Introduction
Psoriasis (Pso) is an inflammatory autoimmune skin disease that affects approximately 3% of the world’s population [1, 2]. Pso is an immune-mediated disease involving the innate and adaptive immune systems together [3]. This is a genetic disease caused by multiple risk factors involving multiple mechanisms including inflammation, antigen presentation, and cellular and transcriptional regulation [4]. Pso can involve different parts of the body including the scalp, elbows, knees, and even the lumbosacral area [5]. Previously, Pso was considered a specific disease of the skin, but today Pso is generally understood as an inflammatory disease associated with a high risk of disease throughout the body, including symptoms of cardiometabolic disease and various psychological disorders that can affect the patients [6, 7]. High BMI, and elevated body fat and body weight are associated with risk of Pso development [8]. A literature review showed several pathways between physical inactivity and inflammatory disease, such as increased adiposity, adhesion molecules, and lipid peroxidation, which can appear in Pso disease [9]. Physical activity has been shown to provide many psychological benefits, such as improved mood, which has positive effects for people with Pso, who are at higher risk of depression. Exercise has even been shown to improve disease outcomes and inflammation in people with psoriatic arthritis [10, 11]. The benefits of this exercise can be attributed to several mechanisms that not only reduce fat but also reduce oxidative stress, which can lead to the development of diseases in Pso. Moderate exercise has been confirmed to have an effect on Pso by increasing ROS/RNS generation and disrupting redox homeostasis, exacerbating inflammation of cells and organs [12, 13]. People with Pso tend to have lower physical activity than people without Pso, so they are at higher risk for comorbidities and underlying disease [13, 14]. Some researchers have reported that people with Pso avoid physical activity more than the general population, but other researchers have described similar levels of physical activity in people with and without Pso [15]. The certain effects of vigorous activity on Pso and the relationship between physical activity and Pso is unknown. There is a hypothesis that physical activity can affect the risk of Pso through its effects on mediators of the inflammatory system [16]. Immune activation may be modulated by vigorous activity, which can predispose people to Pso. We know that anti-inflammatory cytokines can play an important role in the pathogenesis of Pso, and some inflammatory-related disease or conditions, such as obesity, can reduce the risk of Pso. Physical activities can decrease inflammation and significantly reduce the levels of pro-inflammatory cytokines and leptin, as well as increase the levels of anti-inflammatory cytokines, including adiponectin [17]. Hence, physical activity can play an important role in Pso prevention. Unfortunately, despite the vital role of exercise in reducing the severity of symptoms of psoriatic patients and the possibility of reducing the incidence of Pso following exercise, little research has been done on this issue, and controversial findings have been reported.
Therefore, in the present study, by conducting a meta-analysis, we hope to find a documented conclusion about the effect of exercise on Pso.
Methods
Search method
We designed this study according to the Systematic Reviews and Meta-Analyses (PRISMA) statement. The study is registered as a meta-analysis at the Open Science Framework with registration number http://osf.io/eaf9z. The ISI, Scopus, PubMed, Cochrane library, and Google Scholar databases were used to search articles up to the end of May 2024. Also, to manage electronic resources, EndNote was used.
The PubMed search process was performed using the following mesh terms:
(“Psoriasis / physical activity “[Mesh] OR “Psoriasis/Movement “[Mesh] OR “Psoriasis/sport “[Mesh])) AND “ Psoriasis, Exercise “[Mesh])) OR. For other databases, we used these keywords: psoriasis, exercise and physical activity (Figure 1).
Scores and parameters
We used the Demirel [17] physical activity index and metabolic equivalent task (MET) minutes details of studied patients at published articles.
Inclusion and exclusion criteria
Inclusion criteria were controlled clinical trials, randomised controlled trial studies, and prospective and retrospective cohort studies. Case studies, in vitro studies, reviews, and case reports were excluded from the present article.
Data extraction methods
Data extracted from the studies included design of study, sample size, mean age, BMI, and gender. Risk ratio with 95% CI, and fixed and Mantel-Haenszel methods were calculated. Random effects were used for potential heterogeneity, and I2 showed heterogeneity. I2 values > 50% signified moderate-to-high heterogeneity. RevMan statistical software was used for evaluation of this meta-analysis.
Results
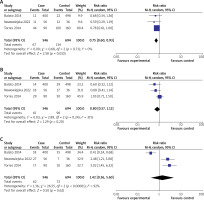
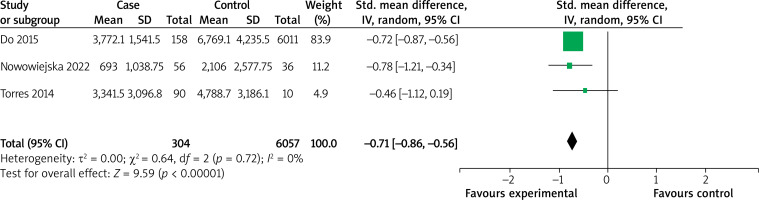
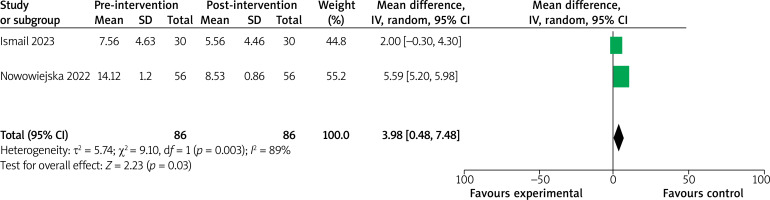
Based on the mentioned methods, 1319 articles were extracted from the databases, including 683 articles from Embase, 311 from PubMed, 71 from Cochrane Library, and 254 from Science Citation Index Expanded. Firstly, 1089 articles were excluded because of inaccurate title or abstract. Then from the other 230 articles, 191 articles were excluded due to not reporting details of physical activity like level of activity or MET information. Out of the 39 remaining articles, 33 articles were excluded as being duplicate studies. Finally, 7 articles [18–24] were selected for analysis. Articles were published between 2014 and 2023 and included 2 articles from Italy, one article from Portugal, one article from Korea, one article from Egypt, one article from Poland, and one article from Spain. The minimum sample size was 30 and the maximum sample size was 400 people for the case groups, and in the control groups the sample size varied from 30 to 6011 in different studies, and the total number of patients in 7 articles was 7847. The lowest mean age was 35.5 ±6.1 years, and the highest mean age was 53.5 ±16.7 years. The details of these 7 articles are presented in Table 1. The selected studies presented the relationship between Pso and physical activity by 3 different indexes. The first focused index was severity of exercise, which was divided into high, moderate, and low level. The results of the meta-analysis of studies showed that high-intensity exercise is significantly lower in Pso patients than in healthy people (RR = 0.75; 95% CI: 0.60–0.93; p = 0.010). But there was no significant difference between the 2 groups for the moderate-intensity exercise (RR = 0.80; 95% CI: 0.57–1.12; p = 0.20) and low-intensity exercise (RR = 1.42; 95% CI: 0.36–5.60; p = 0.62), which is presented in Figures 2 B and C. Also, the studies compared MET differences between Pso and healthy groups. The results of the meta-analysis of studies showed that MET in the Pso group was significantly lower than healthy controls (SMD = –0.71; 95% CI: –0.86–0.56; p < 0.00001) (Figure 3). The final important finding of the present study was the investigation of the effect of exercise on the changes in the PASI score of psoriatic patients. The analysed result showed that post-exercise PASI score decreased significantly in psoriatic patients (SMD = 3.98; 95% CI: 0.48–7.48; p = 0.03) (Figure 4).
Table 1
Characteristics of the included studies
| Ref. | Author | Year | Country | Case number | BMI | Age | Female gender | Control number |
|---|---|---|---|---|---|---|---|---|
| [18] | Balato | 2014 | Italy | 400 | 24.1 | 42.9 ±18.1 | 47% | 489 |
| [19] | Naldi | 2014 | Italy | 151 | 30.8 | 53.5 ±16.7 | 24.4 % | 152 |
| [20] | Torres | 2014 | Portugal | 90 | 28.6 | 47.7 ±10.9 | 38.9 | 160 |
| [21] | Do | 2015 | Korea | 158 | 30.6 | 41.45 | 54.45% | 6011 |
| [22] | Nowowiejska | 2022 | Poland | 56 | 27.33 | 49.03 ±2.2 | 44.64 | 36 |
| [23] | Ismail | 2023 | Egypt | 30 | 31.85 | 44.03 ±3.59 | 0% | 30 |
| [24] | Diaz | 2023 | Spain | 59 | 31.7 | 35.5 ±6.1 | 0% | 59 |
Discussion
Pso is a skin disease characterised by sharply demarcated whitish scaled erythematous plaques [25, 26]. Pso prevalence varies by location, and Pso can appear at any age, showing that genetic background, ethnicity, and environmental factors can affect the onset of Pso [27]. Pso can manifest with several different underlying or comorbid diseases, such as atherosclerosis, obesity, hypertension, diabetes, gastrointestinal diseases, cardiovascular diseases, and osteoporosis [28, 29]. Shared inflammatory pathways and cellular mediators are hypothesised as subsidising origins. Previous research shows that obesity has a relationship with the onset of Pso [30]. Obesity is significantly prevalent in Pso patients [31, 32], and the body fat percentage significantly is elevated in Pso. Also, obesity is a consequence of Pso by causing physical inactivity, depression, social isolation, and a high-fat diet [33]. Conversely, some researchers showed that high body mass index may cause PsA rather than being a consequence [34, 35]. Low-intensity exercise can possibly be a Pso risk factor, but Pso itself could be a barrier to physical exercise in Pso patients. Overall, conclusive evidence points to the protective impact of exercise in reducing the risk of Pso development. However, limited evidence exists on the benefits of exercise and its extent in the management of Pso in affected patients [36, 37]. Physical activity not only decreases the severity of Pso lesions, but it can also prevent the occurrence of metabolic syndrome by reducing adiposity, oxidative stress, inflammation, and adhesion molecules [21].
Studies that have investigated the role of exercise in the occurrence of Pso and the role of exercise in reducing the severity of Pso, included in this systematic review and meta-analysis to identify the role of exercise in Pso patients. As mentioned in the methods and results section, 7 articles were finally analysed in our study. Our finding showed that high-intensity exercise is significantly less common in Pso patients than in healthy people (RR = 0.75; 95% CI: 0.60–0.93; p = 0.010), and MET in the Pso group was significantly lower than in healthy controls (SMD = -0.71; 95% CI: –0.86–0.56; p < 000001). This means that psoriatic patients do less physical activity and exercise than healthy people, which is the first important problem in this patient lifestyle. A more important finding of our study was the relationship of exercise with reducing severity of Pso by PASI score investigation. We found that the post-exercise PASI score decreased significantly in psoriatic patients (SMD = 3.98; 95% CI: 0.48–7.48; p = 0.03), which means that exercise intervention is possible as a therapeutic method for Pso patients. Although the role of exercise in Pso has received little attention from researchers, it has been reported in the literature that exercise not only reduces the incidence of Pso, but also reduces the severity of the disease and improves the quality of life of patients. Exercise also decreases the cardiovascular risk and metabolic diseases in these patients [38, 39]. In another meta-analysis article, Mahil et al. reported that weight loss may prevent the onset of Pso in obese patients [39]. Another meta-analysis, published by Upala et al., showed that alternative, nonsurgical weight loss is associated with decreased Pso severity in obese patients, which emphasised the role of physical activity and exercise [40]. Other study by Naldi et al. also reported that exercise decreased the severity of Pso in obese patients with Pso [19]. The results of other articles also show that psoriatic patients tolerate these exercise well, and it is possible to suggest exercise to treat the disease and reduce its severity. In one of the studies, Diaz et al. reported that aerobic exercise at a moderate level was well tolerated, safe, and effective in Pso patients [24].
Conclusions
The results of the current meta-analysis article show that high-intensity exercise is significantly less common in Pso patients than in healthy people and that MET in the Pso group was significantly lower than in healthy controls. Post-exercise PASI score decreased significantly in psoriatic patients, which means that exercise intervention can be suggested as a therapeutic method for Pso patients. New clinical trials may improve this finding and extend the general compliance of using exercise as new a method of preventing Pso and reducing its severity.