Aortic dissection type B is a cardiovascular emergency of the descending thoracic aorta, which can lead to visceral malperfusion, a potentially life-threatening complication. Mortality rates of acute visceral ischaemia have been reported to be as high as 25% to 62% [1–3]. As well as pharmacotherapy, other therapeutic options are available to restore intestinal blood flow, including various endovascular and surgical procedures [2].
We report a case of a 53-year-old woman who presented with constant central abdominal pain that radiated to the back. Abdominal symptoms occurred approx. 30 days prior to hospital admission and were followed by recurring vomiting and diarrhoea. There were no relieving factors and no other associated symptoms – in particular, there was no chest pain, urinary symptoms, or neurological deficits. Her medical history included well controlled arterial hypertension. She had no smoking history and was an occasional drinker. Physical examination did not elicit any findings apart from mild abdominal distension, epigastric tenderness, and decreased intestinal sounds. Her chest was clear with normal heart sounds, and blood pressure was 140/85 mm Hg. The blood pressure in the right arm was unfortunately not documented. All other observation readings were within normal range. The results of liver and kidney function tests, electrolytes, amylase, lipase, and cardiac enzymes were within normal range. Inflammatory markers were raised, with a C-reactive protein level of 105.3 mg/l (normal value, < 10.0 mg/l) and a leukocyte count of 14,590 per cubic millimetre (reference range: 4000 to 10,000 mm–3). Except for a moderately prolonged prothrombin time of 18.20 s (reference range: 10.4 to 12.5 s), the results of blood and coagulation tests were unremarkable. A 12-lead electrocardiogram indicated no abnormalities. On presentation her abdominal ultrasound and chest radiography were normal. She was sent for an emergent esophagogastroduodenoscopy. The findings are shown in Figure 1. Small bowel infarction was suspected, and she was transferred for an emergent computed tomography (CT), which revealed thickening of the duodenal wall and Stanford type B and DeBakey type IIIb acute aortic dissection (AAD), starting from the left subclavian artery, running along the aortic arch and descending aorta, and reaching distal to the right common iliac artery (Figure 2). The patient was referred for endovascular stent grafting.
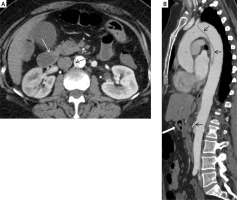
Figure 2
Thickening of duodenal wall (white arrow) and dissection of the abdominal aortal wall (black arrow)
Intestinal ischaemia/necrosis caused by aortic dissection is extremely rare. In a review of 384 type B dissections, mesenteric ischaemia was seen in 5% compared to malperfusion (renal, mesenteric, or limb) in 21% and acute renal failure present in 14% of patients [4]. However, literature data indicate that during the course of aortic dissection mesenteric ischaemia and acute renal damage are more frequent in men. This conclusion arises from computed tomography angiography (CTA) data clearly showing that involvement of the coeliac trunk and superior mesenteric arteries is more frequently seen in men [5]. The International Registry of Acute Aortic Dissection (IRAD) study evaluated differences in clinical features and outcomes of males and females with AD. The IRAD study reports that the ages of onset are 60.3 ± 13.7 and 66.7 ± 13.9 years for men and women, respectively [6, 7]. However, a recent Asian study showed that the mean age of onset for men can also be earlier compared with women (49.6 ± 12.6 years and 54.2 ± 12.4 years, respectively) [5]. The overall outcome of women can be worse than that of men regarding death rate, including 30% higher in-hospital mortality than men, probably because AAD occurs in women an average of 10 to 14 years later than men. Moreover, it was also shown that impending rupture occurs more often in women [4, 7–12].
There are a limited number of reports on aortic dissection (AD) presenting as chronic abdominal symptoms, and none of these pertain to middle-aged women [2]. What also makes this clinical case unique is that the patient had no history of severe cardiovascular or connective tissue disease. The clinical presentation was chronic central abdominal pain that radiated to the back due to the advancing involvement of the coeliac axis and the mesenteric artery. It is noteworthy to mention that at the time of hospital admission, values of serum markers of bowel ischaemia or infarction were negative. This probably underscores the significance of a high index of suspicion while diagnosing aortic dissection during the emergency room workout. Therefore, because AD is a life-threatening condition, it should also be considered in patients with chronic abdominal pain alone, which may resemble common peptic presentation.











