An acetabular or hip socket fracture is an infrequent affliction as compared to the analogous fractures of the upper femur or femoral head (hip fractures). While the incidence of acetabular fractures in India is yet to be established, the United Kingdom and France, for example, report an annual incidence of 3 per 1,00,000 and 4.95 per 1,00,000, respectively [1–3].
Neuraxial anaesthesia is a preferred choice for acetabular or analogous hip fractures for many anaes-thetists. It provides excellent surgical anaesthesia and perioperative analgesia and helps to avoid the risks associated with general anaesthesia. Acetabular fractures are associated with severe pain, which is a deterrent to positioning these patients in a sitting posture to perform neuraxial anaesthesia. Traditionally, systemic opioids, femoral nerve blocks, plane blocks such as fascia iliaca block, and more recently, pericapsular nerve group (PENG) block have been used for positioning these patients. Regional anaesthesia techniques such as fascia iliaca compartment block (FICB) are now increasingly used to set the patient in a sitting posture with better results, pain relief and comfort to perform neuraxial blocks in patients with hip and femur fractures [4–7]. PENG is a regional technique where local anaesthetic is deposited over the hip joint capsule [8]. Fracture of the capsule of hip joint in acetabular fractures precludes the use of PENG block in our study. The FICB is another fascial plane block where the drug is deposited between the ilio-psoas muscle and the fascia iliaca covering it. It aims to block three primary nerves – the lumbar plexus femoral, lateral cutaneous nerve, and obturator – with varying success rates. These are the nerves that provides sensory supply to the femur, neck, and the anterior lip of the acetabulum. Using ultrasound and a recent suprainguinal approach for fascia iliaca block has improved its reliability and has already been used with good results in hip surgery [9–12]. Unlike hip surgery, there is a paucity of studies on pain management in acetabular fracture surgery. We conducted a randomized controlled pilot study to compare the analgesic efficacy of ultrasound-guided suprainguinal fascia iliaca block (SFICB) to intravenous fentanyl in positioning patients with acetabular fracture for the neuraxial blockade.
METHODS
Ethical approval for this study (ethical committee no. IECPG-623/19.12.2019) was provided by the institutional ethical committee of the All India Institute of Medical Sciences, New Delhi, India on 28th February 2019. This study was also registered in the clinical trial registry of India (CTRI/2019/ 03/018179). Patients above the age of 18, with American Society of Anesthesiologists (ASA) physical status I–III, referred for elective surgical repair of acetabular fractures (anterior column fractures, anterior column-posterior hemi-transverse fractures, associated both column fractures) by the iliofemoral, ilioinguinal or Stoppa approach were enrolled in the study. The procedure with advantages and possible complications was explained to all the patients eligible for the study. Patients who refused to participate or with contraindications for neuraxial blockade, known allergy to local anaesthetic drugs, neurological deficit, or haemodynamic instability were excluded from the study.
Patients were randomly assigned, using computer-generated random numbers into 2 groups, wherein they received either fascia iliaca block (group B) or intravenous fentanyl (group F) for positioning. The visual analogue scale (VAS) score was explained and used to assess pain (0 = no pain to 10 = worst possible pain) during positioning. After randomization of the patients as per the group, the allocation and intervention as per the group were performed in a preoperative block room by an anaesthetist experienced in ultrasound-guided regional techniques. After the intervention, another anaesthetist, blinded to groups i.e., our primary investigator, collected the post-intervention outcomes and performed the neuraxial block. The analyst assessing the data was also blinded to the group allocation.
Baseline
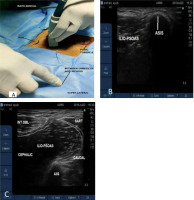
Patients were asked to sit with help to the best possible sitting position with bearable pain. Before any intervention, the baseline VAS score for pain was obtained in the supine and sitting positions. The degree of sitting achieved was measured in terms of sitting angle (SA) using a goniometer (Figure 1) A patient lying supine had an SA of 0 degrees, while a patient sitting fully upright had an SA of 90 degrees.
Group B, fascia iliaca block (FICB) [10–12]
An anaesthetist experienced in sonoanatomy and sonography-guided regional techniques performed the block using a high-frequency linear ultrasound probe (6–13 MHz, SonoSite M-Turbo. Bothell, WA, USA). The probe was placed over the anterior superior iliac spine (ASIS), in an oblique orientation with the marker pointing towards the midpoint of the line joining the xiphoid process and the umbilicus (Figure 2A). The hyperechoic shadow of the ASIS was identified (Figure 2B), and the probe was just slid down from the ASIS infer-medially along the line of the inguinal ligament. A superficial bow tie or an hourglass pattern can be appreciated, formed by two muscles – the sartorius infer-laterally and the internal oblique located super- medially. The muscle belly of the iliopsoas with its overlying fascia iliaca and underlying hyperechoic anterior inferior iliac spine was visualized beneath the hourglass shape to confirm the correct probe position (Figure 2C). A 5–8 cm nerve block needle (B. Braun, Stimuplex Ultra 360 22G) in an in-plane approach was introduced inferiorly to the inguinal ligament and advanced to reach the fascia iliaca above the inguinal ligament. 30 mL of 0.25% ropivacaine was injected into the fascial plane. The local anaesthetic spread can be seen over and across the surface of the iliac muscle, spreading cranially to the iliac fossa towards the lumbar nerve roots.
Group F or fentanyl group
A bolus of intravenous fentanyl 0.5 μg/kg was given to patients belonging to group F for positioning. After a time interval of 30 minutes in group B and 5 minutes in group F, the patient was handed over to another anaesthetist, who assessed the VAS score again in the supine position. If the VAS score was ≤ 5, the patient was asked to sit, and SA and VAS scores were again measured. If VAS scores were > 5 or there was a failure to achieve adequate positioning due to pain, additional boluses of intravenous fentanyl 0.5 μg kg–1 up to a maximum of 2 μg kg–1 were given in both groups. When other supplements of fentanyl failed, the patient was taken up for surgery under general anaesthesia or the neuraxial under lateral position was attempted.
After successful positioning, an anaesthetist blinded to the intervention performed a combined spinal and epidural neuraxial block. A dose of 10 mg, 0.5% hyperbaric bupivacaine with 25 μg fentanyl was administered through an intrathecal route to each patient. The anaesthetist was asked to provide a subjective assessment of the quality of patient positioning (0 – not satisfactory, 1 – satis-factory, 2 – good, 3 – optimal). Patients were also observed and scanned for complications, including respiratory depression, nausea, vomiting, profound sedation with systemic opioids or haematoma, local anaesthetic toxicity, etc., with fascia iliaca block. Intraoperative patients were operated on under neuraxial anaesthesia with occasional supplementation of injection midazolam. In the postoperative period, patient-controlled epidural analgesia (PCEA) was initiated at the rate and settings of 3–5 mL hr–1 as a background infusion and 2.0 mL (or 0.5 mL) on demand, with a 15 min lockout during a 48 h period. The PCEA regimen was composed of fentanyl (5 µg mL–1) plus ropivacaine (0.125–0.25%).
The study’s primary outcome was to compare the efficacy of the fascia iliaca block in facilitating positioning for neuraxial block by providing analgesia, measured in terms of sitting angle after the intervention and improvement in the SA and VAS scores before and after the intervention. The secondary outcomes were a comparison of total opioid consumption, quality of positioning for neuraxial block after the intervention, and the presence of any side effects in both groups.
Statistical analysis
Considering the low incidence of acetabular fractures and the lack of any previous study, we decided to conduct a pilot project with a sample size of 20. The assumption of normality was assessed by the Kolmogorov-Smirnov test. Normally distributed continuous variables were expressed as mean and standard deviation (SD) and non-normally distributed and categorical variables were expressed as the median and interquartile range (IQR). Binary variables were expressed as absolute numbers and proportions and compared with Fisher’s exact test. The Mann-Whitney U test was used to compare categorical variables and non-normally distributed continuous variables. A P-value of less than 0.05 was considered statistically significant for all tests.
RESULTS
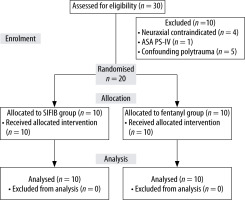
A total of 30 patients were assessed for eligibility during the study period, out of which 20 were recruited, with 10 patients allocated to each group (Figure 3) The demographic variables age, sex, weight, and physical status (ASA) were comparable in both groups. All patients in both groups were male.
Hemodynamic variables, i.e., heart rate and blood pressure measured before and after intervention, were similar between the groups. An assessment of baseline sitting angle and VAS score revealed an insignificant difference between the groups.
After the intervention, although SA was better in the block group than the fentanyl group, the diffe-rence was not statistically significant. However, when the improvement, measured as the difference in SA achieved after intervention, was compared, significance was found (Mann-Whitney U = 85, P = 0.006) in patients who received the block (27.5° [20.75–36.5°]) (Table 2).
TABLE 1
Demographic data of study population
TABLE 2
Baseline and postintervention VAS score, sitting angle (SA) and improvement in SA
When VAS scores were compared between the groups, the postintervention VAS score was lower in group B as compared to group F both in supine and sitting positions. Still, a statistically significant difference was only noted in the sitting position (5.9 ± 2.1 vs. 3.5 ± 1.5, P = 0.01) (Table 2).
When opioid consumption was measured in both the groups, group F had significantly higher me-dian opioid consumption in comparison to group B (Mann-Whitney U = 0.0, df = 18, P < 0.05) (Table 2). Only one patient required rescue analgesia in group B as compared to 4 patients in group F. Positioning even failed in 1 patient in group F despite 2 boluses of rescue analgesia. The anaesthetist performing the block found no difficulty recognizing the sono-anatomy, visualising the needle, or performing the block in any cases. None of the patients deve-loped complications in either of the study groups.
Subjective positioning assessment was observed by the blinded anaesthetist performing neuraxial block, and was also statistically significantly different between the two groups. While 70% of patients in group B could achieve an optimal position, only 10% of the patients in group F could achieve the same to perform the neuraxial block. 20% of the patients in group F had unsatisfactory positioning (P score – 0) (P = 0.02) (Table 3).
DISCUSSION
Pelvic and acetabular fractures comprise only 3% of all orthopaedic injuries reported to a trauma centre. Most of these happen from high-impact events such as a car accident or falling from a significant height. These can be categorized into two broad types – stable and unstable. While the most stable fractures are managed conservatively, unstable fractures may often require surgical intervention. With recent advances in pelvic implants, intraoperative imaging, and a more advanced understanding of injury, there has been a shift towards more operative management of pelvic fractures that were previously treated non-operatively [13, 14]. Despite these developments, acetabular fractures are still not so frequent in the theatres, and there is a dearth of literature on anaesthetic management and analgesic techniques for these fractures.
Conventionally CSE is the anaesthetic technique of choice for many anaesthetists as it provides dense anaesthesia during and adequate analgesia after surgery [15]. Acetabular procedures are complex and often performed simultaneously for associated lower limb fractures, leading to prolonged surgery. This further led to accentuating the need for CSE. As these patients planned for surgery have multiple unstable fractures, they are often in severe pain, a major deterrent for positioning them for neuraxial block. Positioning for CSE further adds to the difficulty, needing better positioning and more time. Therefore, there is an increasing need for a technique that could help patients sit comfortably for CSE with minimal pain. Regional techniques such as femoral nerve blocks, PENG, and fascia iliaca blocks have recently revamped the analgesic choice for positioning patients with hip and femur fractures, with good results [5–7, 16–18]. There is, however, a lack of literature on these blocks for pelvic or acetabular fractures.
Chelly et al. described the successful use of a continuous lumbar plexus block after surgery in patients with acetabular fracture under general anaesthesia [19], and in a case report Elena et al. described the use of a constant quadratus lumborum type 2 block in a patient with complex iliac and acetabular fracture [20].
Fascia iliaca block is another block shown to provide better analgesia compared to systemic opioids for positioning of patients with hip and femur fractures [5, 7, 16–18]. We used a supra-inguinal approach for FICB for positioning in patients with acetabular fractures in our study. Suprainguinal is a relatively new and prudent approach for fascia iliaca to block the femoral, LFCN, and obturator nerves reliably. It offers the convenience of a single injection of local anaesthetic beneath the iliac fascia, in a cephalad direction towards lumbar nerve roots, and thus provides complete sensory block and has shown better results than its precedent infra- inguinal approach [11, 21].
To the best of our knowledge, this is the first study assessing and comparing the use of a regional technique and systemic opioids for positioning of patients with acetabular fractures for CSE.
We assessed the degree of sitting achieved or sitting angle, pain scores in supine and sitting position before and after intervention and quality of positioning for the anaesthetist in charge to perform neuraxial block.
It is known that pain associated with fractures is further worsened by movement. In our study, while there was no significant difference in the post-intervention VAS scores in the supine position, there was a significant difference in reduction of VAS scores in the sitting position in group B. This is probably because the analgesia provided by fentanyl was not sufficient to take care of the exacerbated pain due to movement of the fractured joints. Four patients required supplemental fentanyl to position, and we even failed to position one patient in the fentanyl group.
We also measured sitting angles and asked the anaesthetist performing the block to rate the quality of positioning to measure of effect of each intervention in positioning. We found that suprainguinal FICB resulted in significant improvement in sitting angles compared to intravenous fentanyl. Anaesthetist assessment of patient positioning for neuraxial block was also significantly better (70%) in group B as compared to only 10% in group F (score = 3). Further, 20% of patients were even rated unsatisfactory (score = 0) in the fentanyl group. In line with these findings, the requirement of rescue analgesia was also lesser in group B with only one patient requiring rescue analgesia in the form of i.v. fentanyl 0.5 μg kg–1 once, as compared to 4 patients in group F, two of whom required rescue boluses twice.
No complications were documented in patients from our study related to block or intravenous opioids. This may be because most members of our study population were younger (35–45 years) with minimal comorbidities. There was a risk of local anaes-thetic systemic toxicity in our patients, consi-dering the high volumes of local anaesthetic required for the block and again in epidural for peri-operative analgesia. However, we did not encounter any in our study – the local anaesthetic dose was always calculated to ensure that safe limit.
The results of our study are similar to previous studies comparing FICB to systemic fentanyl for positioning patients with hip or femur fractures for neuraxial block. Both Rajashree et al. and Yun et al. in their studies noted lower VAS scores, better sitting angles and better quality of positioning in the FICB group. In these studies, the time required to perform spinal anaesthesia was also noted to be significantly lower in the FICB group [6, 16]. We surmise that the supra-inguinal FICB, in our patients with acetabular fractures, reliably blocks three of the major sensory nerves and provided superior analgesia than fentanyl, particularly during movement, better sitting angles and optimal position to perform neuraxial block.
LIMITATIONS
Our study had several limitations and biases. First, as this pilot study was conducted on trauma patients undergoing surgery for an infrequent acetabular fracture, the sample size was small, and only male patients were included. This severely limits the study; thus, the results may not reflect the gene-ral population. The patients who presented for surgery had varying severities of fracture and time since the fracture incident. We also did not unify, gather, or assess the preoperative analgesic details of the patients. These data were not obtained and may affect the outcome. Further, there was no sham block for the patients who received only fentanyl; this prevented the patient from being blinded and can lead to bias in the results. Lastly, the acetabulum also receives sensory innervation from the scia-tic nerve, gluteal nerve, etc., which would not be blocked by suprainguinal fascia iliaca block.
However, we consider our use of this block justified, as its purpose was to provide adequate analgesia to achieve an optimal position for neuraxial block which would then serve as the primary analgesic modality.