The surgical removal of a displaced Amplatzer Amulet occluder (Abbott, Abbott Park, Illinois, USA) is an exceptionally rare procedure in medical practice. This letter to the editor illuminates the intricate aspects involved in addressing such an unusual complication. The surgical intervention included not only the extraction of the occluder but also the establishment of coronary artery bypass grafting and closure of the left atrial appendage using an AtriClip. It is crucial to underscore the infrequency of complications of this nature, with only a limited number of documented cases in the medical literature [1–3].
Left atrial appendage occluders, such as the Amplatzer Amulet, find application in specific clinical scenarios. These devices are typically employed in cases of atrial fibrillation (AF), particularly when anticoagulation therapy poses a challenge or is contraindicated. The decision to use occluders is often guided by factors such as a history of stroke, bleeding complications related to anticoagulation, or patient preference [4]. Procedures involving the deployment of left atrial appendage occluders are considered in carefully selected patients to mitigate the risk of thromboembolic events.
A 75-year-old male patient urgently presented at the Cardiothoracic Surgery Department due to the displacement of an Amplatzer Amulet occluder from the left atrial appendage into the left atrial cavity, necessitating immediate surgical intervention.
The patient’s medical journey began in 2015 with a significant cardiac event leading to the implantation of a stent (SYNERGY, Boston Scientific, USA) for the occluded left anterior descending coronary artery. Subsequent to this, in March 2016, he was readmitted for nonspecific chest discomfort, resulting in a modification of pharmacological treatment and discharge in good condition. During this hospitalization, the diagnosis of heart failure with reduced ejection fraction (HFrEF) was established.
Further cardiac history included a planned implantation of an implantable cardioverter-defibrillator (ICD) in November 2017 for primary prevention. In November 2018, coronary angiography was performed due to nonspecific chest pain, revealing no significant changes and prompting adjustments to pharmacological treatment. AF was diagnosed at the beginning of 2019, and the subsequent management followed established guidelines. In June 2019 and September 2021, the patient underwent hospitalizations for electrical cardioversion, successfully achieving normal sinus rhythm on both occasions. The treatment, including anticoagulation therapy, was administered in accordance with the guidelines. In September 2023, neurological symptoms led to admission to the neurology department, with subsequent rehabilitation and speech therapy evaluation during the stay. In October 2023, the patient underwent a preliminary assessment for the closure of the left atrial appendage, culminating in discharge. A subsequent admission in the same month to the cardiology department resulted in the percutaneous closure of the left atrial appendage using the Amplatzer Amulet (Figure 1), with an uncomplicated procedure leading to discharge 2 days later. However, in December 2023, the patient faced a sudden deterioration of vision in the right eye, prompting urgent admission to the cardiology department. Echocardiographic evaluation revealed the dislodgment of the Amplatzer Amulet clip into the left atrium, necessitating intervention. Subsequently, he was transferred to the Cardiothoracic Surgery Department for the surgical removal of the displaced Amplatzer Amulet clip. An intracardiac device was successfully removed, and the left atrial appendage was closed using a stapler (AtriClip 40 mm, AtriCure, USA) (Figure 2). The procedure also involved the placement of a venous graft to the left anterior descending coronary artery (LAD). Following a 10-day hospitalization, during which the patient’s condition improved significantly, he was discharged to a cardiac rehabilitation facility.
Figure 1
Intraoperative fluoroscopic image capturing the Amplatzer Amulet occluder during coronary angiography (arrow)
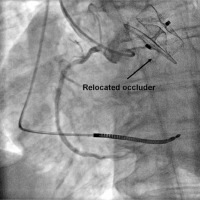
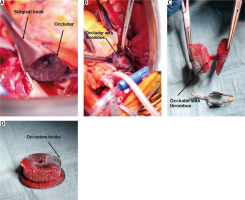
Figure 2
The Amplatzer Amulet occluder in the surgical field protruding from the left atrial appendage before its removal from the heart cavity. The occluder extracted from the cardiac chamber during the procedure. Removed occluder with the accompanying thrombus. The occluder removed from the site, revealing the visible hooks used for attachment
The application of occluders, such as the Amplatzer Amulet and Watchman, is commonly considered in patients with atrial fibrillation, particularly in scenarios where conventional anticoagulation may be challenging or contraindicated. According to the medical literature, primary indications include the reduction of stroke risk in atrial fibrillation patients, especially those with additional risk factors such as prior strokes or a predisposition to bleeding. Occluders are also contemplated for patients with contraindications to prolonged anticoagulant therapy [5].
The literature underscores that the choice between various occluders should be individually tailored to the clinical profile of the patient and the preferences of the treating physician. Available data suggest that the efficacy and safety profiles of the Amplatzer Amulet and Watchman are comparable, substantiating their role in the comprehensive management of patients with atrial fibrillation and an elevated risk of stroke.
Surgical interventions for atrial fibrillation often involve closure of the left atrial appendage (LAA) and radiofrequency (RF) ablation during cardiothoracic procedures [6]. The closure of the LAA is commonly achieved using devices such as the AtriClip, aiming to reduce the risk of thromboembolic events associated with atrial fibrillation. This procedure involves the mechanical closure or stapling of the LAA, mitigating the potential for blood stasis and subsequent clot formation [7]. The collaborative efforts of cardiologists and cardiothoracic surgeons not only saved the endangered life of the patient following the implantation of the Amplatzer Amulet occluder but also facilitated the realization of all therapeutic benefits. Surgical interventions, including closure of the left atrial appendage and RF ablation, leveraging advanced techniques and devices, constituted an integral part of a comprehensive strategy for treating atrial fibrillation. This seamless collaboration proved instrumental in effectively minimizing the risks associated with atrial fibrillation complications, underscoring the pivotal role of synergy between cardiology and cardiothoracic surgery specialists in achieving comprehensive therapeutic outcomes.






