Despite significant evolution over the past four decades in percutaneous coronary interventions (PCI) in-stent restenosis (ISR) remains one of its major complications. The recent meta-analysis showed that ISR occurs between 1 and 5 years after PCI at an annual rate of approximately 2% [1, 2]. Although clinical evidence supporting advantage for routine intravascular imaging in PCI is still lacking it can help to differentiate between biological and various mechanical causes of restenosis [3].
An 80-year-old patient with hypertension, non-insulin dependent diabetes mellitus (DM), hyperlipidaemia and chronic kidney disease (stage G3A) after PCI of his right coronary artery (RCA) and left main bifurcation with drug-eluting stents (DES) implantation 4 years earlier was admitted with typical resting angina, left bundle branch block (LBBB) in his echocardiography (ECG) and a mildly elevated serum troponin level. Coronary angiography (CAG) revealed significant stenosis in the middle part and ostium of RCA with only mild changes in the left coronary artery (LCA) and a preserved good result of the previous PCI. The operator decided to treat both lesions in RCA. Unfortunately, due to the poor guide support related to severe angulation of the right subclavian artery and significant tortuosity and calcifications of RCA, he was only able to dilate the mid-part stenosis and implant 3.5/22 mm DES in the proximal segment.
Eight months later the patient was readmitted with symptoms of resting angina and an elevated hsTnT level. CAG showed thrombus in the ostium of RCA and mid segment occlusion with TIMI 0 flow (Figure 1). The femoral approach with 40 cm long reinforced sheath and 7F AL1.0 guide catheter were chosen. Despite using the inchworming technique, which involves immediate advancement of the guide extension catheter (GEC) over the deflated 2 mm balloon positioned halfway at the distal tip of the catheter, 6F Guideliner GEC (Teleflex) as well as IVUS Eagle Eye Platinum (Philips) were introduced only to the proximal segment of RCA showing an underexpanded stent not covering the ostium of the artery (Figure 2). The distal part of RCA was opened with 3.0 mm semi-compliant balloon and 3.5 mm NC balloon was used to open the struts of the proximal stent. Then 3.5/24 mm DES was implanted at the ostium and postdilated. Final intravascular ultrasound (IVUS) run showed an acceptable result (Figure 2).
Figure 1
A – Thrombus at the ostium of right coronary artery (RCA) (ring) and occlusion in the middle segment (arrow); B – Septal collaterals from left anterior descending artery to posterior descending artery (double arrow); C – Tip of Guideliner 6F GEC in the proximal segment of RCA (arrow); D – Final angiography with TIMI 3 flow
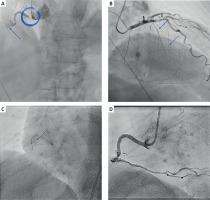
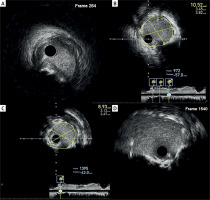
Figure 2
Intravascular ultrasound (IVUS) images before percutaneous coronary intervention (PCI): A – Severe stenosed and calcified ostium of right coronary artery (RCA) not covered by the stent; B – Proximal edge of the stent not fully expanded with heavy circular calcifications; C – Good stent expansion and apposition in the proximal segment. IVUS images after PCI; D – Ostium of RCA covered by the stent; E – Broken calcium ring around the stent at the site corresponding to image B; F – Stent protrusion to the aorta

Six weeks later, after the cessation of DAPT treatment for unknown reason, the patient was readmitted with severe retrosternal pain, hypotension, and ST elevation in II, III and aVF leads with LBBB in ECG. Urgent angiography showed ostial RCA occlusion (Figure 3). Immediate balloon angioplasty was performed and despite several thrombectomy runs the thrombus burden remained significant. Twenty-four-hour IIb/IIIa inhibitor (eptifibatide) infusion was initiated during which the patient sustained/had two short episodes of ventricular tachycardia and fibrillation. Next day control angiography showed TIMI 3 flow, full thrombus resolution and significant stenosis distal to the stent (Figure 3). Again the artery was cannulated with 7F AL1.0 guide catheter and Telescope GEC 6F (Medtronic) using the inchworming technique. The GEC reached the middle part of the artery and 3.5/38 mm DES was successfully implanted. The stent at the RCA ostium was flared with 4.5 mm NC balloon. The Opticross HD IVUS probe (Boston Scientific) with Telescope GCE support was successfully introduced showing an insignificant calcific/calcified nodule in the distal segment, good expansion of the stents with acceptable flaring at the ostium (Figure 4). One-month clinical follow-up confirmed the patient’s general good health.
Figure 3
A – Ostial occlusion of right coronary artery (RCA) with TIMI 0 flow; B – Coronary angiography (CAG) after thrombectomy with significant thrombus within previously implanted stents and TIMI 3 flow; C – Control angiography after 24-hour IIb/IIIa inhibitor infusion – significant restenosis after balloon angioplasty in the middle segment of RCA (ring); D – Tip of Opticross HD IVUS probe (Boston) in the distal segment (arrow); E – Tip of Telescope 6F GEC in the middle segment supporting drug-eluting stent (DES) implantation (arrow); F – Final angiography with TIMI 3 flow

Figure 4
Final intravascular ultrasound (IVUS) images. A – Insignificant calcific/calcified nodule distal to the stent in the middle segment of right coronary artery (RCA); B – Good expansion and apposition of the stent in the middle segment; C – Good expansion and apposition of the stent in the proximal segment; D – “Flared” stent at the ostium of RCA
We show the example of a long and difficult history of single coronary artery interventions with a spectrum of factors leading to subsequent failures. After the first procedure of poor 6F guide support through a tortuous subclavian artery, stent geographic miss and stent underexpansion in the calcified artery led to the first failure. In the second one, IVUS imaging revealed the underlying causes but again inadequate support restricted the full visualisation of the artery only to the proximal segment missing the distal restenosis. Probably, not without significance, was the ostial stent protrusion and distortion. Finally, during the last intervention, triggered by abrupt DAPT cessation, all the previous factors were considered and helped to build the strategy with a combination of 7F supportive femoral guide, modern design guide extension catheter and low-profile IVUS probe. Telescope guide extension catheter helped at many stages of the last procedure including IVUS probe engagement and distal stent implantation thanks to its unique compilation of advantages such as: solid and round pushwire maximizing the transmission of the push force, soft polymer tip with hydrophilic coating and coil design body providing flexibility and deliverability, and short 4 cm half-pipe transition zone for smooth stent accommodation (Figure 5).
Our example illustrates that awareness of medical equipment’s technical aspects and good interpretation of intracoronary imaging might be the basis of a safe and long-lasting result procedure.









