Introduction
Psoriasis, a well-documented disorder since 2000 B.C., is still a topic of exciting and challenging study. With further and further discoveries on the immunological basis of many disorders, it comes naturally to try to improve our knowledge on such a disease. Smoking seems to be one of the main triggering factors for the disease and plays a fundamental role in its natural history. This article aims to assess the most interesting discoveries on its role and the means of it.
Epidemiology
Epidemiologically the disease is highly diverse among both population age and country. The highest prevalence has been reported in the USA of 5.1%. The prevalence in the EU ranges from 0.73% to 2.9% in Italy. Estimates in Africa are of 0.09%. Prevalence in the North America ranges from 1.43% and 5.1%. Some ethnic groups seem to have no incidence such as Aboriginal Australians and South American Indians.
We can also observe in the study of Michalek et al. that in children less than 18 years old the prevalence ranges from 0 to 1,37% with a peak of prevalence in Germany population of 16,500 during a lifetime study, instead the lowest prevalence has been found in Taiwan.
In adults, the prevalence is much higher, ranging from 0.51% to 11.3%. The lowest prevalence was observed in the USA in a study of 799,607 patients with disabilities and/or above 65 years of age. The highest prevalence was noted in Norway in a study of 10,302 patients, notably the second European country for prevalence in adults is the United Kingdom with a prevalence of 1.3% [1].
Smoking and psoriasis
Psoriasis is a multifactorial disorder, both intrinsic and extrinsic factors play a major role in its etiopathogenesis. The factors are diverse and make the disease a challenging one to prevent. Other extrinsic factors that are worthy of note are alcohol consumption, psychological factors such as depression and of course smoking, which this article will focus on [2].
Smoking is for sure one of the most important risk factors for psoriasis, being its influence and the means of it yet to be fully understood, it is a challenging and exciting work trying to gather all the factors related to it that could influence the disease and its course. This addiction acts on psoriasis through the release of free radicals during combustion, this will trigger the activation of many cytokines and factors promoting oxidative stress in cells; furthermore, smoking activates independently, by cytokines, the factors involved in pathways normally active in psoriasis such as: MAPK, NF-κB, and Jak-Stat. Smoke also triggers the expression of genes involved in the development of psoriasis: HLA-CW6, and HLA-DQA1*0201 e CYP1A1 [3]. Notably enough, there also seems to be a synergistic interaction between the HLA-Cw6 and smoking habits of the patient [4].
Another mechanism involves the Aryl hydrocarbon receptor (AhR) on lymphocytes Th17 and Th22, leading to the release of interleukins IL-17 and IL-22 (Table 1) [5–8].
Table 1
Smoking, metabolic syndrome and psoriatic march
Both metabolic syndrome and smoking are associated to an increase in the risk of psoriasis, by these means, it is interesting to assess the relationship between the two factors and see how they act in a synergistic way in worsening the disease and its course.
In a big study performed in Utah by Herron et al., the role of smoking and obesity in psoriasis was assessed. It was shown that there is a higher prevalence of smokers in the obese population at enrolment, the concomitance of smoking and obesity also was found in patients with no family history of psoriasis. This suggests that the concomitance of smoking and obesity is a huge environmental factor in the development of disease. Also, it was assessed that smoking is more prevalent in obese patients with psoriasis compared to the rest of Utah population (35% vs. 9%). The study also concludes that, while smoking is a factor appearing before psoriasis, obesity seems to be concomitant with the onset of psoriasis itself [9].
A study by Wei et al. assessed the correlation between psoriasis and metabolic syndrome; in a population of 1014 patients, the prevalence of smoking was 31.85%, the prevalence of smokers was significantly higher in male than female patients, with increasing age and BMI the prevalence of tobacco smoking was also dramatically increased. The prevalence of metabolic syndrome seems to be higher in patients without tobacco smoking (OR = 2.26) [10].
A study by Owczarczyk-Saczonek et al. has shown an increase in the ApoB/ApoA1 ratio and triglyceride levels in a group of smoking women with psoriasis in Poland; this was related to an increase in incidence of metabolic syndrome [11].
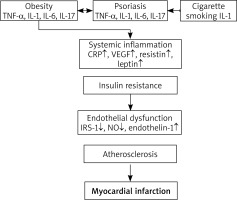
Due to the increase in prevalence of metabolic syndrome in patients with psoriasis, we also have an increase in the risk of atherosclerosis, this process will eventually lead to ischemic events and the increased risk of myocardial infarction and stroke. This phenomenon is called psoriatic march and it is a fascinating phenomenon to assess how psoriasis is not only a disorder of the skin, but also a systemic one in which multidisciplinary care must be given.
According to Boehncke et al., systemic inflammation caused by psoriasis is shown to induce insulin resistance, which causes the endothelial dysfunction that leads to atherosclerosis. The most intriguing hypothesis is that psoriasis might be an independent risk factor for cardiovascular disorder: even though the comorbidity alone does not give certainty of the direct correlation between psoriasis and cardiovascular disorders, we still have a strong suggestion of it (Figure 1) [12].
According to Yu et al., another important factor in cardiovascular disorders associated to psoriasis is adipokines, which play an important role in the cardiovascular diseases, also express abnormally in psoriasis and may induce or exacerbate the skin lesion. The adipokines associated with psoriasis and cardiovascular disease include adiponectin, leptin, resistin, omentin, visfatin, chemerin and retinoid binding protein 4 (RBP-4) [13].
It is mentioned by Masson et al. how the stroke risk in patients with psoriasis is increased in a way that is not explained by other major risk factors, hence it is safe to assume that there is a direct correlation with the disease itself [14].
Concerning the aims of the paper we can say that concomitance of smoking and psoriasis may increase drastically the risk of cardiovascular disorders, not only due to the concomitance of two risk factors, but also due to the synergistic effect that smoke has on the natural history of psoriasis.
Role of smoking in microbiota and psoriasis
In the last years exciting new discoveries have been made about the gut microbiota and its role in many pathologies, one of these being for sure psoriasis, in which patients seem to host peculiar strands of bacteria, understanding the role of smoking on the flora can be ground-breaking for further study.
Using metagenomic shotgun sequencing analysis, Todberg et al. found out that psoriatic patients have a less rich metagenomic species compared to healthy patients, with an aberrant microbiota in patients with psoriasis. The microbiota is even different from the one of other inflammatory disorders such as inflammatory bowel disorders and multiple sclerosis, hence suggesting that many factors of the disease play a role in the flora. Metabolic syndrome itself seems to have a role in the development of an abnormal gut microbiota: insulin resistance seems to be associated to flora alteration, we can say the same in obesity, with an increase of Bacteroides and a decreased presence of Faecalibacterium strands.
Spondylarthritis is one of the diseases in which the alteration of gut microbiota is better documented and, being associated to psoriasis, it is safe to assume that there could be a shared bowel dysbiosis in the two disorders [15]. In an article by Buhas et al., it is shown that other strands of bacteria are altered. In particular, a correlation with either an increase or decrease in the Prevotella species is shown. Also, the microbiota changes according to the markers expressed: with IL-2 expression we have a concomitant increase in Phascolarctobacterium and decrease of Dialister species, their abundance may be a predictor of psoriasis severity.
Some microbiota-targeting therapy, especially probiotics and dietary adjustment are being evaluated, we think this could be a ground-breaking innovation in the field of treating psoriasis and one worth more focus from the scientific community [16]. Todberg et al. noted an increase in 4 specific species: Bacteroidetes, Firmicutes, Proteobacteria and Actinobacteria were the most abundant. Akkermansia are decreased especially in PsA, their alteration is associated with gut degradation in a murine study [17].
The role of smoking in gut microbiota is well documented by Capurso et al. [18]. Even though specific studies on the effect of smoking in gut microbiota in psoriasis were not found, according to the authors it is safe to assume that, since smoking can cause an alteration of the gut microbiota and there is a correlation between microbiota alteration of psoriasis, smoking can be one of the factors involved in its alteration, further studies should be conducted to assess the issue (Table 2).
Table 2
Studies of microbiota alterations in smokers
Smoking and psoriatic arthritis
Even though the relationship of psoriatic arthritis (PsA) with smoking would seem obvious, data are controversial, and many articles show different outcomes when assessing the association. In an article by Pezzolo and Naldi, 2 case-control studies are reported in which no correlation seems to be involved in PsA, in one we may also see a reverse association between the two. However, the same article reports a large-scale study that demonstrates a risk increase in PsA in the smoking population (RR = 1.54 for past smokers and RR = 3.13 for current smokers). In another study the report is of a risk increase compared to general population, but a reverse increase compared to psoriatic patients [19].
Similar results are found by Gazel et al., in a meta-analysis evaluating the prevalence of PsA among smokers, a decreased prevalence was found in patients with psoriasis (OR = 0.70) while in the general population the prevalence was found increased in half of the studies while in other three no association was found (OR = 1.10). The prevalence of PsA in psoriatic patients who smoke is also correlated to the quantity of smoking, it becomes particularly evident in patients that smoke between 15 and 25 cigarettes per day [20].
In conclusion, we may say that the correlation between smoking and PsA is directly positive in the general population while reversely positive between the psoriatic patients, this phenomenon is referred in the literature as “smoking paradox”. For this phenomenon we have both methodological and physiopathological explanation; while it seems that smoking has an effect on Toll-like receptors and reduces the activity of both IL-1 and IL-8, methodological explanations seem to be, according to Pezzolo and Naldi, the most relevant: the authors believe that the effect of smoking on PsA is totally dependent on the one on psoriasis, hence, the restriction of the analysis to patients with psoriasis which is a group on the causal pathway between smoking and PsA, was able to reverse the true association between smoking and PsA [19]. Nguyen et al. confirm the smoking paradox through their study: compared to the general population in which the HR for PsA in smokers vs. non-smokers was 1.27, comparing the same groups in a psoriatic population we have HR decreased to 0.91 [21].
Cancer risk in psoriasis
Smoking is the main risk factor in many cancers, the correlation between smoking and psoriasis leads to think about the possibility that there could be an increased risk of cancer development in psoriatic patients. A meta-analysis by Vaengebjerg et al. studied the correlation between psoriasis and cancer. The study showed a high correlation of all kinds of cancers, including keratinocyte cancers, lung cancer and non-Hodgkin lymphomas. Prevalence of overall cancers among psoriatic patients was 5.74%, while PsA was greatly associated with breast cancer. While considering the treatment, the prevalence of cancer seems to be lower in patients under biologic treatment when compared to patients treated with first-line drugs. For keratinocyte cancer the exposure to sunlight is the main risk factor, patients on treatment with PUVA showed a higher risk of keratinocyte cancer.
The increase in prevalence of cancer seems to be dependent mainly on therapy and lifestyle, especially behaviours such as alcohol consumption and smoking, very common in the disease [22]. Another meta-analysis by Trafford et al. had similar results to the previous, in addition it also assessed mortality for cancer and it showed an increased RR of 1.25 for overall cancers, while considering site specific cancers, 3 had an increase in incidence higher than the others: oesophageal cancer (RR = 2.53), liver (RR = 1.43) and pancreas (RR = 1.31). Even though more and more evidence of the correlation between psoriasis and the risk of cancer and cancer mortality is found, the guidelines for treatment of psoriasis are not adapted to this knowledge [23].
Treatment of psoriasis and smoking
Another way in which smoking is affecting psoriasis is through the alteration therapy: through both acting on the effect of the drug and on compliance to therapy. Zhou et al. also studied the impact of smoking on treatment, finding that smoking negatively affects the treatment of psoriasis at 6 months, with an OR for disease improvement of 0.80, with an inverse correlation to smoking. Current smoking seems to interact especially on TNF-2 inhibitors and in general mainly involves biologic agents. However, only one study was found regarding the role of smoking in the first-line therapy such as methotrexate, cyclosporin and acitretin [3]. In two independent studies it was shown that smoking patients with psoriasis have a lower compliance to treatment, leading to reduced remission of the disease [24].
Smoking also seems to induce the Tumour Necrosis Factor Converting Enzyme (TACE) and inducing inflammation, this is especially true after treatment with NB-UWB and is directly correlated to the number of cigarettes smoked, TACE levels and PASI score [25].
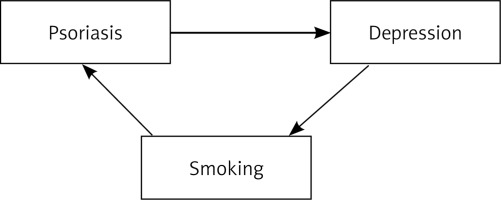
Smoking as a coping mechanism and the vicious circle of smoking and depression
Smoking is a well-known coping mechanism adopted by patients with psoriasis, being an invalidating disorder and due to the strong correlation with depression, the patient finds instant gratification in both smoking and alcohol consumption; if unaware of the correlated risk, this can become a threat to the patient’s health. According to Hayes et al., the prevalence of depression in psoriatic patients ranges from 10% to 62%, the wide range is probably due to the difference in clinical methods used and different kinds of population, especially the difference between in-patients and out-patients. Depression seems to be associated with severity of disease and lesion appearance, however, Psoriasis Area and Severity Index (PASI) does not seem to be a good predictive value for the risk of depression (Figure 2).
Depression seems to be associated with the quality of life of the patient: pruritus, poor sleep quality and the stigmatization related to the poor understanding by the general population of the disease seem to be the most important factors involved in this association; however, a pathogenic hypothesis has been made involving the activation of some factors such as nerve growth factor, substance P, and mast cell activation upon activation of the hypothalamic pituitary axis and sympathetic nervous system [26].
Patients would be using cigarette smoking as a coping mechanism to relieve depression and anxiety; it is safe to hypothesize that this behaviour will trigger a vicious circle in which smoking triggers psoriasis which will trigger depression and anxiety and so forth. Hence, assessing the role of depression in psoriasis seems to be a yet to understand by the community but a fundamental aim in our scientific work.
Through the treatment of depression we may also favour smoking and drinking cessation, hence improving the quality of life of the patient and inducing a better remission and response to treatment. However, carefulness must be used during smoking cessation as it seems to induce depression through the action on the hypothalamic-pituitary-adrenal axis. Hence, a proper caring for the patient and introduction of alternative coping mechanisms is fundamental [27].
A proposal for alternative coping mechanisms
We would like to conclude by assessing some methods of relaxation that the patient can use as an alternative to cigarette smoking:
Physical exercise is a well-known lifestyle behaviour promoting relief of stress, mild to moderate exercise may be introduced in patient’s lifestyle to promote both smoking cessation and stress reduction. This might also aid the patient in controlling the metabolic syndrome associated to psoriasis and reduce the psoriatic march [28].
Meditation seems also a good method to promote relaxation and stress relief, in a study by Goyal et al., it was shown how meditation has a moderate effect on both depression and anxiety, however there is no evidence that it can be an alternative to medical therapy [29].
Balneotherapy in thermal water seems to be a promising addition to the treatment of psoriasis due to both its direct effect on the skin lesions and also due to a notable effect on stress relief which assists the healing process as well [30].
Acupuncture is a traditional Chinese medicine technique consisting of inserting needles in the skin of the patient, it has been reported how depression severity is decreased in these patients [31] and it has been used as an alternative to pharmacotherapy for psoriasis [32]. However, we have to state that some controversies are present due to the fact that acupuncture may be a trigger for inflammation in active status and thus for psoriasis, this is called Koebner phenomenon [33].
Even though all these coping mechanisms are beneficial and appreciated by the patient, psychological therapy remains the best treatment for a patient in distress and it may be good to be given in patients with psoriasis-related depression and anxiety in the form of cognitive behavioural therapy [34].
Conclusions
About 1.18 million of people worldwide are smokers. Reduction of the smoking population is a fundamental goal for workers in the healthcare system to improve the quality of life of our patients and especially in patients with psoriasis. Knowing all the implications and providing our patients with an alternative to smoking is an essential goal that we have to seek as both researchers and clinicians along with providing our patients with constant support through the process and until quitting.