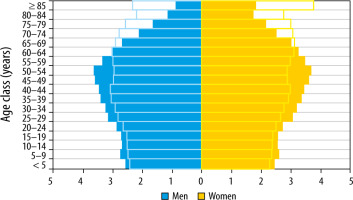
In Europe there are increasing numbers of old (more than 65 years old) and very old (more than 80 years old) patients (very old intensive care patients – VIPs) (Figure 1). In addition to combinations of chronic conditions (multi-morbidity), there are geriatric disabilities and functional limitations, with a profound impact on management in the ICU and afterwards [1].
THE ORIGINS OF THE VIP NETWORK
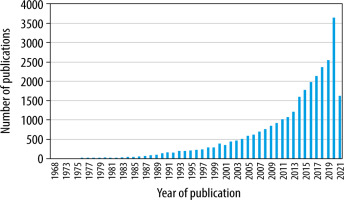
The rapid increase in the number of publications, as shown by the slope of the graph in Figure 2, indicates the increased interest in the area of VIPs.
A group based on the Health Service Research and Outcome Section (HSRO) of the European Society of Intensive Care Medicine (ESICM) decided to further advance the study of VIPs, and an initiative was launched at the HSRO Section meeting in Milan in October 2016. We describe herein the development and progress of the research network (VIP Network) that has grown out of these initial efforts.
The new VIP Network, with financial support from the ESICM (ESICM Research award for 2017), identified knowledge gaps both in how best to treat VIPs and in outcomes (survival and quality of life).
The VIP Network is led by a steering group which meets in person from time to time (e.g. at international research meetings, as well as at dedicated network meetings in Bergen, Norway, and Jerusalem, Israel [2]) and weekly by videoconference to discuss the research agenda. The steering group emphasizes shared decision-making and inclusiveness. The task of leading research projects has been distributed amongst the group members. Interested researchers from outside the core group are often invited to join projects. The steering group sets the agenda and the direction of study. Then, each country has a national co-ordinator to recruit suitable and interested ICUs. Such a system captures a very wide spectrum of countries and ICUs, but will still be affected by some degree of bias, in that only units with an interest in the topic and with the resources to carry out a project will be involved. This approach has resulted in the inclusion of tens of countries, hundreds of ICUs, and thousands of patients. The entire network is based on interest in the subject, collegiality, and goodwill.
Access to data and authorship of papers are both important for the smooth functioning of the network. Once collated, the de-identified data is available for use by all members of the network. Production of publications is open to all members of the network, with authorship (inclusion in the list of authors and order of inclusion) reflecting contribution to the publication.
THE MAIN VIP NETWORK STUDIES – VIP1, VIP2, AND COVIP
The VIP Network has undertaken 3 major studies (VIP1 [3], VIP2 [4], and COVIP [5]), in a multi-national setting involving approximately 30 European and Middle Eastern countries and in hundreds of intensive care units. These studies have been set up with modest funding (see Table 1) and despite the hurdles of differing ethical review board requirements in different jurisdictions. Clinical studies in Europe have faced the additional challenges of the General Data Privacy Regulation (GDPR) by the European Union since May 2018 [6]. The GDPR regards the protection of personal data as a fundamental right.
TABLE 1
Funding sources for the VIP group 2017–2021
The VIP1 study was undertaken rapidly after establishment of the VIP Network, with the first paper accepted for publication by September 2017 [3]. The focus of the study [3] (over 5000 patients) was the over 80-year-old group of patients presenting to the ICU. The main finding was that frailty, as measured by the Clinical Frailty Scale (CFS), was highly associated with 30-day mortality.
VIP2 (approximately 4000 patients) focused only on emergency admissions of VIPs to the ICU [4]. The occurrence of other “geriatric” syndromes such as co-morbidity, polypharmacy, activity of daily life, and cognition were also included. Frailty was again the best predictor of outcome.
The COVIP study (4000 patients) [5] was conducted during 2 time periods in 2020, coinciding with the initial 2 surges of the Covid-19 pandemic in Europe, and investigated the main predictors of hospital outcome in VIPs with Covid-19. The study also captured 30- and 90-day outcomes, as well as differences between the first and second surges of the pandemic.
The results of the above studies have been published widely (Appendix 1). The conduct of studies has been streamlined over time, with eCRFs and central data management, allowing for rapid data analysis and publication of results, whilst maintaining compliance with GDRP.
FUTURE PROGRESS
Current work is focused on further sub-analyses and publication of the COVIP data. The group is also strengthening alliances with multi-disciplinary groups, in particular geriatricians and rehabilitation experts, recognizing that intensive care is only one segment of the health trajectory of geriatric patients.
The group is exploring 2 further important areas of research. Firstly, the use of artificial intelligence to improve prediction of outcome at the individual level [7, 8]. Secondly, we are planning a study of time-limited trials (TLT) in VIPs. Because the outcome is so difficult to predict, the VIP is admitted to the ICU and given the benefit of full treatment. If he/she responds to treatment, then treatment continues at the same intensity, but if it becomes clear that the patient is deteriorating despite treatment, then de-escalation or palliation are considered. Other areas of interest for future study by the VIP Network are listed in Table 2.
TABLE 2
Future areas of study by the VIP Network [9]
The VIP group is making a concerted effort to engage legal and political entities, such as the Konrad Adenauer Foundation in Germany, with the ethical challenges faced by all intensivists.
CONCLUSIONS
The VIP study network is an example of a group of like-minded intensivists who are self-organized into an international network, recognizing a growing area of intensive care practice with unanswered questions, then tackling those questions by working together collegially and efficiently. Bureaucracy and funding to expand the focus of planned studies remain challenges. A great deal of work remains.