Introduction
A paraovarian cyst (POC) is defined as a cystic mass located in the broad ligament or the mesosalpinx [1, 2]. They are labelled as paraovarian or paratubal depending on the proximity to the respective structure, though the two terms are generally interchangeable [1]. Their prevalence has been estimated to be as high as 5–20% amongst the adnexal masses [1, 3]. Despite the high prevalence and the availability of advanced imaging modalities in modern-day medicine, it is estimated that an accurate diagnosis of POC prior to surgery is still made in less than 50% of patients [1]. Here, we describe a case series of six patients with POCs, their varied clinical presentations and management done at a tertiary care centre.
Material and methods
Consent
Written informed consent was obtained from all patients for their anonymized data including the images to be published. The procedures followed were in accordance with the Helsinki Declaration of 1975, revised in 2000.
Case reports
Case 1
An 18-year-old nulliparous female presented to the gynaecology emergency department with the complaint of right iliac fossa pain associated with vomiting for two days. She had been referred from a local hospital as a suspected case of appendicitis. At presentation, her pulse rate (PR) was 112 beats per minute (bpm) and blood pressure (BP) was 98/64 mm Hg. On per-abdomen examination, there was an abdominopelvic mass corresponding to 14 weeks’ gravid uterus size, which was tender, had a cystic consistency, smooth surface, well-defined margins, and restricted mobility. Her urine pregnancy test was negative. Ultrasonography (USG) performed in the emergency setting showed a pelvic unilocular cystic lesion of size 14 × 10 cm with a colour score of one on the right side, a bulky right ovary of size 7 × 4 × 5 cm showing decreased colour uptake along with a normal left ovary (Fig. 1 A). Her blood investigations revealed an increased total leucocyte count of 14,400. A provisional diagnosis of right POC with right ovarian torsion was made and an emergency laparotomy was performed. Intraoperatively, there was a right POC of size 12 × 10 cm, with right ovarian torsion (Fig. 2 A). Paraovarian cystectomy was performed along with detorsion of the right adnexa. The patient recovered well post-operatively and was discharged in a stable condition after three days.
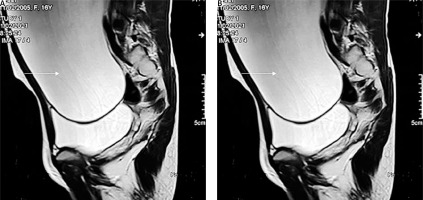
Fig. 1
Two-dimensional grey scale ultrasound images. A) Unilocular cyst (white arrow) seen separately from the two ovaries (dashed arrow); B) large unilocular cyst (white arrow) in a post-hysterectomy case; C) large unilocular anechoic cyst (white arrow); ovary is separately visualised (dashed arrow)
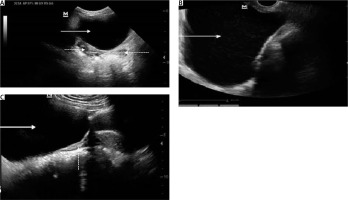
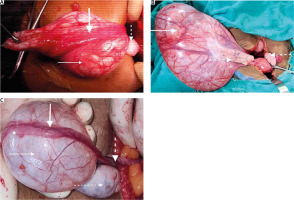
Fig. 2
Intraoperative images. A) Paraovarian cyst (thin solid white arrow) with fallopian tube (thick solid white arrow), ovary is separate (dashed white arrow); B) large right paraovarian cyst (arrow); ovaries are separate (dashed arrows); C) torsion (thick dashed white arrow) of paraovarian cyst (thin solid white arrow) and fallopian tube (thick solid white arrow); ovary is separate (thin dashed white arrow)
Case 2
A 42-year-old nulliparous female presented with generalized abdominal pain and a bloating sensation for the last six months. She had a history of total abdominal hysterectomy with bilateral salpingo-oophorectomy performed one year back in view of a large fibroid uterus with bilateral ovarian serous cystadenomas. On examination, her vitals were stable. Per-abdomen examination revealed a well-defined mass of cystic consistency corresponding to 14 weeks’ size gravid uterus. Bimanual examination showed the same cystic mass of size 10 × 10 cm in the left adnexa which was non-tender and had side-to-side mobility. USG revealed a 13 × 9 cm unilocular anechoic cyst with thin, incomplete septations (Fig. 1 B). As the patient had had previous bilateral oophorectomy, a provisional diagnosis of POC was made and the patient was taken up for surgery. Intraoperative finding revealed a large 14 × 10 cm mesenteric cyst along with multiple bowel adhesions. Surgical assistance was called for. Further adhesiolysis showed that the cyst was arising from between the two leaves of the mesentery, which was excised and sent for histopathology. A final diagnosis of mesenteric cyst was made. The patient recovered well post-operatively and was discharged in a stable condition after three days.
Case 3
A 16-year-old nulliparous unmarried female presented to the gynaecology outdoor service with gradually progressive abdominal distension for a period of one year. Her menstrual cycles were regular. She was haemodynamically stable. Abdominal examination showed a grossly distended abdomen. Transabdominal USG showed a large unilocular cyst arising from the ovary of size 23 × 24 cm with no internal colour flow. Tumour markers were done and were all normal. Magnetic resonance imaging of the pelvis and abdomen showed a well-defined thin-walled cystic lesion of size 16 × 26 × 33 cm with no solid components, noted in the abdominopelvic region, with normal bilateral ovaries, findings suggestive of a giant mesenteric cyst (Fig. 3 A). The patient was then transferred to the general surgery ward for further management. She underwent exploratory laparotomy and intraoperatively a huge cyst of around 20 × 30 cm in size was identified at the right mesosalpinx weighing 8.15 kg. The mass was confirmed as a POC because both ovaries were intact and discrete from the mass. The cyst was excised while preserving the adnexa.
Case 4
A 32-year-old multiparous female presented to the surgery outdoor service with the complaint of gradual abdominal swelling for the past eight months. Her vitals were stable. Abdominal examination showed a large 25 × 25 cm cystic, non-tender mass with well-defined margins and a smooth surface. USG abdomen revealed a huge 20 × 19 cm unilocular cyst with low-level internal echoes with no solid components extending from the epigastrium to the pelvis. A provisional diagnosis of a mesenteric cyst was made. The patient was admitted for further evaluation and management. Contrast-enhanced computed tomography (CECT) was performed and showed an abdominopelvic mass, 25 × 24 × 12 cm in size, likely arising from the right ovary (Fig. 3 B), with a normal uterus and left ovary with suspicion for neoplastic aetiology. The patient was henceforth transferred to the gynaecology department for further management. Her tumour markers were within the normal range. Laparotomy was performed and showed a huge, 25 × 25 × 15 cm, right POC with a normal uterus, and normal bilateral fallopian tubes and ovaries (Fig. 2 B). The cyst was excised while preserving the bilateral adnexa and sent for histopathology. The patient was discharged in a stable condition after 3 days.
Case 5
A 26-year-old nulliparous female presented to the gynaecology outdoor service with the inability to conceive since three years. Her examination findings were normal, except for right forniceal fullness on per-vaginal examination. USG performed for evaluation of infertility revealed a unilocular anechoic right ovarian cyst of size 7 × 6 cm. Other investigations done for the evaluation of infertility were normal. She was planned for laparoscopic cystectomy with chromopertubation. Intraoperatively, a right POC of size 8 × 8 cm was seen with normal uterus and bilateral fallopian tubes and ovaries. Cystectomy was done. Chromopertubation showed bilateral free peritoneal spill. The patient was discharged after two days in stable condition. She conceived spontaneously five months after the surgery and has been in routine follow-up at the obstetric unit since then.
Case 6
A 34-year-old multiparous female presented to the gynaecology emergency with the complaint of left lower abdominal pain for two weeks with increased intensity and vomiting for three days. On examination, she had a PR of 118 bpm and BP of 90/66 mm Hg. There was left iliac fossa tenderness. Per vaginal examination showed a palpable 8 × 6 cm tender mass in the left fornix with cystic consistency, smooth surface, well-defined margins and restricted mobility. Ultrasonography showed a unilocular anechoic cystic lesion of size 7 × 5 cm adjacent to the left ovary (Fig. 1 C) with minimal peripheral vascularity with normal uterus and bilateral ovaries. A provisional diagnosis of left POC torsion was made and the patient was taken up for laparotomy in the emergency setting. Intra-operative findings revealed an 8 x 6 cm left POC with two rounds of torsion with the left fallopian tube stretched over the cyst (Fig. 2 C) with normal bilateral ovaries and right fallopian tube. Cystectomy was done with fallopian tube detorsion and the cyst wall was sent for histopathology. The patient was subsequently discharged after three days in a stable condition.
Discussion
Paraovarian cysts are said to originate from the mesothelium of the broad ligament in 68% of cases, remnants of the paramesonephric duct in 30% of cases, and from the mesonephric duct remnants in the remaining 2% of cases [1, 3].
Paraovarian cysts have been reported in females of all age groups from neonates to post-menopausal [3], though the reported incidence is higher in reproductive-age females [3, 4]. In our case series also, five patients were in the reproductive age group. It is hypothesized that the alteration of the hormonal milieu in the reproductive age may be a contributing factor in the development of POCs. This is also supported by the fact that POCs have been found to increase in size during pregnancy [5]. Since POCs are affected by hormonal changes, whether oral contraceptive pills could be used for their management is worth exploring.
Traditionally, adnexal cysts are called ‘large’ when their size is more than five centimetres and ‘giant’ when they are larger than 15 centimetres [6]. Giant POCs are an uncommon entity [6]. It is notable that two of our patients had giant POCs measuring greater than 20 centimetres.
More than half of POCs are misdiagnosed as ovarian cysts, tubal cysts, peritoneal inclusion cysts and even mesenteric cysts [1]. In our case series, two cases were mistakenly diagnosed as mesenteric cysts, one as a benign ovarian cyst and one as an ovarian neoplasm. One patient who was preoperatively diagnosed to be having a POC was ultimately found to have a mesenteric cyst. The correct diagnosis prior to surgery can be made by ultrasound features such as the split sign (separation of the cyst from the ovary on applying probe pressure) [1] and the absence of the rim sign (normal ovarian follicles surrounding the cyst). It is vital to differentiate POCs from ovarian cysts as these behave differently both clinically and biologically [3]. Magnetic resonance imaging and CECT can also be used as modalities to better delineate the origin and nature of an adnexal mass [6]. Table 1 categorizes the differentiating features of POCs from other adnexal masses on USG.
Table 1
Ultrasound characteristics of different adnexal masses
Paraovarian cysts usually remain asymptomatic and are mostly visualized incidentally either on imaging or during surgery. At times, they can become symptomatic and present with acute abdominal pain in the event of cyst torsion, cyst rupture or haemorrhage [1]. Since POCs have no pedicle of their own, their torsion usually involves the ovary, fallopian tube or the infundibulopelvic ligament [3]. Two of our patients had cyst torsion, of which one had associated fallopian tube torsion. It is notable that POCs are the most common associated finding in the cases of isolated fallopian tube torsion [7], which in itself is a rare entity with the reported incidence of one in 1,500,000 [8]. Torsion has been more commonly reported on the right side, likely due to the sigmoid colon limiting the cyst mobility on the left [7]. These cases are usually misdiagnosed as appendicitis and diagnosed during surgery for the same [7]. One of our patients was also referred to us initially as a case of suspected appendicitis. Table 2 describes the detailed characteristics of the patients in our case series.
Table 2
Patient characteristics
Paraovarian cysts are also associated with an increased incidence of ectopic pregnancy and infertility as they can cause tubal narrowing and disturbed tubal motility [3]. One patient in our case series, with associated infertility, conceived spontaneously after cystectomy was done, further emphasizing the fact that the POC was the probable reason for infertility in her case.
Paraovarian cysts are mostly benign, though rare reports of borderline and malignant cases do exist [1, 6]. The reported incidence of borderline and malignant POCs is 2–3% [6]. Clinical features of rapid cyst growth associated with weight loss and anorexia, along with sonographic findings such as papillary projections, ascites, lymphadenopathy, and increased blood flow, can be used as indicators of malignancy [9].
No clear-cut guidelines exist for the management of POCs despite their high prevalence [6]. To date, the management has been decided by the individual gynaecologist based on the cyst size, presence of symptoms, and complications [6]. In general, conservative management has been advocated for cysts smaller than five centimetres [10], as larger cysts are more prone to complications [1, 6].
Surgical excision is the mainstay of treatment in cysts which are of large size, suspicious for malignancy and in cases of rupture or torsion. Laparoscopy is the preferred approach [11], with laparotomy being reserved only for patients with suspected malignancy [3]. Casarin et al. concluded in their study that irrespective of the size, laparoscopy should always be considered as the preferred surgical approach for the management of benign adnexal masses [12]. For the extraction of larger cysts in laparoscopy, techniques such as transvaginal extraction by culdotomy are being increasingly used as an effective and cheaper alternative [13, 14]. Benign cases should be treated by cystectomy by enucleating the cyst from the surrounding mesosalpinx [6]. An effort should be made to conserve the ovary and fallopian tube of these females at all costs, though at times excision of large POCs may necessitate removal of the tube or even the ovary [2]. There is no consensus on the management of borderline or malignant POCs [3]. To date, the management has been done on similar lines as borderline or malignant ovarian cysts by doing either unilateral adnexectomy or complete surgical staging depending on the female’s desire for future fertility [15].
Conclusions
Optimal management of an adnexal mass depends on the knowledge of the origin and the exact nature of the mass. Paraovarian cysts should be kept in mind as a differential diagnosis for patients with adnexal masses both by gynaecologists and radiologists. In view of the high prevalence of POCs, there is an increasing need for further research on this topic so as to formulate clear-cut guidelines for their management. Whether hormonal treatment might be successful in these cases needs further research. Gynaecologists need to be aware of the cases which can be managed conservatively and those that need surgery, along with the extent of the surgery required, taking care to protect the ovary at all costs, particularly in benign cases.