Calcified nodules (CNs) are eccentric calcified lesions protruding into the vascular lumen, and the long-term outcomes of drug-eluting stents are unfavorable [1].
To maintain patency, reducing calcification through debulking procedures is essential [1]. Rotational atherectomy (RA), the Coronary Orbital Atherectomy System (OAS) and excimer laser coronary atherectomy are commonly employed for this purpose [2]. However, these methods often prove inadequate when there is an unfavorable wire bias. This report proposes a treatment approach for CNs by presenting a case where directional coronary atherectomy (DCA) was successfully performed when conventional debulking techniques failed to achieve optimal outcomes.
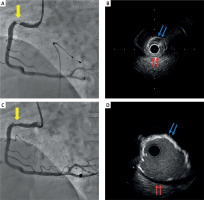
A 49-year-old male dialysis patient presenting with effort angina underwent a 1.75 mm RA procedure for CN at segment 1 (Figure 1). Subsequent intravascular ultrasound (IVUS) revealed a significant residual mass of calcification, necessitating additional ablation. However, due to strong wire bias contact with the healthy vessel wall, using a larger burr posed a high risk of vascular injury. Therefore, we decided to perform DCA. An Atherocut catheter L 6 mm (NIPRO corporation, Osaka, Japan) was delivered and expanded to 5 atm. The procedure was successfully performed and the percent plaque area improved from 80% to 52%. The intervention concluded with 4.5 mm non-compliant balloon and drug-eluting balloon (DEB) expansion, employing a non-stent strategy. At 10-month follow-up, multislice computed tomography showed no restenosis.
Figure 1
A – Coronary angiography (CAG) revealed 90% stenosis at segment 1 (yellow arrow). B – Intravascular ultrasound (IVUS) image after 1.75 mm rotational atherectomy (RA) procedure. Blue arrows indicate the edges of the calcified nodule (CN), while red arrows indicate the healthy vessel wall. The reference vessel diameter is over 4.5 mm, indicating a large vessel with a significant amount of residual CN, necessitating the use of a larger burr for debulking. However, the IVUS transducer and guide wire are in contact with the healthy vessel wall and not the calcified nodule. This implies that the burr would contact the healthy side, posing a risk of vascular injury if a large burr were used. C – CAG after directional coronary atherectomy (DCA) shows the resolution of the target lesion stenosis (yellow arrow). D – IVUS image after DCA. Since DCA allows for the intentional determination of the cutting site without being influenced by wire bias, it avoids injuring the healthy side (red arrows) and selectively debulks the CN (blue arrows)
Wire bias, which denotes the contact location between the guide wire and the vessel wall, is a significant predictor of vascular injury as it predicts the contact between the burr or crown and the vessel wall. The location ablated by RA or OAS is determined by wire bias and cannot be controlled intentionally. This often leads to suboptimal debulking in CN cases, resulting in difficulties with balloon expansion and stent under-expansion. Conversely, DCA allows for intentional determination of the cutting site by directing the cutter towards the target plaque identified via IVUS. This method allows for the reduction of the target plaque while avoiding healthy vessel walls, making DCA a highly advantageous treatment strategy for CN.
DCA is typically used for bifurcation lesions involving non-calcified plaques, and its utility for calcified lesions is not well known. However, studies have shown that DCA can effectively excise calcified plaques in vitro [3]. DCA was revived in 2014 following improvements in catheter technology and the emergence of DEB and is currently an atherectomy device available exclusively in Japan. However, accumulating evidence on its long-term outcomes and safety suggests that its use may expand to other regions in the future. As demonstrated in this case, DCA offers a viable treatment strategy for CNs where RA and OAS fail to achieve effective debulking, potentially leading to improved long-term outcomes. Percutaneous coronary intervention for CNs remains a developing field, and various strategies are required to achieve better long-term results. As illustrated in this case, combining DCA with RA or OAS for CNs that do not respond adequately to conventional methods can yield favorable outcomes and promising long-term results.








