Introduction
Pediatric inguinal hernia (PIH) stands out as a prevalent condition among the pediatric population, with an incidence rate ranging from approximately 0.8% to 4.4% [1, 2]. Recently, there has been a discernible uptick in the prevalence of PIH, necessitating the exploration of innovative and minimally invasive surgical modalities. Notably, laparoscopic pediatric inguinal hernia repair (LPIHR) has emerged as a promising procedure, offering an array of advantages compared with conventional repair, such as less postoperative pain, shorter recovery periods, and enhanced cosmetic outcomes [3, 4]. This shift from conventional open repair to laparoscopy in pediatric hernia cases is evidenced by a fivefold increase in the proportion of cases treated laparoscopically between 2009 and 2018 [5, 6].
While previous research has evaluated disparate intra-abdominal pressures during laparoscopy in adults, similar studies in PIH cases undergoing LPIHR are rare. Previous studies suggested that high intra-abdominal pressure during laparoscopic procedures may influence respiratory, circulatory, and neuroendocrine systems, a phenomenon particularly pronounced in pediatric cohorts, which are characterized by heightened sensitivity to fluctuations in intra-abdominal pressure [7]. Conversely, low intra-abdominal pressure may compromise visualization of the surgical field and affect the performance of intricate procedures; in severe instances, safety may be jeopardized. Consequently, this study aimed to meticulously evaluate the safety and efficacy of low pneumoperitoneum pressure (LPP) compared with the established standard pneumoperitoneum pressure (SPP) in LPIHR.
Aim
The aim of this study was to evaluate the benefits of LPP vs. SPP in laparoscopic pediatric inguinal hernia repair.
Material and methods
This retrospective study was performed in a tertiary hospital that performs over 300 laparoscopic PIH repairs annually. This study was performed from January 2022 to August 2023 and was approved by the institutional research and ethics board of our hospital. The aim of the study was to evaluate the benefits of low pneumoperitoneum pressure in LPIHR. Patients admitted during the study period were divided into two groups: an SPP group and an LPP group. We retrospectively reviewed the medical records of PIH patients who underwent laparoscopic repair. Data were collected from the electronic operation and anesthesia medical records. The evaluated parameters comprised age, location of the hernia, operation time, anesthesia time, postanesthesia care unit (PACU) time, peak partial pressure of end-tidal carbon dioxide (PETCO2) during anesthesia, trough PETCO2, PETCO2 at the end of surgery, length of hospitalization, and postoperative complications. Operation time was defined as incision time to the end of surgery. Anesthesia time was defined as the start of drug administration for anesthetic induction to the removal of the endotracheal tube.
Laparoscopic procedure
After successful anesthesia induction, the patient is positioned supine. A 5-mm skin incision is made along the umbilical edge to create pneumoperitoneum. The established pneumoperitoneum pressure is maintained at 8 mm Hg (SPP) or 6 mm Hg (LPP). A 5-mm diameter trocar is inserted, and a 2-mm incision is created at the body surface projection of the right inner ring orifice. The threaded hernia needle is then guided into the extraperitoneal space to encircle half of the inner wall of the inner ring orifice then proceeds around the posterior wall of the hernia sac and is pulled through, leaving a 2-0 non-absorbable suture within the abdominal cavity. The needle is retracted outside the peritoneum, circling half way around the hernia sac from the inner ring’s lateral wall. The original non-absorbable suture remaining in the abdominal cavity is lifted out of the incision, allowing for the release of air and fluid from the hernia sac and subsequent tying. A meticulous check ensures no bleeding in the abdominal cavity, absence of hematoma around the sutures, and correct instrument count. The pneumoperitoneum is then desufflated, the trocar is removed, and the umbilical margin incision is sutured.
Statistical analysis
All data were analyzed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Nonparametric variables were presented as the median (interquartile range), while categorical variables were presented as percentages. Group comparisons were performed using Fisher’s exact test, the χ2 test, and one-way analysis of variance. Statistical significance was set at p < 0.05.
Results
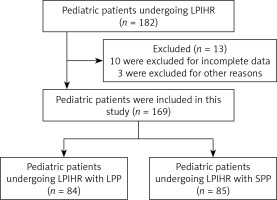
The patient flowchart is shown in Figure 1. A total of 169 eligible patients were enrolled in this study, of whom 107 (53.92%) were male and 62 (46.08%) were female. The mean age of the included patients was 5.20 years. There were 49 patients with unilateral hernias and 35 patients with bilateral hernias in the LPP group, compared with 51 patients with unilateral hernias and 34 patients with bilateral hernias in the SPP group (Table I).
Table I
Characteristics of included patients
Figure 1
The patient flowchart
LPIHR – laparoscopic pediatric inguinal hernia repair, LPP – low pneumoperitoneum pressure, SPP – standard pneumoperitoneum pressure.
Anesthesia characteristics
The anesthesia characteristics are shown in Table II. There was no significant difference between the LPP and SPP groups for operation time (18.37 ±7.72 min vs. 19.52 ±7.72 min, respectively). The anesthesia time in the LPP group (61.17 ±13.06 min) was shorter than that in the SPP group (67.62 ±16.35 min). The LPP group had a shorter PACU time (25.42 ±8.87 min) than that in the SPP group (28.47 ±5.93 min). Regarding PETCO2 values (mm Hg), the LPP group had lower values for peak PETCO2 (33.37 ±4.09 vs. 36.56 ±4.08), trough PETCO2 (38.33 ±5.04 vs. 40.46 ±4.14), and PETCO2 at the end of surgery (35.29 ±4.59 vs. 38.76 ±4.22). Regarding the anesthesia drugs, the LPP group required less sufentanil citrate (8.76 ±4.07 ml vs. 18.03 ±16.04 ml) and midazolam (1.56 ±0.45 ml vs. 1.79 ±0.59 ml) (Table II).
Table II
Anesthesia characteristics of included patients
Patients’ postoperative characteristics
Postoperative complications occurred in 2 patients in the LPP group and 1 patient in the SPP group (Table III). One patient developed a seroma and one developed a hematoma in the SPP group, while 1 patient developed a hematoma in the LPP group. No patients developed a surgical site infection in either group. There was no in-hospital or 30-day mortality. One patient in the SPP group developed recurrence 6 months postoperatively (Table III).
Table III
Postoperative characteristics of included patients
Discussion
In this retrospective investigation, we performed a comparative analysis between LPP and SPP in LPIHR, focusing on both efficacy and safety metrics. Our findings suggest that LPP is associated with shorter anesthesia and PACU times, and lower peaks and troughs for PETCO2 compared with SPP. Moreover, no statistically significant differences were identified for operation time, postoperative complications, or the recurrence rate between the two groups.
Laparoscopic hernia surgery, owing to its benefits of minimal trauma and rapid recovery, has become the predominant approach for pediatric hernia treatment. However, as the procedure necessitates general anesthesia and insufflation of CO2 into the abdominal cavity, potential complications, such as hypoxemia and hypercapnia, are concerns [8, 9]. The increased intraperitoneal pressure pushes the diaphragm toward the head, causing a decrease in lung capacity, which may increase the frequency of compression atelectasis [10, 11]. A previous study reported that high PETCO2 was associated with higher rates of acute lung injury after surgery compared with low PETCO2 [12]. The current study showed that LPP resulted in lower values for peak and trough PETCO2, and PETCO2 of the end of surgery, compared with SPP. Lower PETCO2 may shorten anesthesia time. In our study, anesthesia and PACU times in the LPP group were lower than those in the SPP group. Growing concerns about the impact of general anesthesia on the neurodevelopment of children underscore the need to reduce anesthesia duration, particularly with the increased use of laparoscopic techniques in PIH treatment [13, 14]. Our study indicates that under low intra-abdominal pressure, the anesthesia time for PIH was shorter compared with SPP, leading to a shorter postoperative recovery period.
In our investigation, LPP was associated with a comparable operative time to that with SPP, indicating that LPP could result in a satisfactory surgical field in laparoscopic inguinal hernia repair. Furthermore, regarding postoperative complications, our study revealed no significant differences in early postoperative complications and short-term recurrence rates between the two patient groups. Additionally, our LPP group required less sufentanil citrate and midazolam, as anesthesia drugs. A reduction in medications may also reduce the effects of anesthesia in children.
Several limitations exist in the current study. The primary limitation is that the retrospective design introduced potential bias. This study was neither prospective research nor a randomized controlled trial, which may have resulted in selection bias. Second, selection bias related to the surgeons might have existed. Third, the follow-up time in this study was short, and there was a lack of data on long-term postoperative complications and recurrence rates.








