Introduction
Parkinson’s disease (PD) is a neurological disorder which can impact motor and non-motor functions, usually commencing over the age of 60. PD is a chronic disease, and it is the second largest neurological disease affecting an estimated 571 per 100,000 people in Europe with rising prevalence due to the aging population. In the United States, there are approximately 1.5 million patients with PD [1]. In Hungary, PD deaths were 398 or 0.35% of total deaths in 2020 [2]. The main cause of PD is the loss of brain cells called Substantia Nigra which are responsible for producing dopamine [3,4]. PD symptoms can be rigidity, tremor at rest, bradykinesia and postural instability. It can influence the balance and the gait in late stages [5]. Balance is a common serious challenge for PD people. Balance dysfunction is identified as one of the causes of poor quality of life (QoL), especially when it comes to difficulty in turning or standing, which may cause falling as a result of postural instability [5,6]. PD can also lead to mood disorders such as anxiety, depression and apathy. Almost 45% of PD patients suffer from anxiety [1]. In addition, apathy is a frequent psychiatric disturbance that can be obvious even earlier than the motor symptoms of PD [7]. The traditional way of PD curing as a motor disorder is by dopaminergic medication. In the last decades, non-pharmacologic interventions started to be used to treat PD patients [5]. It has recently been shown that regular exercises and rhythmic movements can improve bradykinesia symptoms in PD. In addition, physical activity (PA) increases survival and prevents people from chronic diseases [7]. According to the literature, movement therapy improved balance and gait function led to better QoL in PD patients. While benefits can be obtained with a short dance intervention, longer interventions prove to be more effective [8]. Although PA improves specific aspects of physical fitness by using multiple compensatory strategies as a therapeutic approach, many questions are still unanswered [9,10]. Based on the above presented, we are conducting this study to investigate the effect of dancing on PD patients as a non-pharmacological treatment.
Aim of the work
This research aimed to determine the effect of dancing on PD patients as a non-pharmacological treatment, by evaluating general and specific health status, and QoL of PD patients and by measuring balance at baseline and after 10 weeks of participating in dance classes.
Material and methods
Research design and setting
This was a quasi-experimental, interventional, follow-up study using validated questionnaires and clinical tests. The research took place in Vasutas Művelődési Ház Pécs, Hungary, in cooperation with the Parkinson Dance Group of the Parkinson Association.
Participants
In this research, we targeted the PD patients. The estimated number of participants in the intervention group (IG) was 20, but due to Coronavirus Disease 2019 (COVID-19) we had difficulty keeping in contact with the patients. Only 8 participants could take part in the research until the end. Due to COVID-19, some participants were not able to attend the dancing class. The control group (CG) included 15 patients. Data were collected between February 2021 and January 2022.
Sampling technique
Non-random, consecutive sampling was used. The final sample was n=23. All patients had similar symptoms, tremors, freezing, and slowdown. The IG took part in dance classes, whereas the CG did not. Each class was held for 1 once/week. Some dancing classes moved online due to COVID-19 restrictions. The dancing training was structured into 4 parts using the chair as a core support. The first part involved breathing and warm-up while seated. The second part consisted of partnered exercises in a standing position at the same rhythm as the music. In the third part, the PD participants were asked to dance the tango. The fourth part was intended for relaxation and the PD participants were invited to wind down [11]. The IG had a physical examination: Balance Berg Test (BBT) and Four Square Step Test (FSST). Both groups filled out four validated questionnaires.
Adults over 18 years diagnosed with PD between stages 1-4 were eligible to participate if they had one of the following symptoms: tremors, freezing, and slowed movements. Patients with a Body Mass Index (BMI) higher than 35 and those with any physical and mobility impairments were excluded. None of the participants met the exclusion criteria.
Data collection tools
Sociodemographic Questions and Short Anamnesis: the questionnaire gave us more detailed information about the PD participants. It included age, gender, marital status, education level, employment status and current activity. Additionally, the patients were asked about their height and weight for BMI measurements, in addition to the walking aids they used.
Lifestyle Questions: this form focused on the PD participant’s lifestyle 5 years before and 5 years after diagnosis. The answers gave us specific information about coffee and alcohol consumption, smoking habits, in addition to eating habits.
36-item Short Form Health Survey (SF-36): the PD participants were asked to describe their usual activities related to 8 sub-scales. This helped us to evaluate the health status of our participants [11].
39-question Parkinson Disease Questionnaire (PDQ-39): the answers referred to the impact of the illness on the patient’s life in the previous month [12].
FSST: the first test took place on the 7th of October 2021, while the second test was on the 16th of December 2021. This test informed us about the PD’s patients balance ratio. The equipment required for the FSST was a stopwatch and four sticks [13,14].
BBT: following the FSST on the same dates, we could examine unsupported movement ability and body coordination in the IG [15,16].
Since the official language in Hungary is Hungarian, it was impossible to distribute the questionnaires in English. The SF-36 questionnaire was already validated in the Hungarian language. Concerning the PDQ-39 and the lifestyle questionnaires, they were both in English. Both questionnaires were translated into Hungarian and then content validity was checked by a panel of experts. Permission to use all questionnaires was granted. Additionally, the instructions for the BBT and FSST tests were in Hungarian.
Data analysis
SPSS version 26 was used to analyze the data. For descriptive statistics, frequencies and percentages were used for categorical variables, and mean and Standard Deviation (SD) for continuous variables. The Kolmogorov- Smirnov test was used to check the normal distribution of the data. For variance analysis of categorical variables, the Chi-square (χ2) test or Fisher’s exact test was used to compare the variance in the dependent variable across the independent variable. Meanwhile, for numerical variables (mobility, FSST, BBT), the Wilcoxon test, Mann-Whitney-U test, paired sample T-test and One-way ANOVA tests were used to conduct the variance analysis. The significance level was set at p<0.05.
Ethical considerations
Participants were informed about the research’s aim and methods before signing the informed consent form. The investigation conformed to the principles outlined in the Declaration of Helsinki. Voluntary participation and the ability to withdraw from or leave the study at any point without a reason and without feeling an obligation to continue. Anonymity and confidentiality were guaranteed for the participants. All possible sources of harm to participants were considered and mitigated. To ensure the safety of the participants, a trained dance physiotherapy instructor was present during the intervention sessions, sometimes accompanied by an expert neurologist. The study was approved by the Regional Committee for the Research Ethics of the Clinical Centre of the University of Pécs (Record number: 8838-PTE 2021).
Results
Main characteristics
Within the IG, 37.5% were male, 50% had additional illness and 37.5% used walking aids. However, in the CG, 60% were male, 46.7% had additional illness and 13.3% used walking aids. The average age and the BMI of the IG were higher than that of the CG. The detailed social demographic and anthropometric data of both groups are presented in Table 1 and Table 2.
Table 1
Demographics of the PD participants
Lifestyle
No change in coffee consumption habits among the participants in both groups (IG and CG) was observed between the last 5 years and the current month. Concerning sleeping quality, we noticed a higher difficulty of sleeping in participants of both groups of the current month compared to 5 years ago. The details of the lifestyle questions are presented in Table 3.
Table 3
Lifestyle questionnaire results
General health status
Based on SF-36, 60.9% of the PD participants reported bearable, 17.4% bad, 13.0% good and 8.7% very good health status. As shown in Table 4, 13.3% of the CG and 37.5% of the IG reported good or very good health, although this was not significant (p=0.681). Bad health was reported by 20.0% of the CG and 12.5% of the IG. More than half of the PD participants stated that they did less than they wanted due to PD. 12.5% of the IG stated that their health was much worse than a year ago compared to 20% in the CG. The details of lifestyle questions are presented in Table 5.
Table 4
Health status of PD participants
| Health status | Intervention group (n=8) n (%) | Control group (n=15) n (%) | p-value |
|---|---|---|---|
| Very good | 1 (12.5) | 1 (6.7) | 0.682 |
| Good | 2 (25.0) | 1 (6.7) | |
| Bearable | 4 (50.0) | 10 (66.7) | |
| Bad | 1 (12.5) | 3 (20.0) | |
| Total | 8 (100.0) | 15 (100.0) |
Table 5
Health status now compared to a year ago for both PD groups (n=23)
Parkinson’s disease-specific quality of life
According to PDQ-39, the IG had higher mobility (p=0.873), better performance while doing the daily living activities (p=0.083), emotional well-being (p=0.082), cognition (p=0.335), and communication (p=0.811) than the CG but the results were not significant. The details of the 8 sub-scales of the PDQ-39 is shown in Table 6.
Table 6
PDQ-39 questionnaire results
The CG reported experiencing strong or very strong physical pain, while those in the IG did not. Additionally, 73.3% of the CG reported slight restrictive pain, while only 37.5% of the IG reported the same. The IG were worried about falling in public more often than those in the CG, although a few IG participants never felt worried about falling in public. According to our results, more of the IG cooked independently and more often than the CG. However, the IG participants had PD symptoms more frequently than the CG participants.
Regarding the variance analysis, the IG participants had significantly more severe writing problems (p=0.044) and feelings of anger (p=0.015) in the last month. There was a significant difference in feelings of isolation across genders among the CG participants (p=0.015). Additionally, there were significant differences in basic life activities such as cooking and dressing across age groups in the CG (p=0.008, p=0.048 respectively). The CG members with a higher BMI needed more help than those with lower BMI (p=0.01). Confinement to the home significantly varied among different age categories (p=0.036) in the IG.
Since there was not any significant difference in age and BMI between the IG and CG PD participants (p=0.092, p=0.401 respectively), we estimated some difference in relation to PDQ-39, but we were only able to describe significant difference based on the One-way ANOVA test by the mobility subscale (F=3.463, p=0.029) related to age categories but no significant difference was found related to BMI categories (F=1.875, p=0.179).
Berg Balance Test
Based on the results of the Kolmogorov-Smirnov normality test, BBT data appeared to deviate from normal. Therefore, the Wilcoxon signed rank test, a non-parametric test, was used to compare data, as an alternative to the paired T-test. A significant difference was not found based on the Wilcoxon test for the 14 BBT tasks. However, some differences were found in the personal data comparing the baseline and follow-up results of the 14 BBT task. The most difficult were the last 4 tasks, such as when the participants were asked to stand on one leg, which proved to be a major challenge. After the 10th week, the BBT results presented an improvement in each PD dancer and they were able to do almost all the tasks with a good score [3-4]. The IG could perform the BBT tasks more confidently and independently.
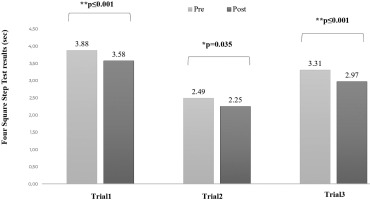
Four Square Step Test (FSST)
During the first week, the participants were not able to do the task properly from the first FSST trial, while they were able to do it during the second trial. After 10 weeks, the participants could do the task from the first trial. Additionally, the FSST second trial was faster than that of the first week. As shown in Figure 1, there were significant differences between the FSST results of the first (p≤0.001), second (p=0.035), and third (p≤0.001) trials between pre- and post-intervention measurements, where the participants were faster in the post-intervention measurements, especially in the first and third trials were the difference in time was greater than during the second trial. For more details about the FSST instructions and test results.
Discussion
Even though there is no cure for PD, medication, surgery, or reassuring care can relieve some symptoms. Pharmacological treatment barely improves balance dysfunction. However, many studies showed that movement therapy for PD sufferers who had balance dysfunction increased awareness and positive potential which led to better QoL and health status [6]. So, this study was conducted to investigate the effect of dancing on PD patients as a non-pharmacological treatment.
The average age of the IG was higher than the CG. As a result, the IG faced more challenges and difficulties than the CG due to the age differences [17,18]. Patients of more advanced age experience water loss, which may lead to several changes: starting from the bone structure due to loss of bone density, muscles weakness due to muscle mass reduction (sarcopaenia) and increasing body and visceral fat. All these changes could increase the risk of fractures [18].
Our findings showed that the IG reported better health than the CG, although the difference was not significant. This findings confirmed our hypothesis of the dancing classes program which helped to motivate and increase in PD symptoms tolerance and balance for each PD participant [5,19]. The results also showed that PD participants had to stop do some of the daily activities due to their health condition. The question regarding feeling calm or full of energy was relative because PD patients usually change their mood frequently depending on their strength [7,20]. Additionally, PD medications can lead to depression or anxiety [18], which can affect the patient’s activity and limit their movement. Dancing classes can foster acceptance and respect for each other’s problems. The PD participants may talk, share their thoughts and laugh, which may improve their social life [20,21]. Our results support this, in the sense that the IG presented better communication scores than the CG. During our research, attendance was almost complete, and the participants showed interest and were motivated to participate. Many studies showed evidence that the PD patients attended dance classes for social and emotional benefits as well [22].
As someone grows old, weight tends to increase due to health and mainly the loss of physical activity, so dance classes may fill this gap and help patients work on their physical and mental health together [7].The IG members were worried about falling in public more often than those in the CG, although a few IG participants never felt worried about falling in public. The main idea of practicing dancing was to boost confidence and alleviate the fear of falling. It could also reduce the embarrassment of having the PD generally [23].
Some studies have shown that when PD participants focused on the improvement and independence they achieved from the dance classes, they forget about their chronic disease and their symptoms [7,24] such as difficulties in sleeping and writing. Our results contradict these findings that the IG participants had more writing and sleeping problems, but our findings showed that the IG had could handle their daily activities independently, such as cooking and dressing than the CG.
Studies have shown that movement therapy can increase awareness and positive potential for PD patients with balance dysfunction, which enhances QoL [5]. Our IG participants felt less angry during the last month compared to the CG. There was a significant difference in feelings of isolation across genders among the CG (p=0.015). Gender could be a factor behind better or a worse health, which then leads to better or poorer QoL, depending on the structure and rules of a particular society. For instance, women are more likely to work in healthcare institutions, so they can take better care of themselves due to their knowledge. On the other hand, men work in different fields and have less knowledge about health. Females also generally are more likely to have check-ups due to their body hormones, during pregnancy, after menopause or the maturation period [25].
All dance classes started with warm-ups and breathing after standing and walking, which could have improved the IG patients’ stability after 10 weeks of dance participation. Based on some research, age can lead to a high BMI which limits movement and impairs balance [4]. The first week of BBT results clarified that the IG participants had already achieved good posture. We assumed that the reason could be because the PD dancing group in Pécs started 3 years ago. Therefore, the BBT tasks were not hard for most of them. Regarding the BBT results of the IG participants after 10 weeks, their gait and posture became natural and smooth. Their balance shifted to the center and all directions equally which led to a good performance in the FSST task. They were not afraid to fall as they had been 10 weeks before. According to our evaluation, dance classes could greatly improve their ability while standing on one leg for example which was the final and most difficult task for all the IG participants [26]. Concerning the FSST results, the IG participants needed time to analyze the moves and to put them in order before starting the task, which was normal for their age [27]. Dancing affects, the motor system and makes a major change in brain stimulation [5,6,26,28]. We assumed that dance activity could improve the participant’s motor skills and maintain good stimulation by avoiding PD symptoms such as tremors and moving to the rhythm of the music. This could increase the potential to change their mindset and encourage a new perspective. Our results support this, in the sense that after 10 weeks, the participants could do the task from the FSST first trial. There were significant differences between the FSST results of the first, second, and third trials between pre- and post-intervention measurements, where the participants achieved faster post-intervention measurements.
Limitations
Our study has some limitations. First, we excluded patients with communication problems and those with inappropriate mobility. Second, we could not control the participants’ medication pre- and post-dancing classes. Third, the physical tests were performed before or after the dancing class depending on the participants’ preferences. Fourth, some dancing classes were held online due to COVID-19 restrictions, which might have led to less effective intervention due to poor monitoring of participants. Finally, a limited number of participants were included in the IG due to COVID-19 restrictions thus, there is a need for additional research including a larger sample size using random sampling to examine the potential long-term effects of dance on PD patients.
Conclusions
To sum up, we assumed that dancing, as a non-pharmacological treatment, can be beneficial for the health status of people with PD. Our SF-36 results showed that the IG had better health than the CG but the difference was not statistically significant. Thus, we could not prove our hypothesis. We also assumed that QoL would be better in PD patients who are part of a dancing program than patients who are not. Our findings showed that the IG had greater mobility, better performance while doing the daily living activities, enhanced emotional well-being, advanced cognition and improved stigma considerably more than the CG however the results were not significant.
Finally, we assumed that PD patients’ balance would improve due to the dancing intervention. Our findings showed some improvement in BBT results after 10 weeks of intervention within the IG but the results were not significant. However, our results showed significant improvements in FSST results in all trials before and after 10 weeks of intervention. Thus, our hypothesis was confirmed. More research is needed to examine the potential long-term effects of dance on PD patients.