Introduction
Colorectal surgery is a viable treatment option for various lower digestive system conditions, including but not limited to haemorrhoids, diverticulitis, and cancer [1]. The utilization of minimally invasive procedures, including laparoscopic and robotic interventions, is on the rise. The typical duration of hospitalization subsequent to colorectal surgery ranges from 6 to 11 days, while the incidence of complications is estimated to be between 15% and 20% according to sources [2, 3]. In 2001, a group of surgeons and anaesthesiologists, led by Kehlet, introduced the Enhanced Recovery After Surgery (ERAS) protocol, also referred to as the fast-track surgery program, as a possibility to change the perioperative care and have a substantial impact on treatment outcomes [4]. ERAS is a consensus protocol that is evidence based and multimodal. It comprises various elements of perioperative care pathways, and its primary objectives are to optimize body functioning, decrease the surgical stress response, and accelerate postoperative recovery in patients undergoing major surgical procedures [5, 6].
Since 2010, the ERAS group has established global colorectal surgery perioperative care standards. Preoperative counselling, perioperative hydration, anaesthetic and analgesic regimens, nutritional care, and complication avoidance are prioritized in the ERAS colorectal surgery recommendations [7–9]. Several studies and trials have demonstrated that the implementation of the ERAS protocol results in enhanced outcomes such as reduced length of hospital stay, improved gastrointestinal function, increased mobility, decreased postoperative complications, and lower readmission rates, when compared to standard care [10–13]. Nevertheless, certain investigations have reported no discernible distinction between the ERAS and conventional protocols [14, 15]. A meta-analysis was carried out on recent and reliable trials [16–27] to evaluate the effectiveness and safety of the Enhanced Recovery After Surgery (ERAS) program in patients who have undergone colorectal surgery.
Aim
The objective of this meta-analysis was to assess the effectiveness and safety of the ERAS program in patients undergoing colorectal surgery using randomized controlled trials published between 2010 and 2023.
Material and methods
The present study adhered to the normative recommendations of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines [28].
Search strategy
In accordance with PRISMA guidelines, a systematic and thorough investigation of randomized controlled trials (RCTs) was conducted on the databases of PubMed and the Cochrane Library. The search query utilized the keywords “Enhanced Recovery After Surgery” (ERAS) and “Fast Track Surgery” (FTS) in conjunction with “Colorectal Surgery”, “Rectal Surgery”, and “Colorectal Cancer Surgery”. The search methodology employed a meta-analysis approach. A comprehensive review of academic literature was carried out by utilizing the databases of the PubMed and Cochrane libraries. The search strategy involved the utilization of the Boolean operator “AND” to merge the medical subject headings (MeSH) and text keywords. Furthermore, a manual search of the bibliographies was carried out by 2 researchers (LYN and LQP) in an independent manner to identify noteworthy papers. A systematic screening process was employed to select all RCTs that were published within the timeframe of 2010 to 2023.
Inclusion and exclusion criteria
The present investigation integrated relevant scholarly works published from 2010 to 2023, which delineate comparative results among patients undergoing colorectal surgery utilizing the ERAS protocol versus those receiving customary care. The study incorporated full-text articles and only included abstracts in the meta-analysis if they contained sufficient information. Studies that lacked adequate data, were not related to colorectal surgery, or were published before 2010 were excluded. Two authors (WZ and FW) conducted an independent review of the relevant literature to identify pertinent studies. The utilization of inclusion criteria was employed to exclude obsolete references and include studies of significant relevance.
Evaluation of the analytical variables
The demographic summary and event data were independently collected from the included studies by 2 researchers, identified as SQ and ZL. The study’s main measures of success included: (1) the duration until the first occurrence of flatus; (2) the overall length of hospitalization; (3) the length of hospitalization after surgery; (4) the frequency of readmissions; (5) the total count of complications that occurred after surgery; and (6) the total count of infections that occurred at the surgical site.
Sources of heterogeneity
Two reviewers (WZ and FW) conducted an independent assessment of the methodological validity of the studies included and computed the heterogeneity in the experiments that were included. The author SZ was assigned with resolving any potential conflicts that may have emerged between the authors WZ and FW. The examination of heterogeneity was carried out by employing the Cochran Q statistic and I2 index in a random bivariate mode, with the aid of the RevMan software [29]. The study investigated various sources of heterogeneity, such as the utilization of full-text publications versus abstracts, differences in age groups and sample sizes, diverse types of surgical parameters evaluated, and varying study outcomes.
Risk of bias assessment
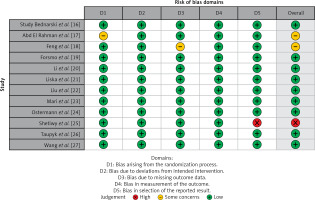
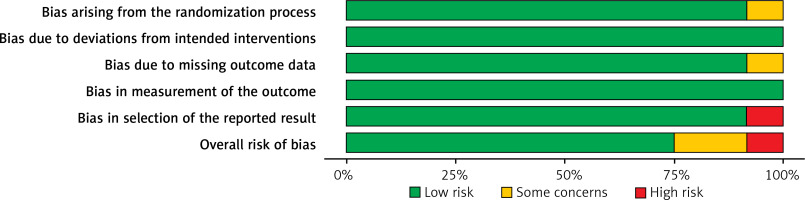
The evaluation of potential bias in the studies that were incorporated was carried out using a predetermined questionnaire. The researchers employed the Cochrane Risk of Bias: Robvis tool [30] to generate a summary and graph of the risk of bias.
Meta-analysis
The meta-analysis was conducted using RevMan software (Version 5, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020). The group of individuals demonstrating a level of variability surpassing 50% chose to utilize the random effect, whereas the subgroup with a heterogeneity level below 50% employed the fixed effect. The Mantel-Haenszel technique with random bivariate effects was predominantly utilized in this investigation to compute statistical parameters such as standard deviation and odds ratio, accompanied by a 95% confidence interval [31]. Additionally, corresponding forest plots were created. The statistical measures of τ2, χ2, I2, and z were employed to assess the degree of heterogeneity present in the studies that were incorporated in the analysis. A significance level of 0.05 was used to determine statistical significance based on the p-value. The diagnostic odds ratio was determined through employment of the DerSimonian Lair approach, utilizing a 2 × 2 table, as reported in reference [32]. To evaluate the publication bias of the studies included in the analysis, Begg’s test [33], Egger’s test [34], and Deek’s funnel plot [35] were employed. The log odds ratio of each study was plotted against its standard error using MedCalc software [36] for the production of the Deek’s funnel plot.
Statement of ethics
All procedures performed in the study were in accordance with the institutional and/or national research committee’s standards of Medical Ethics Committee of Affiliated Hospital of Hebei University of Engineering; adopted on June 18,2019; batch No. 2019 [K] 023 and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Results
Literature search results
Figure 1 shows how the PRISMA chart selected the research studies. By examining the digital databases, 487 research studies were found. After removing duplicate entries, 314 papers were screened by abstract and title. Text analysis was performed on 142 eligible papers. Twelve papers satisfied the inclusion and exclusion criteria for the current meta-analysis. This study examined the efficacy and safety of the ERAS protocol in colorectal surgery. Only randomized controlled trials were analysed. Table I presents a comprehensive overview of the pertinent characteristics of the scrutinized studies, encompassing the identification number, publication year, research design, overall sample size, number of participants in the ERAS and control cohorts, age distribution of patients in both groups, gender ratio, and primary outcome measures.
Table I
Characteristics of the included studies
| Study ID | Publication year | Journal of publication | Type of study | Total participants | Age of participants | Gender (M/F) | Number of participants in ERAS group | Number of participants in Control group | Primary outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|
| ERAS group | Control Group | |||||||||
| Bednarski et al. [16] | 2019 | The British Journal of Surgery | Randomized controlled study | 30 | 58.7 ±12.6 | 59.3 ±10.2 | 16/14 | 14 | 16 | Total length of hospital stay, readmission rate, post-operative complications |
| Abd El Rahman et al. [17] | 2020 | Indian Journal of Surgical oncology | Randomized controlled study | 80 | 49.5 ±10.4 | 49.7 ±8.4 | 40/40 | 40 | 40 | Total length of hospital stay, post-operative complications, total number of surgical site infections |
| Feng et al. [18] | 2016 | International Journal of Colorectal disease | Randomized controlled study | 230 | 58.12 ±11.04 | 58.31 ±10.89 | 129/101 | 116 | 114 | Post-operative length of stay, time to first flatus, post-operative complications, post-operative length of stay, total number of surgical site infections |
| Forsmo et al. [19] | 2016 | Colorectal disease | Randomized controlled study | 307 | 64.24 ±12.46 | 65.15 ±13.98 | 165/142 | 154 | 153 | Total length of stay, time to first flatus, readmission rate, post-operative complications, total number of surgical site infections, post-operative length of stay |
| Li et al. [20] | 2019 | BMC Cancer | Randomized controlled study | 342 | 59.8 ±10.09 | 61.3 ±11.21 | 213/130 | 172 | 170 | Total length of stay, time to first flatus, readmission rate, post-operative complications, total number of surgical site infections, post-operative length of stay |
| Liu et al. [22] | 2017 | Saudi Journal of Biological sciences | Randomized controlled study | 156 | 52.4 ±12.6 | 52.4 ±12.6 | 87/69 | 86 | 70 | Post-operative length of stay, time to first flatus, post-operative complications |
| Liska et al. [21] | 2021 | Annals of surgery | Randomized controlled study | 135 | 54.87 ±11.64 | 55.38. ±10.89 | 357/357 | 135 | 269 | Total length of stay, readmission rate, post-operative complications, total number of surgical site infections |
| Mari et al. [23] | 2016 | Surgical laparoscopy, endoscopy and percutaneous techniques | Randomized controlled study | 140 | 63.78 ±8.65 | 66.43 ±10.12 | 74/66 | 70 | 70 | Post-operative length of stay, time to first flatus, readmission rate, post-operative complications, total number of surgical site infections |
| Ostermann et al. [24] | 2019 | Disease of the colon and rectum | Randomized controlled study | 150 | 80.06 ±4.38 | 78.27 ±4.17 | 61/89 | 75 | 75 | Total length of stay, readmission rate, post-operative complications, total number of surgical site infections |
| Shetiwy et al. [25] | 2017 | Annals of Coloproctology | Randomized controlled study | 70 | 48.54 ±12.29 | 53.63 ±11.5 | 45/25 | 35 | 35 | Total length of stay, readmission rate, post-operative complications, total number of surgical site infections, post-operative length of stay |
| Taupyk et al. [26] | 2015 | Oncology Letters | Randomized controlled study | 70 | 58.5 ±8.4 | 57.4 ±10.1 | 42/28 | 31 | 39 | Total length of stay, time to first flatus, readmission rate, post-operative complications, post-operative length of stay, total number of surgical site infections |
| Wang et al. [27] | 2011 | Colorectal disease | Randomized controlled study | 210 | 72.41 ±12.30 | 73.06 ±13.09 | 42/36 | 106 | 104 | Post-operative length of stay, time to first flatus, total length of stay, post-operative complications, post-operative length of stay, total number of surgical site infections |
Quality assessment of the included studies
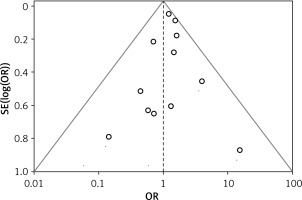
Table II shows the study quality ratings. Figure 2 summarizes the partiality risk, whereas Figure 3 visually depicts it. Nine of the 12 studies had low bias. Two studies had a moderate risk of bias due to randomization issues and inadequate outcome data. The study’s outcome selection was deemed biased. Figure 4 suggests a low probability of publication bias. Begg’s test (p = 0.374) and Egger’s test (p = 0.254) yielded non-significant p-values (p > 0.05) [37].
Table II
Risk assessment of included studies
| Study ID and year | Bednarski et al. [16] | Abd El Rahman et al. [17] | Feng et al. [18] | Forsmo et al. [19] | Li et al. [20] | Liska et al. [21] | Liu et al. [22] | Mari et al. [23] | Ostermann et al. [24] | Shetiwy et al. [25] | Taupyk et al. [26] | Wang et al. [27] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Did the study avoid inappropriate exclusions? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Did all patients receive the same reference standard? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were all patients included in the analysis? | N | N | N | N | N | N | N | N | N | N | N | N |
| Was the sample frame appropriate to address the target population? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were study participants sampled in an appropriate way? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were the study subjects and the setting described in detail? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Were valid methods used for the identification of the condition? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the condition measured in a standard, reliable way for all participants? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
Efficacy outcomes
The present study conducted a meta-analysis of 12 randomized controlled trials, involving a combined sample size of 1920 participants. Out of the total sample population, ERAS care was administered to 880 individuals, whereas conventional care was provided to 1002 individuals. The present study conducted a statistical analysis of the primary outcomes of the included studies to assess the safety and efficacy of ERAS for colorectal surgery.
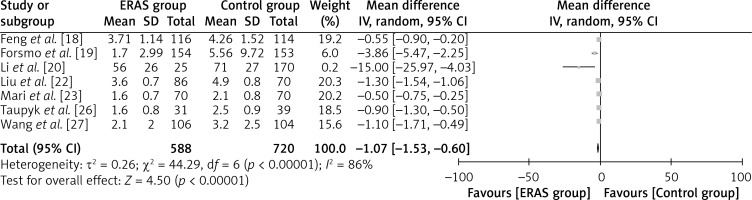
Time to first flatus
Figure 5 shows that 7 studies recorded the parameter in 588 ERAS patients and 720 standard-treatment patients. The study found that ERAS patients resumed flatus faster than typical-treatment patients. The results indicate a statistically significant difference, as demonstrated by a WMD of –1.07 days and a 95% confidence interval of –1.53 to –0.60, with a p-value of less than 0.00001. A random-effects model was utilized owing to the significant heterogeneity observed (I2 = 86%).
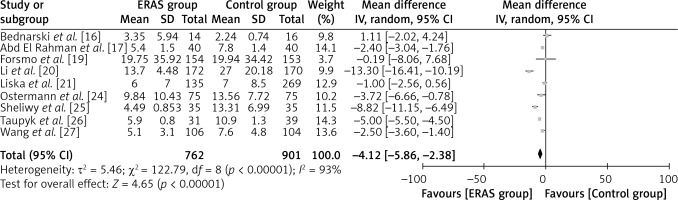
Total length of hospital stay
Nine studies have documented this statistic, including 762 patients in the ERAS group and 901 in the usual treatment group (Figure 6). The study found that ERAS patients had a shorter hospital stay than traditional care patients. This is supported by a weighted mean difference (WMD) of –4.12 days (95% CI: –5.86 to –2.38, p < 0.00001). A random-effects model was utilized as a result of significant heterogeneity, with an I2 value of 93%.
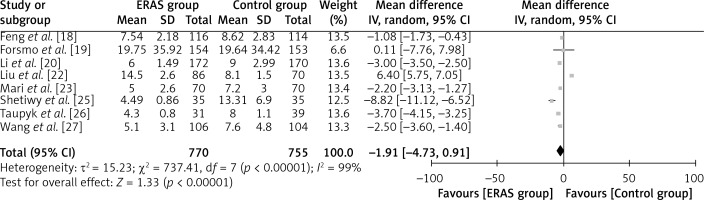
Length of post-operative hospital stay
Figure 7 shows the findings of 8 investigations with 770 ERAS patients and 755 standard care patients for this parameter. The study found that ERAS patients had shorter post-operative hospital stays than traditional patients. This was supported by a WMD of –1.91 days (95% CI: –4.71 to 0.91, p < 0.00001). A random-effects model was utilized as a result of significant heterogeneity (I2 = 99%).
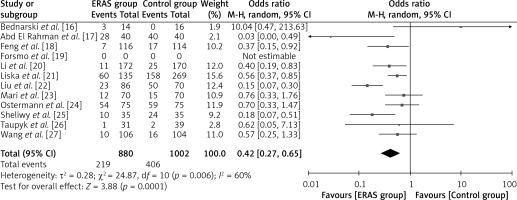
Total number of post-operative complications
Figure 8 shows this effect from 12 trials with 880 ERAS patients and 1002 standard-care patients. The study found that ERAS patients had fewer post-operative problems than conventional patients. This is supported by the odds ratio (OR) of 0.42 (95% CI: 0.27 to 0.65, p = 0.0001). The utilization of a random-effects model was necessitated by significant heterogeneity, as indicated by an I2 value of 60%.
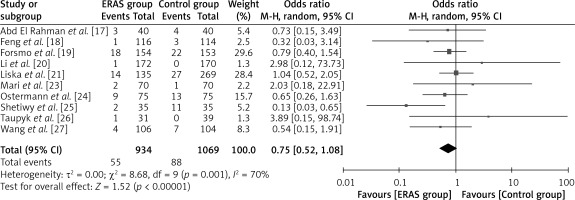
Total number of surgical site infections
Figure 9 shows the results of 10 investigations with 934 ERAS patients and 1069 standard-care patients. The study found that ERAS patients had fewer surgical site infections than conventional patients. This was supported by the OR of 0.75 (95% CI: 0.52 to 1.08, p < 0.00001). In light of the significant heterogeneity (I2 = 70%), a random-effects model was utilized.
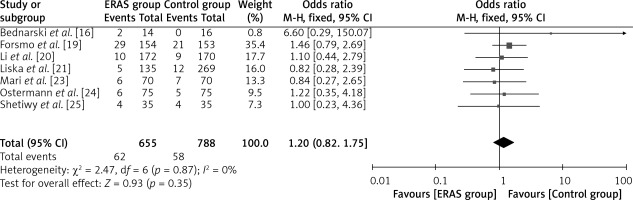
Readmission rate
Figure 10 displays the results of 8 studies, which included a total of 655 patients in the ERAS group and 788 patients in the traditional care group, with respect to this particular outcome. The fixed-effects model was utilized considering the low heterogeneity value of I2 = 0%. The findings indicate that the ERAS group patients had a lower rate of readmission compared to those in the control group, as demonstrated by the OR of 1.20 (95% CI: 0.82 to 1.75, p = 0.35).
Discussion
General anaesthesia is used for difficult colorectal surgery. The surgeon may use laparoscopic or open approaches to perform these treatments [38, 39]. Both options need hospitalization for many days [40]. Before starting therapy, the patient must undergo several diagnostic tests and imaging modalities and receive many pharmaceutical medications [41].
Postoperative complications may arise after any surgical procedure, including colorectal surgeries. These complications may include anastomotic leakage, impaired gastrointestinal motility, thromboembolic events, and haemorrhage. The ERAS approach was developed to address the aforementioned complications. ERAS is an interdisciplinary and collaborative strategy that aims to reduce the physiological stress response to surgical procedures and expedite the recovery of organ function. The study revealed that the adoption of the ERAS protocol was associated with a decrease in the occurrence of general complications and a shorter hospital stay, without any increased risks of readmission, reoperation, or mortality in patients undergoing emergency colorectal surgery [42, 43].
Several meta-analyses [44–46] have compared ERAS to traditional treatment in colorectal surgery patients to assess its advantages. ERAS protocols reduce postoperative complications and speed colorectal surgical recovery, according to a literature review. Primary hospital visits and hospitalization lengths also decrease. However, ERAS guidelines do not appear to reduce hospital readmissions or deaths. ERAS methods have been limited in their adoption due to a lack of confidence or expertise [47, 48] because some medical professionals oppose early feeding, catheter removal, and mobility. Several meta-analytic studies have examined ERAS specifically in laparoscopic colorectal surgery patients [49] or included both randomized and non-randomized trials [50].
The present study was conducted to investigate and resolve the aforementioned inconsistencies. The present study is of a comprehensive nature because it includes patients who have undergone diverse surgical procedures. Our approach is impartial with regards to any specific surgical technique, and we give priority to the incorporation of high-quality research by strictly following randomization as a screening standard.
The present meta-analysis investigated several key primary outcomes, such as the duration until the first occurrence of flatus, the overall length of hospital stays, the total length of post-operative hospital stays, the aggregate number of post-operative complications, the cumulative number of surgical site infections, and the rate of readmission. The present study conducted a meta-analysis of 12 randomized clinical trials involving a total of 1920 participants. The analysis revealed significant heterogeneity among the included studies, indicating variations in the observed outcomes. Additionally, the risk of bias was found to be low, suggesting that the included trials were conducted with minimal potential for systematic errors. The statistical tests employed to assess publication bias, namely Begg’s test (p = 0.374) and Egger’s test (p = 0.254), yielded insignificant results, indicating no evidence of publication bias in the analysed studies. Our study revealed that patients who underwent ERAS treatment experienced a faster recovery of flatus compared to those who received conventional treatment. The difference in mean recovery time was statistically significant, with a WMD of –1.07 days. Additionally, ERAS patients had shorter overall hospital stays, with a WMD of –4.12 days, as well as shorter post-operative hospital stays, with a WMD of –1.91 days. The study revealed that the ERAS group exhibited a reduced incidence of post-operative complications, as indicated by an odds ratio of 0.42. Additionally, a lower occurrence of surgical site infections was observed in the ERAS group, with an odds ratio of 0.75. Furthermore, the ERAS group demonstrated a relatively low rate of readmission, as reflected by an odds ratio of 1.20.
The study’s outcomes demonstrate that the adoption of the ERAS protocol results in a decrease in the duration of the first flatus, hospitalization, and post-operative complications in comparison to the time required for the first fluid intake and solid diet tolerance, as indicated by the statistically significant results (p < 0.05). Furthermore, it has been determined that the ERAS protocol is associated with a reduction in hospitalization duration, post-operative hospitalization, readmission rates, and incidence of complications. The traditional method of providing care, however, fails to produce a statistically significant effect on the frequency of hospital readmissions.
The results of our investigation have indicated a noteworthy statistical advantage in favour of the ERAS protocol. Our study reveals that the implementation of enhanced-recovery protocols in colorectal surgery demonstrates both feasibility and favourable outcomes. Specifically, these protocols are linked to a reduced length of hospital stay, expedited recovery of physiological function, and no significant increase in complication or readmission rates.
This meta-analysis is subject to various limitations. Despite the study’s adherence to rigorous methodology, the findings are constrained by the restricted number of 12 randomized controlled trials (RCTs) exhibiting moderate to high levels of heterogeneity. Subsequently, a number of the results that were analysed were not present in the majority of RCTs. A significant proportion of randomized controlled trials exhibited inadequate concealment of surgeons and participants, as well as insufficient masking. Thirdly, the outcomes of the study were influenced to some extent by the impact of diverse populations and varying reported results. Finally, the omission of articles written in languages other than English may have impeded our meta-analysis.
Conclusions
The results of our meta-analysis suggest that the ERAS care cohort demonstrated a statistically significant decrease in the duration of time until the first flatus, a reduction in the length of hospitalization, an accelerated recovery of typical gastrointestinal function, and a decreased occurrence of post-operative complications and surgical site infections, relative to the conventional care cohort. The study found that there was no statistically significant difference in the readmission rates between the 2 cohorts. The results of our study suggest that the implementation of the ERAS protocol is a viable and secure approach for reinstating normal bodily processes in patients who have undergone colorectal surgery. In their prospective cohort study, Gumusoglu et al. (2022) investigated the significance of inflammatory markers in identifying complications among patients with gastric cancer, who were subjected to the ERAS protocol [51]. The authors found that IL-1, TNF, CRP, and PCT could serve as valuable indicators for early detection of major complications in gastric cancer patients undergoing the ERAS protocol, thereby further augmenting the potential benefits of this protocol.