Introduction
Inflammatory bowel disease (IBD) is an autoimmune chronic inflammatory gastrointestinal disease. Crohn’s disease (CD) and ulcerative colitis (UC) are the main types of IBD [1].
CD was first described by Prof. Burrill Bernard Crohn at Mount Sinai Hospital in New York in 1932. CD is a transmural inflammatory disease that affects any part of the gastrointestinal tract from mouth to anus in patchy affection or skip lesions in the form of superficial aphthous ulcers that may fuse together to form longitudinal or transverse ulcers in advanced stage with normal mucosa between the ulcers leading to a ‘cobble stone’ appearance of the mucosa, which is characteristic for CD. CD may have one of 3 pathways either inflammatory course in the form of remission and relapse or stricturing course, which leads to stricture and obstruction or fistulising course, which in turn leads to fistula formation [1].
UC is a mucosal disease that begins in the rectum and may spread proximally to involve the whole colon. The mucosa is oedematous, ulcerated, and haemorrhagic, and it may have pseudopolyps in active stages. UC is a precancerous disease and may cause adenocarcinoma of the colon and also may lead to toxic megacolon in some severe cases [1].
The “gut microbiota” is the collection of bacteria, archaea, and Eukarya that live in the human GI tract, and some of it can exchange benefits with the human body while some others can be harmful to the body, and they are in equilibrium between beneficial and harmful states. The gut microbiota is formed at 1–2 years after birth when the intestinal epithelium and mucosal barrier are formed. These microbiota bacterial cells number more than 1014, which means 10-fold the human cells and 1000-fold genomic materials than the human genome. The contents and quantities of the microbiota change according to chemical, nutritional, and immunological factors through the gut regions [2].
The gut microbiota offers many benefits to the human body, such as keeping the integrity of the intestine, protecting against pathogens, and development, maturation, and regulation of immune system, and fermenting dietary fibre to short chain fatty acids (SCFAs) like butyric acid and acetic acid. Diet is a major source that formulates the contents of the microbiota. If any alteration occurs to the composition of microbiota, it is called dysbiosis, which leads to disturbance of the equilibrium between beneficial and harmful bacteria by decreasing beneficial bacteria and increasing harmful bacteria, and it may share in the pathogenesis of a lot of diseases like IBD, irritable bowel syndrome (IBS), colon cancer, and antibiotic-associated diarrhoea [3].
The gut microbiota is composed of 12 phyla of bacteria and 1014 bacterial cells of more than 2000 species. The major phyla found in the gut are 6 phyla, which are (1) Firmicutes that contains Faecalibacterium, (2) Bacteroidetes that contains Bacteriodes, (3) Verrucomicrobia that contains Akkermansia, (4) Actinobacteria that contains Bifidobacterium, (5) Proteobacteria that contains Escherichia, and (6) Euryarchaeota. The other 6 phyla are minor phyla in addition to Archaea and Eukarya [4].
Faecalibacterium prausnitzii is named after Otto Prausnitzii, the German bacteriologist who discovered it. It is a gram-positive bacteria, rod shaped, anaerobic, non-spore forming, non-motile, one of the most abundant in human gut microbiota, it is found in about 5% of the gut microbiota, it produces butyrate and short chain fatty acids, and it boosts the immune system and improve gut barrier function. It is classified as species F. prausnitzii and genus Fecalibacteria and family Ruminococcaceae order Clostridiales and class Clostridia and phylum Firmicutes [5, 6].
It uses simple carbohydrates as a carbon source for growth, it can live in the low oxygen of the gut, and it grows in the optimal pH of the colon (5.7–6.7). In IBD there is acidic stool, so there is a low abundance of this bacteria. It produces butyrate, which is an important energy source for colonocyte and acts as an anti-inflammatory for IBD through inhibition of NF-κB transcription factor activation [7, 8].
Several studies found that these bacteria to be depleted in CD and UC patients. Other studies found these bacteria to be potential biomarkers to discriminate CD from IBS and CD from healthy people [9].
Aim
The aim of this study is to determine the role of F. prausnitzii in Egyptian patients with UC and CD and to correlate it with the disease activity.
Material and methods
Patients
This study included 80 patients divided as follows: 3 groups of patients recruited by random sampling, group (I): 30 patients with UC, group (II): 30 patients with CD, and group (III): 20 healthy patients as control.
Inclusion criteria
Patients newly diagnosed as IBD (CD and UC) from both genders, adults, able to give consent, will be included in the study.
Exclusion criteria
Patients were excluded if they had gastrointestinal malignancy, recent gastrointestinal surgical intervention of the small or large intestines within the last 6 months, history of prolonged use of antibiotics, non-steroidal anti-inflammatory drugs abuse, pregnancy, severe burn, sepsis, chronic advanced renal disease, or liver disease.
Ethical approval
The study follows the principles of the Declaration of Helsinki. After approval of the Ethical Committee (approval number: 0105301), Faculty of Medicine, Alexandria University, signed informed consent was obtained from each patient expressing their acceptance to participate in the study and have the results published.
History and examination
All patients were subjected to the following:
Detailed history taking with emphasis on GIT symptoms and their duration, such as abdominal pain, diarrhoea, weight loss, and gastrointestinal bleeding – either occult or fresh.
Systemic physical examination including general and abdominal examinations for detection of tenderness, palpable organs, or masses.
Laboratory investigations including the following:
Ileo-colonoscopy was done for all patients. Patients were prepared with a low-fibre diet on the day preceding the colonoscopy, a split regimen of 4L of polyethylene glycol (PEG) solution (or a same-day regimen in the case of afternoon colonoscopy), no longer than 4 h before the colonoscopy. Four biopsy specimens from 5 sites, including the ileum and rectum, were obtained from both affected and normal-appearing mucosa; specimens from different locations were labelled and submitted separately. To assess the activity of the diseases, the total Mayo score was used for UC [10]; Crohn’s disease activity index (CDAI) [11] and SES score [12] were used for CD. A histopathological examination for the biopsy specimen was done.
Statistical analysis
Data entry and analysis were carried out using the Statistical Package for Social Sciences version 20 (SPPS PASW Statistics, Chicago). Data were coded, entered, and code checked before analysis. Quantitative variables were presented in the form of range, mean, median, and standard deviation. On the other hand, studied qualitative variables were presented as frequency and percentage from total. Comparisons between the different study groups were carried out using χ2 for qualitative variables and t-tests for quantitative ones. All results were interpreted at a 5% level of significance where the difference between the study groups was considered significant if p ≤ 0.05.
Results
Demographic data
The present study was carried out on 30 UC patients; 22 male and 8 female, with a male-to-female ratio of 5.5 : 2; age ranged from 20 to 70 years with a mean age of 32.20 ±10.73 years. The CD group comprised 30 patients, 19 male and 11 female, with a male-to-female ratio of 1.7 : 1; age ranged from 20 to 44 years with a mean age of 28.80 ±7.30 years. The control group comprised 20 cases; 9 male and 11 females; age range from 23 to 42 years with a mean age of 33.0 ±5.83 years (Table I).
Table I
Comparison between the 3 studied groups according to demographic and clinical data
Clinical and laboratory data
Two of the patients had a positive family history of UC, and 4 of the patients had a positive family history of CD. The disease duration of UC ranged from 1 to 14 years with mean of 2.70 ±2.96 years, and for CD it ranged from 1 to 18 years with mean of 2.0 ±3.17 years (Table I).
In addition, faecal calprotectin ranged from 80.0 to 2937.0 with a mean of 425.97 ±586.71, and CRP ranged from 7 to 102 with a mean of 40.43 ±34.94.
Endoscopic findings and score indices
The total Mayo score for UC ranged from 4 to 12 with a mean of 8.77 ±2.62; there were 4 (13.3%) mild, 4 (13.3%) moderate, and 22 (73.3%) severe cases (Table II).
Table II
Distribution of the studied cases according to total Mayo score in the UC group (n = 30)
In CD, CDAI ranged from 3 to 11 with a mean of 6.43 ±2.01; there were 22 (73.3%) remission, 5 (16.7%) mild, 3 (10%) moderate, and 0 (0%) severe cases. SES score ranged from 3 to 11 with a mean of 6.43 ±2.01; there were 17 (56.7%) mild, 13 (43.3%) moderate, and 0 (0%) severe cases (Table III).
Table III
Distribution of the studied cases according to CDAI in the CD group (n = 30)
Microbiome results
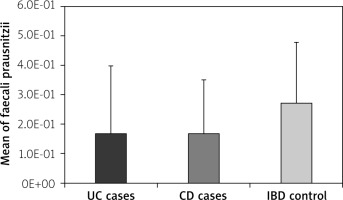
Regarding F. prausnitzii in the study groups, in group 1 of UC patients, we found the level of bacteria ranged from 2.35E-04 to 8.79E-01 with a mean of 1.68E-01 ±2.30E-01. In group 2 of CD patients we found the level of bacteria ranged from 1.06E-05 to 7.0E-01 with a mean of 1.70E-01 ±1.80E-01. In group 3 of the control group, we found the level of bacteria ranged from 5.90E-02 to 8.66E-01 with a mean of 2.72E-01 ±2.05E-01 (p = 0.015 significant) (Table IV, Figure 1).
Table IV
Faecalibacterium prausnitzii in the study groups
[i] IQR – interquartile range, SD – standard deviation, H – H for Kruskal-Wallis test, p – p-value for comparing between the studied groups; p1 – p-value for comparing between UC Cases and CD Cases, p2 – p-value for comparing between UC Cases and IBD control, p3 – p-value for comparing between CD Cases and IBD control; *statistically significant at p ≤ 0.05.
Regarding significance between the study groups, we found p1 = 0.397, which shows no significant difference between the CD group and the UC group. P2 = 0.004 shows a significant difference between the UC group and the control group. P3 = 0.037 shows a significant difference between the CD group and the control group.
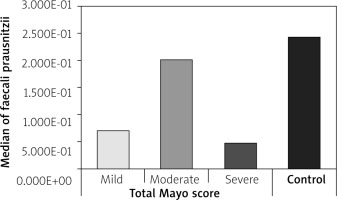
Regarding F. prausnitzii in UC patients according to the Mayo score, in mild patients, the level of bacteria ranged from 3.36E-02 to 1.25E-01 with a median of 6.98E-02 (p = 0.077, NS). In moderate patients, the level of bacteria ranged from 5.60E-04 to 8.79E-01 with a median of 2.01E-01 (p = 0.652, NS). In severe patients, the level of bacteria ranged from 2.35E-04 to 6.59E-01 with a median of 4.80E-02 (p = 0.006, significant). In the control group, the level of bacteria ranged from 5.90E-02 to 8.66E-01 with a median of 2.43E-01 (p = 0.033, significant) (Table V, Figure 2).
Table V
Bacterial abundance in the UC group according to total Mayo score
[i] IQR – interquartile range, SD – standard deviation, H – H for Kruskal-Wallis test, pairwise comparisons between 2 groups were done using Post Hoc Test (Dunn’s for multiple comparisons test), p – p-value for comparing between the studied groups, p0 – p-value for comparing between Control and each group; *statistically significant at p ≤ 0.05.
Figure 2
Comparison between total Mayo score in UC cases and the control group according to Faecalibacterium prausnitzii
Regarding F. prausnitzii in CD patients according to CDAI score, in remission patients, we found the level of bacteria ranged from 7.70E-04 to 7.0E-01 with z mean of 1.71E-01 ±1.94E-01. In mild patients, we found the level of bacteria ranged from 1.06E-05 to 2.71E-01 with a mean of 1.34E-01 ±1.32E-01. In moderate patients, we found the level of bacteria ranged from 2.56E-02 to 3.67E-01 with a mean of 2.21E-01 ±1.76E-01. In the control group, the level of bacteria ranged from 5.90E-02 to 8.66E-01 with a mean of 2.72E-01 ±2.05E-01 (p = 0.110 NS) (Table VI).
Table VI
Bacterial abundance in the CD group according to CDAI score
Regarding F. prausnitzii in CD patients according to SES score in Table III, in mild patients, the level of bacteria ranged from 7.70E-04 to 7.0E-01 with a mean of 1.91E-01 ±2.11E-01. In moderate patients, the level of bacteria ranged from 1.06E-05 to 3.67E-01 with a mean of 1.42E-01 ±1.29E-01. In the control group, the level of bacteria ranged from 5.09E-02 to 8.66E-01 with a mean of 2.72E-01 ±2.05E-01 (p = 0.084 NS) (Table VII).
Table VII
Bacterial abundance in the CD group according to SES score
Discussion
The human gastrointestinal tract harbours a complex and dynamic population of microorganisms, the gut microbiota, which exert a marked influence on the host during homeostasis and disease. Multiple factors affect the development of the human gut microbiota during infancy. Diet is considered as one of the main drivers in shaping the gut microbiota throughout. Gut microbiota plays a critical role in maintaining immune and metabolic homeostasis and protecting against pathogens. Dysbiosis, which is the alteration in gut bacterial composition, has been associated with the pathogenesis of many inflammatory diseases and infections [2].
Large-scale studies of human gut microbiomes have revealed broad differences in composition across geographically distinct populations [13–16]. Because F. prausnitzii is the most abundant bacteria of the gut microbiome, the current study was done to assess its alteration in Egyptian UC and CD patients and its relationship with control and disease activity.
As regards UC group, we found the level of F. prausnitzii significantly decreased in UC patients (mean 1.68E-01) compared to the control group (mean 2.72E-01). And there is a significant reduction in the level of F. prausnitzii in the severe stage of the disease (median 4.80E-02), so the level of bacteria can be affected by the severity of the disease.
Machiels et al. found in a study conducted upon 127 UC patients that F. prausnitzii decreased in patients with UC in relation to controls (p < 0.0001), and there was an inverse correlation with disease activity, which agreed with our results [17]. Ahmed et al. performed a study on 21 active UC patients, F. prausnitzii was higher in mild than in moderate and severe cases; however, the difference was not statistically significant [18]. On the other hand, Liu et al. conducted a study on 48 patients with UC and 48 healthy control and found that F. prausnitzii increased in UC patients more than in healthy controls [19].
As regards the CD group, we found that the level of F. prausnitzii was significantly decreased in CD patients (mean 1.70E-01) compared to the control group (mean 2.72E-01), but there was no significant difference between CD patients and UC patients, so it cannot be used as a marker for differentiation between the 2 diseases. Also, we found no significant difference of the level of bacteria according to the severity of the disease either clinically or endoscopically, the severity of the disease did not affect the level of the bacteria.
In agreement with our results, Rapat pittayanon et al. found in a systemic review done in Canada the differences in gut microbiota in patients with and without IBD, where they reported that 6 out of 11 studies in CD patients showed a decreased level of F. prausnitzii in relation to the control group, which agreed with our results [20]. Takahashi et al. concluded in their study that F. prausnitzii was significantly decreased in patients with CD in relation to the control group [21]. Joossens et al. in their study conducted in the Department of Gastroenterology in University Hospital Gasthuisberg, Leuven, Belgium upon 68 patients with CD, found that F. prausnitzii decreased significantly in CD patients compared to healthy controls [22].
Manichanh et al., in a study in France conducted upon 6 patients with CD and 6 healthy controls using a metagenomic approach, found significant decrease of Firmicutes including F. prausnitzii in CD patients [23]. Against our results, Pascal et al. found, in a study conducted upon 34 CD patients and 33 UC patients and 111 healthy controls in Spain, that there was a significant decrease in Faecalibacteria in CD patients and healthy controls and UC [24].
Conclusions
There was a significant difference between CD and UC patients and the control group in F. prausnitzii. There was a significant reduction in F. prausnitzii only in severe UC cases. But there was no significant difference between CD and UC patients in F. prausnitzii.
Recommendations
Further studies are needed on many patients to confirm the decrease of Faecalibacteria in UC patients because not all the studies agreed about this.
Since most of studies agreed about the decrease of Faecalibacteria in CD, and hence it can be a microbiomarker for CD, we recommend a probiotic that includes this Faecalibacteria to treat and maintain remission in CD patients.