Introduction
Body dysmorphic disorder (BDD), or dysmorphophobia, is a disabling mental condition with a distressing or impairing preoccupation with slight or imagined defects in appearance, resulting in painful, repetitive behaviours (e.g., mirror checking) or mental acts (e.g., comparing own appearance to others) [1]. The Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) defines BDD as an excessive concern about a perceived appearance defect, associated with meaningful discomfort and deterioration of everyday life functioning [2]. According to World Health Organization’s International Classification of Diseases-11 (ICD-11) BDD is ‘preoccupation with appearance or self-image causing significant distress or impairment in important areas of functioning’ or ‘preoccupation with a slight or imagined defect in appearance that causes significant distress or impairment in social, occupational, or other areas of functioning’ or ‘compare body image disturbances’ [3].
Although BDD is comparatively common (the prevalence of BDD in general population is assessed as 1.9%), worldwide prevalent and results in everyday functioning impairment, high levels of distress, and a risk of suicide, the diagnosis is disturbingly, frequently missed [1, 4]. This may be a result of a limited number of screening instruments for BDD (most commonly the scales proposed by Phillips et al. [5, 6] in mid '90s), unacquaintance of available diagnostic tools among medical personnel or lack of potentiality to measure severity of BDD or treatment outcomes [7]. Appearance Anxiety Inventory (AAI) is an instrument developed by Veale et al. in 2014 not only to assess the severity of BDD symptoms, but also as a process measure during any therapy [7].
Aim
Originally AAI was created in English. As there is no Polish version available, this study was created to translate and validate the questionnaire. This will enable the use of AAI in further research or clinical practice in subjects speaking Polish.
Material and methods
The translation and validation process of the Polish version of the AAI questionnaire was conducted according to international standards. The permission to translate the questionnaire was acquired from the copyright holders. The AAI was primarily developed as a measure used to identify the cognitive processes and behaviours that might mediate the outcome of any therapy in people with Body Dysmorphic Disorder (BDD). It can be used to assess the progress of patients throughout the therapy. The scale encompasses 10 items. Each item is scored on a 5-point Likert scale ranging from 0 for “not at all” to 4 for “all the time”. The maximum score is 40, and higher scores reflect greater frequency of a process. The total score is obtained by summing all the items. Individuals who score 14–15 or more are likely to have a diagnosis of BDD, but the questionnaire should be used rather to assess severity of symptoms than to screen for BDD [7].
Translation and validation process
At first, the original English version of the AAI questionnaire was translated into Polish language by two independent translators. Then, the translated versions were compared in terms of incompatibility by a third bilingual expert and a unified, third version was created. Next, another independent translator, who was not acquainted with the original version of the AAI questionnaire, carried out reverse translation from Polish to English. The author of the original English version of AAI recommended minor changes after checking reversed translation. The required corrections were implemented accordingly. Finally, the Polish version of COPS questionnaire was obtained.
After the translation process, the validation was performed. The questionnaire was tested on a group of 49 individuals to assess the level of translation consistency and reproducibility. The group of subjects was recruited from individuals who reported to the dermatology clinic. The questionnaire was completed by 28 females and 21 males aged 26–55 years. In order to determine test-retest reliability, the responders were asked to complete the questionnaire twice with a 3–6 days’ interval, which is considered sufficiently long to prevent the individuals from remembering previous answers.
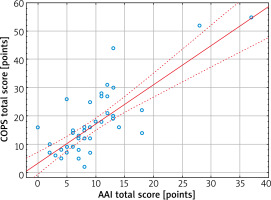
To conduct convergent validity, the subjects were also asked to fill the Polish versions of COPS (Cosmetic Procedure Screening Questionnaire – also used in the original validation paper) [8, 9] and RSES (Rosenberg Self Esteem Scale) [10]. The COPS questionnaire evaluates the features unattractive for the subjects with regard to diagnostic criteria of BDD. The questionnaire encompasses 9 items which are scored from 0 points (least impaired) to 8 points (most impaired), range 0–72 points. The score is a sum of questions 2 to 10. Items 2, 3 and 5 are reversed. The higher score indicates greater impairment. Individuals who score 40 or more are likely to have a diagnosis of BDD [8, 9].
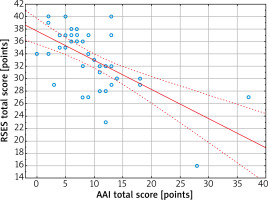
The RSES [10] is one of the most recognized and widely used measures of self-esteem. It comprises 10 items, on a 4-point Likert scale each (strongly agree, agree, disagree, and strongly disagree). Items 1, 2, 4, 6 and 7 are reversed – with a positive impact. Total possible scores range from 10 to 40; the higher scores indicate the higher level of self-esteem.
Statistical analysis
The statistical analysis of the acquired results was performed with the use of Statistica 13 (Dell, Inc., Tulsa, USA) software. The internal consistency of the questionnaire was evaluated with Cronbach α coefficient, which value of at least 0.7 indicates for sufficient questionnaire internal consistency, while the value above 0.9 stands for very good internal consistency [11]. Intraclass correlation coefficient (ICC) was used to assess the questionnaire reproducibility (test-retest reliability). Adequate reproducibility of the questionnaire is recognized if ICC is at least 0.7 [12]. The correlation between the answers from a single completion to each question and to the total score was obtained with Spearman correlation test. The same test was used to measure the dependences between AAI and other instruments (i.e. COPS and RSES) used for convergent validity. Furthermore, responses to each question from the first and second completion were compared with Wilcoxon test in a search for important differences, with p-value ≤ 0.05 considered as statistically significant.
Results
The estimation of internal consistency of the Polish language version of AAI demonstrated that the different items of the questionnaire are interrelated. Cronbach α coefficient value for the questionnaire was assessed as 0.91, which indicated very good internal consistency for the translated version of the instrument. Highly significant correlations (p < 0.01) were found between the results obtained for each item and the total score of the questionnaire (Table 1). The reproducibility of the analysed questionnaire was determined using ICC and assessed as 0.78 for the whole AAI. Moreover, no statistically significant differences were found for each particular question of AAI and AAI total scores between the first and second completion (on day 0 and day 3–6) (Table 2). A highly statistically significant, strong positive correlation (r = 0.67, p < 0.0001) were found between the results obtained for total score when filling out the questionnaire twice. Similarly, moderate-to-strong correlations were also found for each particular question (p < 0.05) (detailed data not shown). AAI correlated strongly with COPS (r = 0.67, p < 0.0001), indicating that higher scores on AAI were associated with higher possibility of BDD (Figure 1), and revealed a strong negative correlation with RSES (r = –0.57, p < 0.0001), which indicated that the higher the appearance anxiety, the lower the self-esteem is (Figure 2).
Table 1
Correlation of each item (Q) score with a total score of AAI
Table 2
Reproducibility of results of AAI
The results presented above proved satisfactory convergent validity, consistency and reproducibility of the translated version of the questionnaire. The individuals reported good intelligibility of the questions and completing of the questionnaire took 3–5 min. The Polish version of AAI is available on request from the corresponding author.
Discussion
Body dysmorphic disorder is characterized by preoccupation with thinking and behaviours related to appearance concerns. It is a disabling mental health disorder where a perceived defect in physical outlook impairs everyday life functioning [1, 7, 13, 14]. As mentioned above, although BDD is associated with a very negative impact on quality of life (severe suffering, constant intrusive thoughts, shame, depression, social distancing) and it is a rather common mental disease, prevalent around the world, the diagnosis is often missed [7]. Because there is a limited number of instruments screening for BDD and measuring its severity, especially available in the Polish language, we decided to conduct the validation process on the one with high evaluating potential (in our opinion) – Appearance Anxiety Inventory (AAI). The scale is brief, sensitive to change, and suitable for weekly assessment during treatment. AAI may be used to assist clinicians to choose the best therapeutic option [7].
This study describes the detailed and adequate process of development and validation of the Polish language version of the AAI questionnaire. Comparing to the original version of the AAI questionnaire, the translated Polish language version showed similar, good test-retest reliability (ICC = 0.87 vs. ICC = 0.78, respectively) and an identical value of Cronbach α coefficient (0.91) [7]. Moreover, convergent validity of AAI and COPS (as used in the original paper) revealed identical results, showing a significant relationship of body image and psychological distress (i.e. r = 0.67) [7].
The main limitations were that the AAI was validated in a population that did not have BDD and the results may be different in a clinical population.
It is very important to improve recognition of BDD which could be achieved by increasing awareness of this disease among medical professionals. Understanding the nature and symptoms of BDD especially by non-psychiatric medical specialists and rising availability of diagnostic tools could lead to more accurate diagnoses. The psychometric assessment of each patient could play a significant role in choosing the appropriate approach. It is important to implement psychological evaluation in non-psychiatric clinics and familiarize medical environment with proper diagnostic and evaluating instruments.