Introduction
Short-term mortality is a complication associated with acute-on-chronic liver failure (ACLF) [1]. It has been suggested that the liver in ACLF patients exhibits partial reversibility, which is not seen in decompensated cirrhosis [2]. As hepatocytes can regenerate quickly, they require inorganic phosphate to meet their needs for producing adenosine tri-phosphate (ATP). An increase in ATP production leads to a requirement for inorganic phosphate, which results in the influx of phosphate into the liver from the bloodstream. Consequently, before even bone phosphate mobilization takes place, a sizable amount of blood phosphate supports the metabolic demands of regenerating hepatocytes [3]. At first, it causes transient lower serum phosphate levels. As a result, early hypophosphataemia may be used to identify a subset of ACLF patients who will still have enough functional liver mass to support liver regeneration and aid in the prediction of spontaneous recovery. The impact of hypo- or hyperphosphataemia on ACLF prognostication has been rarely studied to date. By comparing it with well-accepted prognostic scores, the current study aims to gain insight into the role of serum phosphate in predicting short-term mortality in patients with ACLF [4].
Material and methods
Patients
Patients with ACLF receiving care at the Department of Medical Gastroenterology, Lokmanya Tilak Municipal Medical College, and LTMG Hospital, Sion, Mumbai, between June 2021 and December 2022 were included in this single-centre prospective observational study.
Inclusion criteria: In accordance with the definition of the Asia Pacific Association for Study of Liver Disease (APASL) criteria [1], patients with an established diagnosis of ACLF with ages ranging from 18 to 80 years and either gender were included.
Exclusion criteria: Failure to provide informed consent, hypo- or hyperparathyroidism, hypervitaminosis D, individuals with HIV, pregnant women and nursing mothers, chronic kidney illness, and any kind of malignancies.
Assessment and outcome parameters
Demographic data, mode of presentation, personal history, results of physical examination, laboratory investigations: complete blood count (CBC), liver function (bilirubin, alanine aminotransferase [ALT], aspartate aminotransferase [AST], alkaline phosphatase [ALP], total protein and albumin), coagulation profile (international normalized ratio [INR]), renal functions tests (creatinine, blood urea nitrogen), serum phosphate, serum arterial lactate.
Serum phosphate was measured by the colorimetric method. The principle is that phosphorus reacts with molybdic acid to form phosphomolybdic acid in an acidic medium which further is reduced to molybdenum blue and absorbs light at 340 nanometres (nm) which is directly proportional to phosphate concentration in the sample. The normal range is 2.5-4.5 mg/dl. Serum arterial lactate was measured by the spectrophotometric method with a normal range of 0.5-1.6 mmol/l. Causes of liver disease aetiology were decided according to proper history taking and blood markers. Chronic liver disease was detected with hepato-porto-splenic Doppler, FibroScan as well a computed tomography (CT) abdominal scan and the presence of varices on oesophagogastroscopy. Alcohol-related liver cirrhosis was recorded if alcohol intake in males was more than 60-80 g/day and in females if it was more than 20-40 g/day for more than 10 years. Alcoholic hepatitis was defined as “onset of jaundice within 60 days of heavy alcohol consumption (> 60 g/day for males, > 40 g/day for females) for a minimum of 6 months associated with serum bilirubin more than 3 mg/dl, raised AST, serum AST: ALT more than 1.5 and no other obvious cause of hepatitis”. Hepatitis B and C were diagnosed by the ELISA method. Wherever necessary, acute hepatic insults such as hepatitis A, and E were diagnosed by the serum IgM HAV, HEV ELISA method. Suspected acute flares of hepatitis B were ruled out by HBV DNA quantitative titres by the PCR method. Drug-induced liver injury was suspected by proper history-taking. Autoimmune liver disease was detected by serum anti-neutrophilic antibody (ANA), anti-smooth muscle antibody (ASMA), serum total immunoglobulin G level (IgG total), and anti-liver-kidney microsomal antibody (anti-LKM). Wilson’s disease was investigated by serum ceruloplasmin levels by the copper oxidase method, 24-hour urinary copper levels, and slit-lamp examination for Kayser-Fleisher (KF) rings. A liver biopsy was done by the transjugular route due to the presence of ascites. Infections as a cause of acute insult for deterioration were ruled out by ascitic fluid studies to look for spontaneous bacterial peritonitis (microscopy, biochemistry, cultures), three separate blood cultures, other blood investigations such as the Rapid Malaria antigen detection test, Rapid Leptospirosis IgM test, and Rapid Dengue NS1 Antigen test. COVID antigen testing was also done as a rule for all patients in our study.
ACLF grading into I, II, and III was defined based on the APASL 2019 definition and AARC-ACLF scores, namely AARC-ACLF scores 5-7 as grade I, 8-10 as grade II and 11-15 as grade III. Hepatic encephalopathy was diagnosed and graded by the West-Haven classification; the grade of ascites was determined by ultrasonography and palpation of the abdomen as grade 1, 2 and 3 according to the International Ascites Club.
Patients with ascites were started on diuretics after ruling out contraindications. Anti-encephalopathy measures (lactulose, rifaximin) were taken in patients with hepatic encephalopathy. Appropriate intravenous antibiotics were started and modified according to blood and ascitic fluid culture sensitivity reports. Nutritional support with a high protein and calorie diet was given during the ward stay. Pentoxifylline tablets were given for alcoholic hepatitis without acute kidney injury (AKI). Alcohol abstinence and withdrawal symptoms were managed with a deaddiction specialist. Entecavir was started in patients with hepatitis B flare. Very ill patients were managed with ICU care. Evaluation was done throughout the hospitalization and post-discharge through phone consultations and/or follow-up visits at the liver clinic. Patients were given the option of liver transplantation (LT) at onset. None of the patients opted for liver transplantation due to logistic and financial constraints.
Prognostication scores such as the Chronic Liver Failure Consortium-Sequential Organ Failure Assessment (CLIF-SOFA) score [5], Chronic Liver Failure Consortium (CLIF-C) score [6], Child-Turcotte Pugh (CTP) score [7], Model for End-stage Liver Disease (MELD) [8], Model for End-stage Liver Disease-Sodium (MELD-Na) [9] and APASL-ACLF Research Consortium-Asia Pacific Association for Study of Liver Disease (AARC-ACLF) score [10] were calculated as per standard equations.
The primary endpoint was to assess short-term mortality (up to day 28) in patients with ACLF by utilizing serum phosphate levels. The secondary endpoint was to establish the threshold value of serum phosphate and compare it with established and validated scoring systems in short-term mortality prediction among ACLF patients.
Statistical analysis
Data were entered into Microsoft Excel 2013 utilizing a semi-structured questionnaire set that was used in previous literature. Charts, graphs, and percentages are used to display qualitative data. Quantitative variables’ mean and standard deviation are displayed. For analysis, appropriate statistical tests were run using SPSS software version 21.0. An unpaired t-test was performed to compare the study variables, and a chi-square test was utilized to determine whether there was any correlation. According to the needs of the investigation, ROC (receiver operating characteristics) curves and correlation were used to evaluate various study factors and deaths in ACLF cases. The p-value < 0.05 was considered statistically significant.
Ethical approval
The institutional ethics committee approved the study according to ICH-GCP, New Clinical Trial guidelines (IEC/168/22). Informed written consent was taken from all patients before enrolment in the study, or if there was any indication that the patient’s sensorium had been disturbed, such as hepatic encephalopathy, it was obtained from the patient’s family members.
Results
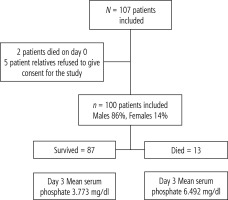
The study enrolled a sample of 107 patients as per the inclusion criteria, as shown in Figure 1; two of them died on the day of admission, while five others refused to give consent, leaving a total of 100 patients. Our study had male predominance: males, n = 86 (86%); females, n = 14 (14%). The baseline characteristics are listed in Table 1. The mean age of patients in our study was 42.96 ±9.73 years. As shown in Table 2, most common cause of chronic liver disease was alcohol, n = 77 (77%), followed by autoimmune hepatitis n = 7 (7%), chronic hepatitis B n = 6 (6%), etc. The most common cause of acute hepatic insult was alcoholic hepatitis, n = 53 (53%), then infections such as spontaneous bacterial peritonitis (SBP), etc., n = 15 (15%), alcoholic hepatitis with DILI, n = 11 (11%), autoimmune hepatitis (AIH) flare, n = 5 (5%), etc. Thirteen patients (13%) in our observational study died while the investigation was being conducted. All fatalities occurred after the seventh day; 11 happened in the second week and 2 in the third week. Table 3 presents a comparison of baseline (day 1) values for survivors and the dead. Statistical significance was reported with respect to haemoglobin levels, WBC counts, serum total protein, blood urea nitrogen (BUN), serum sodium, serum phosphate (SPO4), serum lactate, and serum creatinine levels. Mean WBC count, BUN, SPO4, serum lactate, and serum creatinine levels were higher while haemoglobin and serum total protein were lower in non-survivors. Mean serum phosphate values in the non-survivors’ group were higher (6.53 ±0.577 mg/dl) as compared to the survivors’ group (3.688 ±0.86 mg/dl) on presentation. However, no differences were found between the two groups with respect to age, platelet count, serum total bilirubin, serum aspartate aminotransferase (AST), serum alanine aminotransferase (ALT), serum alkaline phosphatase (ALP), serum albumin, and prothrombin time-international normalized ratio (PT-INR). A statistically significant difference was detected between the two groups with respect to the validated prognostication scores such as CTP, MELD, MELD-Na, AARC-ACLF, CLIF-C, and CLIF-SOFA scores, which were obviously higher in the non-survivor group (p < 0.05).
Table 1
Baseline demographic data calculated on day 1 of admission
Table 2
Day 1 characteristics
Table 3
Baseline characteristics of patients who survived vs. those who died
| Parameter | Survivors (n = 87) Mean ±SD | Died (n = 13) Mean ±SD | P value |
|---|---|---|---|
| Age (years) | 42.97 ±9.4659 | 42.84 ±11.8310 | 0.964 |
| Haemoglobin (g/dl) | 9.47 ±2.1422 | 8.02 ±1.4765 | 0.021* |
| Total leucocyte count (per mm3) | 9185 ±4839.815 | 12045 ±4944.25 | 0.05* |
| Platelet count (per mm3) | 137195.4 ±71727 | 122923.1 ±50077 | 0.491 |
| Total bilirubin (mg/dl) | 12.91 ±7.7642 | 15.83 ±7.1792 | 0.195 |
| Aspartate aminotransferase (IU/ml) | 143.06 ±120.6619 | 133.07 ±70.5991 | 0.772 |
| Alanine aminotransferase (IU/ml) | 77.62 ±91.2612 | 72.69 ±68.2695 | 0.852 |
| Alkaline phosphatase (IU/ml) | 150.63 ±88.1969 | 162.53 ±93.1402 | 0.655 |
| Total protein (mg/dl) | 6.71 ±0.8734 | 6.09 ±1.0602 | 0.022* |
| Serum albumin (mg/dl) | 2.63 ±0.5833 | 2.55 ±0.3619 | 0.619 |
| International normalised ratio | 2.03 ±0.4542 | 2.23 ±0.4424 | 0.145 |
| Serum sodium (mEq/l) | 132.81 ±5.4592 | 127.76 ±10.7715 | 0.009* |
| Serum phosphate (mEq/l) | 3.688 ±0.8624 | 6.53 ±0.5779 | 0.001* |
| Blood urea nitrogen (mg/dl) | 14.32 ±9.9702 | 22.92 ±15.5320 | 0.009* |
| Serum creatinine (mg/dl) | 1.01 ±0.5179 | 1.62 ±1.6523 | 0.008* |
| Serum lactate (mmol/l) | 1.53 ±0.6780 | 2.56 ±1.7356 | 0.001* |
| CTP score | 7.8 ±1.06 | 12 ±0.08 | 0.001* |
| MELD score | 23 ±2.99 | 33 ±4.14 | 0.001* |
| MELD-Na score | 24.5 ±3.24 | 35 ±4.14 | 0.001* |
| AARC-ACLF score | 7 ±0.7 | 12 ±0.78 | 0.001* |
| CLIF-C score | 28 ±2.54 | 72.8 ±3.55 | 0.001* |
| CLIF-SOFA score | 11.3 ±0.97 | 17.9 ±1.84 | 0.001* |
CLIF-SOFA – Chronic Liver Failure-Consortium-Sequential Organ Failure Assessment score, CLIF-C – Chronic Liver Failure-Consortium score, CTP – Child Turcotte Pugh score, MELD – Model for End-stage Liver disease, MELD-Na – Model for End-stage Liver disease-Natrium/sodium, APASL-ACLF Research Consortium-Asia Pacific Association for Study of Liver Disease (AARC-ACLF) score
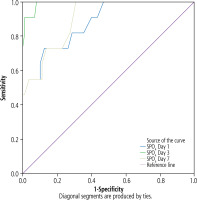
A statistically significant difference was also observed in the mean serum phosphate levels of the survivors and non-survivors on all measured days i.e., days 1, 3 and 7 (p < 0.001) (Table 4). The patients who died within 28 days had higher serum PO4 levels on days 1, 3, and 7 that were greater than 4.5 mg/dl (normal range 2.5-4.5 mg/dl). The mean range of serum phosphate levels for all the patients who did not survive was 6.53 ±0.577 mg/dl on day 1, 6.47 ±0.602 mg/dl on day 3, and 6.48 ±0.56 mg/dl on day 7. Figure 2A-C shows the mean SPO4 level in both survivors and non-survivors according to the grades of ACLF on days 1, 3, and 7, respectively. On day 1, 49 patients presented with grade I ACLF, 38 patients with grade II ACLF, and 13 patients with grade III ACLF. Day 1 mean SPO4 level in ACLF grade I was 3.64 mg/dl, in grade II was 3.757 mg/dl while in grade III it was 6.53 mg/dl. On day 3, almost all 38 patients with grade II ACLF reverted to grade I ACLF after undergoing treatment accordingly. Hence on day 3, 87 patients were with grade I ACLF and 13 patients with grade III ACLF. Day 3 mean SPO4 value in grade I ACLF was 3.773 mg/dl and in grade III ACLF was 6.492 mg/dl. Similarly on day 7, 87 patients continued to have grade I ACLF while 13 had grade III ACLF. Day 7 mean SPO4 in grade I ACLF was 3.868 mg/dl while in grade III ACLF was 6.484 mg/dl. Figure 2D shows mortality according to levels of serum phosphate levels with all deaths seen in values more than the normal SPO4 range. Table 5 gives a tabular view of all prognostic scores on days 1, 3 and 7 along with cut-off values and individual sensitivity, specificity, and accuracy values in predicting short-term mortality. On day 1, the CLIF-SOFA score with a cut-off value of 12 had the highest sensitivity (80%), highest specificity (74%), and highest accuracy (77%) as compared with the other scores. On day 3, the CLIF-SOFA score with a cut-off value of 11 had the highest sensitivity (82%), highest specificity (87%), and highest accuracy (83%). On day 7, the CLIF-SOFA score with a cut-off value of 10 had the highest sensitivity (89%), highest specificity (96%), and highest accuracy (93%). Amongst the remaining scores, the CLIF-C score had an accuracy of 71% on day 1 and was more than the remaining scores but day 3 and 7 accuracy scores were 73% and 83%, respectively, which were almost comparable with the remaining scores on those days. Serum phosphate values on days 1, 3, and 7 with cut-off values of 6.53, 6.47, and 6.48 (all in mg/dl) had an accuracy of 76%, 80%, and 87% in predicting poor prognosis and fared better when compared with all other prognostic scores except CLIF-SOFA, where it was better than SPO4 on all three days. Figure 3A-C shows three ROCs comparing all predictive scores with serum phosphate on days 1, 3, and 7. On ROC analysis as in Fig. 4, SPO4 values on days 1, 3, and 7 were compared. Values on day 3 had 92% sensitivity, 94% specificity, and 93% accuracy for mortality prediction, which was higher than the SPO4 values on days 1 and 7. The area under the curve for day 3 SPO4 was more than the area under the curve for day 1 and 7 SPO4 values.
Fig. 2
Mean SPO4 levels in ACLF grades on days 1 (A), 3 (B) and 7 (C) in survivors vs. non-survivors. D) Serum PO4 levels and deaths

Table 4
Serum phosphate levels in patients on days 1, 3 and 7 who survived vs patients who died
| Serum phosphate | Survivors (n = 87) Mean ±SD | Died (n = 13) Mean ±SD | P value |
|---|---|---|---|
| Day 1 | 3.689 ±0.8624 | 6.531 ±0.5779 | < 0.001 |
| Day 3 | 3.76 ±0.804 | 6.47 ±0.602 | < 0.001 |
| Day 7 | 3.86 ±0.834 | 6.48 ±0.56 | < 0.001 |
Table 5
Comparison of various prognostication scores on days 1, 3 and 7 in predicting mortality
CLIF-SOFA – Chronic Liver Failure-Consortium-Sequential Organ Failure Assessment score, CLIF-C – Chronic Liver Failure-Consortium score, CTP – Child Turcotte Pugh score, MELD – Model for End-stage Liver disease, MELD-Na – Model for End-stage Liver disease-Natrium/sodium, APASL-ACLF Research Consortium-Asia Pacific Association for Study of Liver Disease (AARC-ACLF) score
Discussion
Individuals with ACLF comprise a category of individuals with a poor prognosis and a high 28-day mortality rate. Several forecasting scores are available today to examine ACLF patients. A few of these are the AARC-ACLF score, CLIF-C, CLIF-SOFA, CTP, MELD, and MELD-Na. Dhiman et al. [11] investigated 50 patients with ACLF to compare CLIF-SOFA and APASL scores for predicting outcomes in ACLF, in which 86% were male, which was comparable to the current study. Furthermore, the average age of 46 ±13 years was noted in research conducted by Dhiman et al. [11], similar to our study sample. The most common cause of acute insult (alcoholic hepatitis and infection) as well as underlying chronic liver disease (alcohol related) in our study was like those seen in Western countries [5]. Active alcohol intake in our cohort could explain associated infections in the study as also the CANONIC study had sepsis as a cause of acute insult in most alcoholic patients, which may explain the associated infection in our study [5, 12]. Investigations by Dhiman et al. [11] and Barosa et al. [13] found alcoholic liver disease (68% and 79.7%, respectively) to be the most prevalent trigger of cirrhosis, as in the current study (77%).
ACLF according to APASL grading is associated with a 28-day mortality rate of 12.7% for grade I, 44.5% for grade II, and 85.9% for grade III ACLF [1]. However, in our observational study, grade I and grade II ACLF are not associated with early mortality while grade III ACLF is associated with 100% 28-day mortality. The above disparity could be due to selection bias as a large number of patients presented with grade I and grade II ACLF in our subset and due to early treatment at onset, many grade II patients reverted to grade I and thus fared better in terms of favourable outcomes.
Our study identified CLIF-SOFA as the best predictor of mortality on all three days followed by CLIF-C and then by AARC score. We searched for many comparative studies for prognostication in ACLF patients and found that most studies showed the superiority of CLIF-SOFA and CLIF-C scores over other scores such as CTP, MELD, and MELD-Na. Dhiman et al. [11] studied 50 ACLF patients and compared the AARC and CLIF-SOFA scores and concluded that CLIF-SOFA was the only significant independent predictor of 28-day mortality and was the better score. Barosa et al. compared scores in 132 ACLF patients in which the CLIF-C ACLF score was better than CTP, MELD, and MELD-Na in predicting 28-day mortality [13]. A systematic review by Rashed et al. which included ACLF patients by EASL definition showed that CLIF-SOFA was better than other prognostic scores for detecting 28-day mortality [14]. In a single-centre study by Chen et al. [15], eight prognostic scores in 249 ACLF patients admitted to the ICU were compared and the CLIF-C score outperformed CTP and MELD scores in predicting 28-day mortality, but AARC and CLIF-SOFA scores were not compared in the study. Song et al. [16] examined short-term mortality in ACLF patients diagnosed by both EASL as well as APASL definitions and found that CLIF-SOFA and CLIF-C ACLF scores had higher specificities with a fixed sensitivity than CTP and MELD in ACLF patients according to the CLIF-C definition. However, no such difference was found in patients according to the APASL definition. Zhang et al. [17] investigated 102 ACLF patients and found AUROCs for CLIF-SOFA higher than other forecasting scores at all points of time, like the outcomes of our study.
As per our knowledge and a PubMed search, no study yet has been conducted to compare SPO4 as a prognostic indicator with other validated scores. However, a few studies have been carried out in patients with acute liver failure (ALF) cases which shed light on the potential of SPO4 level as a prognostic indicator of mortality. An investigation by Baquerizo et al. [18] in 112 ALF patients found that analysis of SPO4 showed a statistically significant improved prognosis in patients with low/normal SPO4 and a bad prognosis with higher SPO4 levels, which is practically identical to our study findings. On the other hand, a cross-sectional descriptive investigation of 21 infants with ALF in Bangladesh by Rashid et al. [19] found that low SPO4 was linked with poor prognosis, contradicting our observations. Despite the above investigations being conducted on ALF patients, we did not find research on the impact of serum phosphate on ACLF patients.
India with its population of 1.4 billion people has 0.08 persons per million population as organ donors. Approximately 25,000 liver transplants (LT) are necessary per year in India, whereas by 2022, more than 1800 LT were achieved, the majority (80.7%) of which were live donor-related transplants (LDLT), in contrast to Western countries, where the majority (more than 90%) are deceased donor liver transplants (DDLT) [20, 21]. In India, the majority of liver transplants are carried out in private hospitals and approximately 2% of liver transplants probably take place in the public healthcare system [22]. Socio-economic factors along with cultural and religious beliefs and the absence of effective laws for LT are obstacles to promoting DDLT [23–25]. Furthermore, the cost of a liver transplant is extremely high, so many people cannot afford the medical care. A large percentage of patients at our centre are below the poverty level. Numerous medical facilities in India that cater to this cohort of the patient population, including ours, lack an in-house liver transplant unit. Therefore, predicting ACLF patients earlier with a simple blood examination marker such as SPO4 and adopting suitable actions at the earliest opportunity remains the most effective method for care.
In the present single-centre prospective observational pilot study undertaken in a non-transplant resource-limited environment in western India, we assessed serum levels of phosphate on days 1, 3, and 7 with various liver prognostic scores to forecast mortality at 28 days. Blood phosphate level as a prediction marker has already been explored in acute liver failure patients and it was found that normal levels of blood phosphate were related to an improved outcome and greater than average levels of serum phosphate have been linked with a bad prognosis [18].
There are some limitations to our observations. Firstly, SPO4 levels can also be affected in refeeding syndrome (RFS), which is defined as a medical complication resulting from fluid and electrolyte abnormality shifts due to aggressive nutritional intake. This causes a shift of electrolytes such as phosphorus from the blood to the intracellular compartment, leading to hypophosphataemia and other electrolyte deficiencies. Hypophosphataemia is a hallmark of RFS, generally seen in high-risk patients, as outlined by the National Institute for Health and Clinical Excellence (NICE) guidelines in 2006, updated in 2018 [26], who are chronically malnourished due to various causes and are given either enteral or parenteral alimentation rapidly. Incidence of RFS ranged between 0 and 60% and that of refeeding hypophosphataemia ranged between 7% and 62% in a recent meta-analysis [27]. However, in our study, patients who were found to have higher phosphate levels were the ones at higher risk of poor prognosis and death. Hence we cannot comment on the role that refeeding syndrome may play in the pathophysiology of ACLF patients in our study.
Secondly, some of the scores such as CTP, MELD, and MELD-Na were not meant for patients with ACLF but are still compared here as they are commonly used for evaluating the prognosis of patients with end-stage liver disease.
It is still unknown how serum phosphate levels in ACLF can be used to estimate short-term mortality. Therefore, this study was conducted to acquire an understanding of the role of serum phosphate in anticipating short-term mortality and its usefulness if confirmed as a simple blood examination in resource-limited situations. This is the first study to assess the function of serum phosphate in ACLF patients. The strengths of our study are that we have verified serum phosphate levels in patients suffering from ACLF and have established its precision as opposed to the verified standard scores for anticipating short-term death. Our study has the limitations of a single-centre observational study design and a small sample size. Randomized studies with larger sample sizes could yield efficient results. Nevertheless, further research with a more significant population cohort would be necessary to validate this study.
Conclusions
The high serum phosphate levels on day 3 with a value of more than 6.4 mg/dl have shown almost comparable accuracy with CLIF-SOFA for screening short-term mortality. Hence serum phosphate measurement can be used as a simple bedside laboratory investigation to predict mortality in ACLF patients and early interventions in low-resource settings.