12 weeks postoperatively in the outpatient clinic. The PSAQ has five subscales, four of which have been validated and are used in the scoring [14]. The validated subscales include the following: appearance, consciousness, satisfaction with appearance, and satisfaction with symptoms. Appearance was assessed using questions on scar color, width, flatness, texture, shine, and overall appearance. Consciousness was further delineated into itchiness, pain, discomfort, numbness, odd sensations, and overall troublesomeness of symptoms. Satisfaction with appearance was ascertained by how noticeable the scar was to the patient and to others and by the overall self-consciousness the patient associated with the scar. Satisfaction with symptoms was assessed according to the satisfaction with numbness of the scar, color, similarity to surrounding skin, and overall appearance. Each subscale comprises a set of items with four-point categorical responses, with scores ranging from 1 to 4 points (1 point is assigned to the most favorable response and 4 points are assigned to the least favorable response). Each subscale also contains a single global assessment item that is not included in the summary subscale score but is used to provide a clinically meaningful descriptor for the summary score and for internal validation analysis. For items with double response scales “No” is assigned 1 point. However, if the patient considers the scar as darker or lighter, the remaining categories of slightly darker OR slightly lighter, fairly darker OR fairly lighter, or much darker OR much lighter are assigned 2, 3, or 4 points, respectively.
Statistical analysis
Clinical characteristics and variables were compared between the SPORS and MPLS groups using the χ2 test for categorical data and the independent t-test for continuous data. P-values of < 0.05 were considered indicative of statistical significance. Statistical analyses were performed with IBM SPSS 21.0 software (SPSS Inc., Chicago, IL, USA), and data are expressed as medians with interquartile ranges.
Results
Patient characteristics
The demographic characteristics, including age, sex, body mass index, physical status according to the American Society of Anesthesiology status, preoperative CEA level, tumor location, preoperative obstruction, and number of previous abdominal operations, did not differ significantly between the SPORS and MPLS groups (Table I).
Table I
Patient and tumor characteristics
Perioperative clinical outcomes
All 97 operations were technically successful without the need for conversion to open surgery (Table II). One (3.1%) patient with rectosigmoid colon cancer required conversion from SPORS to reduced-port laparoscopic surgery due to air leak from the single port and external collisions of robotic arms. Regarding single ports, the Single-Site port used in the first 3 cases was not flexible and had poor durability. After our experience with the third patient who required conversion from SPORS to reduced-port laparoscopic surgery, we changed from a Single-Site port to a Glove port, which is more convenient for lifting remote centers of R1 and R2 cannulas and the camera port out of the abdominal wall to secure the distance between instrument tips and the surgical field, such as inferior mesenteric vessels (Photo 1). The operative time was significantly shorter in the MPLS group than in the SPORS group (median time: 155 vs. 232 min, p = 0.009). There were no apparent differences in the time to sips of water, tolerance to soft diet, length of hospital stay, or pain score measured on the numeric rating scale on postoperative days 1 and 2. Overall morbidity within 30 days after surgery and Clavien-Dindo classification were comparable between the two groups (p = 0.460 and p = 0.343, respectively). Two (5.6%) patients in the SPORS group and 4 (6.5%) patients in the MPLS group developed superficial surgical site infection at the specimen extraction site, with no significant difference between the groups. Two minor anastomotic leakages occurred in 2 (3.3%) cases in the MPLS group and were managed by non-surgical treatment using antibiotics and drainage. One instance of postoperative anastomotic site bleeding (2.8%) occurred in the SPORS group, but reoperation or another intervention was not required. There was no reoperation or mortality within 30 days of surgery.
Table II
Perioperative outcomes
Postoperative pathologic outcomes
There were no differences in stage distribution, histologic differentiation, proportion of patients with lymphovascular and perineural invasion, and tumor size (Table III). The mean numbers of harvested lymph nodes (SPORS: 15 vs. MPLS: 18, p = 0.743) and the resection margins were comparable between the two groups. The proportion of patients who received adjuvant chemotherapy was similar between the two groups (SPORS: 52.8% vs. MPLS: 49.2%, p = 0.732).
Table III
Postoperative pathologic outcomes
Cosmetic outcomes
The SPORS group had a shorter total incision length (SPORS: 50 mm vs. MPLS: 80 mm, p < 0.001). Regarding the scars, patients in the SPORS group provided higher subscale ratings for appearance (15 vs. 18, p < 0.001), consciousness (9 vs. 11, p < 0.001), satisfaction with appearance (14 vs. 17, p < 0.001), and satisfaction with symptoms (9 vs. 10, p = 0.022), and they had a higher overall PSAQ score (47 vs. 55, p < 0.001) than the patients in the MPLS group (Table IV).
Table IV
Patient Scar Assessment Questionnaire scores
Discussion
Our present findings demonstrate the technical feasibility and short-term oncologic safety of SPORS. SPORS showed comparable clinicopathologic and superior cosmetic outcomes to those of MPLS for left-sided colon cancer. The 30-day postoperative complication rates were 16.7% in the SPORS group and 23.0% in the MPLS group, without major complications or procedure conversion to open surgery, although the operative time was significantly longer in the SPORS group. Our evaluation of body image perception and cosmesis satisfaction showed statistically superior outcomes with the da Vinci Single-Site surgery than with multiport laparoscopic colectomy at the 12-week follow-up visits. To our knowledge, this is the first study to evaluate SPORS and the conventional multi-port laparoscopic approach and to elucidate the superiority of SPORS with respect to patient scar assessment.
In the present study, the operative time was significantly longer in the SPORS group than in the MPLS group (232 vs. 155 min, respectively). We believe that differences in operation time of more than 1 h in the Trendelenburg position may also be clinically significant, although the difference in operative time was not an unexpected finding. Our previous article on reduced-port versus multi-port robotic colectomy showed that the total operation time in the SPORS group was 258 min, although this time decreased as experience accumulated [16]. Regarding postoperative pain, reducing the number of ports in minimally invasive surgery could minimize the parietal trauma and invasiveness of the procedure.
A previous report indicated that the pain on postoperative day 1 and the duration and dose of analgesics were significantly lower in the reduced-port robotic group than in the conventional three-port robotic group for adrenalectomy [17]. The SIMPLE multicenter randomized clinical trial that compared single-port and multi-port laparoscopic surgery for colon cancer reported that the pain score using the visual analog scale decreased with time in both groups, and that the pain scores were not significantly different between the two groups at rest or while coughing [18]. In the present study, the pain score measured on postoperative days 1 and 2 using the numeric rating scale was not significantly different between the two groups. Further studies are needed to ascertain the impact of reducing the number of ports on postoperative pain after minimally invasive surgery.
Laparoscopic resection is regarded as the treatment of choice for malignant colonic diseases [19–21]. This procedure offers certain advantages, including low invasiveness compared to open surgery and acceptable safety and feasibility as an oncologic surgical approach. In this research, there were no apparent differences in postoperative outcomes, including tolerance of soft diet, length of hospital stay, and morbidity within 30 days after surgery. Moreover, the mean numbers of harvested lymph nodes and the resection margins were comparable between the two groups. These findings support the oncologic safety and technical feasibility of SPORS compared to standard MPLS for left-sided colectomy.
Improvements in the early detection of malignancy have resulted in longer survival times in cancer patients. However, post-surgery cancer patients have had to live with the consequences of this disease and of surgery, such as bowel function problems, postoperative scar, and related psychological distress [22, 23]. Cosmetic outcomes have been broadly investigated in patients after operations, such as thyroidectomy, hysterectomy, cholecystectomy, and laparoscopic bowel resection for non-malignant diseases [10–12, 24]. However, limited data are available regarding the subjective cosmetic consequences of scarring in patients with colorectal cancer. Minimally invasive surgery can provide social needs with respect to quality of life in cancer treatment and cosmetic benefits are expected from fewer ports. Recently, Hamabe et al. [25] evaluated patient satisfaction with cosmesis and body image after colorectal surgery using a validated body image questionnaire and Photo Series questionnaire and reported that the reduced-port laparoscopic group showed significantly better Photo Series questionnaire scores and had more positive overall body image questionnaire scores than the multi-port group. Our data reflect and support these findings, suggesting that reduced-port surgery can offer advantages over conventional multi-port surgery in terms of improved cosmesis.
A new robotic approach, the single-port da Vinci robot platform, has been specifically developed for single-site surgery. This robotic platform has a high-degree-of-freedom robotic arm that is directly inserted into the peritoneal cavity through a single incision. The advantages of the single-port da Vinci robot platform include instrument positioning display by a hologram, the use of wristed articulation and flexible elbows, a console-controlled camera, and three-dimensional optics. These advantages provide high dexterity, especially in the field of transanal, transoral, and transabdominal surgery. Noh et al. [26] reported the feasible and safe initial experience of single-port and reduced-port robotic surgery using the single-port da Vinci system for right- and left-sided colorectal resection. Future studies are needed to demonstrate the true benefits of various kinds of single-port and reduced-port accesses with laparoscopic and robotic surgery.
This study has limitations derived from its retrospective and non-randomized nature, small sample size, lack of data regarding quality of life, and selection bias regarding surgical methods that could affect surgical outcomes. Regarding cosmesis, it is not clear whether the cosmetic outcome, the primary end-point of this study, was due to reduced-port surgery or robotic surgery. Further, our conclusions regarding cosmetic outcomes were dependent on patient perception, which was affected by selection bias as the patients themselves chose the type of procedure. This limitation could be overcome by prospective randomized studies which measure the operator’s inter-observer evaluation using an alternative questionnaire, such as a patient and observer scar assessment questionnaire [27]. Additionally, the different surgical platforms of robotic and laparoscopic surgery with different port accesses can be confusing, although the present study was intended to compare a relatively innovative procedure with a conventional procedure.