Widespread misconception that coronary artery disease (CAD) is a “man’s disease” should be overturned as current data show a growing incidence of CADs across Europe in women [1, 2]. The under-representation of women in randomized clinical trials (RCTs) in the area of coronary intervention (accounting for ~25% of patients) limits the generalization of RCT results to the decision-making process of individual females undergoing percutaneous coronary intervention (PCI) [3]. There are known sex differences in clinical presentation of CAD, in the anatomy – women having smaller vessels than men and treatment strategy – women are less likely to receive drug-eluting stents (DES) [4], what may be associated with worse results of PCI performed in different clinical scenarios [2, 3, 5–7].
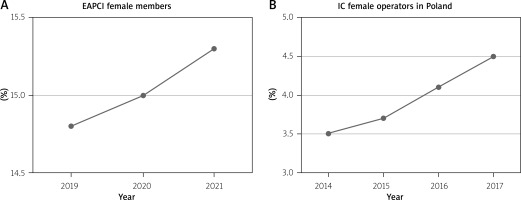
On the other hand, there is still a significant under-representation of women working as healthcare providers in interventional cardiology (IC), despite an increasing proportion of female medical students [8]. Moreover, very few of them reach senior leadership, academic positions, or act as principal investigators, as well as are actively involved in company advisory boards [8]. Analyzing the data from the European Association of Percutaneous Coronary Intervention (EAPCI), a small but steadily increasing proportion of female EAPCI members has been observed (Figure 1 A) [8]. IC still ranks at the bottom among other specialties in terms of female representation and very rarely the proportion of women in the IC area exceeds 20% [8]. Due to the low female representation in interventional fellowship programs, the gender gap appears unlikely to narrow in the near future [9].
The problem of the low number of females in IC is global. US data, women accounted for only 4% (412/9,179) of interventional cardiologists [10]. They performed 3% (n = 70,009) of all PCI procedures in different clinical settings, 77% of procedures were performed on patients the acute coronary syndrome, 3% on patients cardiogenic shock, and 16% on call, during the time period studied (between 1 July 2009 and 30 June 2013) [10]. Female interventionalists performed a median of 48 PCI procedures per year (interquartile range: 22–87), but generally in-hospital mortality was low (1.8%), and was not significantly different between female operators with high (≥ 50 cases/year) versus low (1.95% vs. 1.75%, unadjusted p = 0.12, adjusted OR = 1.03, 95% CI: 0.84–1.27) annual procedure volume [10].
Similar findings were observed in the first analysis of data from the Polish National Registry of PCI (ORPKI) [11]. A total of 31 female operators (4.1%) (Figure 1 B) performed 12,935 PCIs (2.8%) with a median of 75 PCI procedures per year (interquartile range: 43–154), whereas the median for male operators was 139 (interquartile range: 67–216; p < 0.01) [11]. There was no difference in clinical outcomes (a composite of all-cause death, bleeding at the puncture site, or coronary artery perforation) associated with the operator’s sex [11].
Due to the smaller number of females in IC and often limited possibility of their education and improvement in performing procedures, it may be appropriate to wonder whether operator-patient sex discordance exists. There are some studies showing that such a discordance was associated with an increased mortality after acute myocardial infarction (AMI) among female patients treated by male physicians, but no excess in mortality was observed for male patients treated by female physicians [12]. However, it is suggested that sex discordance between surgeons and patients negatively affects outcomes of patients undergoing common surgical procedures [13].
In this issue of the journal, Dziewierz et al. illustrated the results of the data analysis from the Polish National Registry of PCI (ORPKI) showing the impact of the operator-patient sex discordance on periprocedural outcomes of PCI [14]. Of 581,744 patients treated by 34 female and 782 male operators, 194,691 patients were sex discordant with their operator (a female operator with a male patient: 12,479; a male operator with a female patient: 182,212) while 387,053 were sex concordant (a female operator with a female patient: 6,068; a male operator with a male patient: 380,985). The primary endpoint was defined as all-cause periprocedural (in cathlab) mortality. Additional elements like other periprocedural complications, including stroke, cardiac arrest, coronary artery perforation, no-reflow, allergic reaction, and puncture site bleeding were also analyzed. The results showed that, among female patients, no difference in the risk of the composite of periprocedural complications between patients discordant versus concordant with operators was noted (2.70% vs. 3.02%; p = 0.14). Similarly, no difference in the risk of the composite of periprocedural complications (1.92% vs. 1.87%; p = 0.69) between discordant and concordant patients was observed among male patients. The risk of death (0.55% vs. 0.43%; p = 0.037) and bleeding at the puncture site (0.13% vs. 0.08%; p = 0.046) was higher in male patients discordant versus concordant with operators. However, all the differences in outcomes between male patients discordant versus concordant with operators were no longer significant after adjustment for covariates, except for the allergic reaction which was less in male patients discordant versus concordant with the operator. This does not seem to be related to the operator, but rather to the patient characteristics, for example an allergic reaction to contrast. The presented study did not show a detrimental effect of operator-patient sex discordance on periprocedural outcomes in all-comer patients undergoing PCIs. Differences in the baseline risk profile was associated with some of the observed differences in outcomes.
Similar results were obtained in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium’s DISCO study [14]. In this study, there were also no significant differences in outcomes: in-hospital mortality, acute kidney injury, transfusion or major bleeding among male and female patients undergoing PCIs performed by sex-concordant vs. sex-discordant operators [14]. Moreover, similarly to other studies, the DISCO study showed a small percentage of female PCI operators (4.5%), who performed only 2.66% of all PCIs [15].
Given the high interest in studying medicine by women, hopefully more female cardiologists will be involved in IC in the future. Not a large but still increasing number of females in IC is also observed in Poland. It seems that the preparation of appropriately adapted educational programs and, above all, the determination of barriers for women in starting and developing a career in interventional cardiology is crucial to their greater involvement in this field [8]. One of the key elements related to IC is radiation exposure, which is of great importance for women in the reproductive period or during pregnancy. A statement aiming to provide clear regulations on radiation protection for healthcare professionals working in catheterization laboratories during pregnancy has been recently published [16]. In order to reduce the barrier preventing women from accessing these careers, increased knowledge in the community is warranted.
Finally, such studies like the one presented by Dziewierz et al. in this current issue support equality of IC operators in terms of sex [14]. The next challenge is to create the conditions for equal development and successful career in interventional cardiology.