Hypotension during general anaesthesia lasting for even short periods of time can have deleterious effects in the postoperative period [1]. Multi-ple studies have demonstrated the relationship between intraoperative hypotension (IOH) and increased postoperative morbidity and mortality secondary to IOH-induced organ injury (myocardial lesions, stroke, kidney injury, splanchnic hypoperfusion) in surgical patients [1, 2]. Identifying patients at high risk of haemodynamic instability during anaesthesia induction can allow the anaesthesiologist to modify the anaesthetic dosing or administration rate, pre-emptive fluid administration or initial vasoactive medication use [3]. The stability of blood pressure during induction of anaesthesia is of major importance as hypotension during this period may lead to decreased tissue perfusion and organ injury, with an adverse impact on patient outcome [4, 5]. The probability of postinduction hypotension (PIH) increases with age, body mass index, increased blood pressure at the time of operating room arrival, diabetes mellitus type II and high ASA scores [6, 7], most of which are unmodifiable risk factors for PIH. Latent volume depletion is a modifiable risk factor of high clinical relevance.
Correct assessment of fluid status is a difficult task in clinical practice. Hypovolaemia is presumed to be a common factor of PIH, despite worldwide improvement in preoperative volume optimization, avoiding unnecessary fasting and bowel preparation [7]. The utility of non-invasive ultrasound assessment by anaesthesiologists could be important in the assessment of haemodynamic status [8]. Although several studies have investigated the use of preoperative inferior vena cava ultrasound examination, its use for PIH prediction is heterogenous both in methodo-logy and in results, with a large difference between observed sensitivities and specificities [9]. Therefore, preoperative identification of latent hypovolaemia can prompt the anaesthetist to ini-tiate fluid admi-nistration before induction of anaesthesia.
In patients undergoing chronic haemodialysis, bioimpedance-based methods are frequently used to measure body composition [10, 11]. Bioimpe-dance analysis (BIA) is used to assess body composition and estimate total and extracellular water volumes based on the tissue’s capacity to conduct electrical impulses [12]. Bioimpedance spectroscopy (BIS) is a safe, simple, fast and unique bioimpedance approach that is frequently used in clinical practice [13]. As compared with other methods, which are costly, unnecessarily invasive in most elective surgical procedures, with high complication rates (pulmonary arterial catheter, transpulmonary haemodilution technique, etc.) [14] or highly heterogenous in estimation [9], BIS objectively and easily assesses the preoperative fluid status, and may indicate fluid depletion correction, avoiding hypotension at anaes-thesia induction.
The study’s main purpose was to determine the correlation between the preoperative BIA assessed fluid status and PIH.
Methods
This study was performed on the same cohort of patients as a previously published prospective observational single centre study which investigated the relationship between arterial stiffness and PIH. All the details of the study design, inclusion and exclusion criteria have been previously published [15].
Bioimpedance measurement
Bioimpedance measurements were performed with a commercial device, the Body Composition Monitor (BCM; Fresenius Medical Care, Bad Homburg, Germany), a portable whole-body multifrequency bioimpedance analysis device. The BCM measures body resistance and reactance to electrical currents of 50 discrete frequencies, ranging from 5 to 1000 kHz [16]. It can assess total body water (TBW) and extracellular water (ECW) [8]. The Chamney physiological tissue model, which considers the person’s weight, height, and gender, is used to provide values for TBW and ECW [17].
The BCM displays absolute fluid overload (AFO), the difference between normal (expected) and actual (measured) ECW (expressed in litres) and the relative fluid overload (RFO), calculated as absolute fluid overload/extracellular water ratio (AFO/ECW) expressed in percentages. A negative AFO indicates the patient’s underhydration, while a positive one indicates overhydration. Based on RFO values, we classified the hydration status into three categories: dehydrated (RFO < –10%), normohydrated (–10% ≤ RFO ≤ 15%), and hyperhydrated (RFO > 15%).
The bioimpedance measurements were performed by a trained operator according to the manu-facturer’s recommendations. The measurement was performed 2 hours before the surgery. After explaining the procedure, blood pressure, body height, and weight were measured and the patient placed in the supine position. After cleaning the skin with alcohol solution, four dedicated skin electrodes were placed on the right wrist and ankle. To minimize electrical disturbances at the time of measurement, contacts between the patient and metallic bed parts were excluded. The patient’s weight and height were entered into the device, and measurements were recorded. Successful completion of the measurement was checked in real time on the device using a signal quality index > 85% and a Cole-Cole Gaussian curve. Measured and derived parameters were displayed within 2 minutes.
Induction of anaesthesia protocol and PIH
As mentioned in the published data [15], we protocolized pre-anaesthetic evaluation and anaesthesia induction. We defined PIH as the blood pressure decrease occurring during the first 10 minutes after induction of anaesthesia and orotracheal intubation before surgical incision and used the same definition for hypotension as in the previously published study [15]. Baseline blood pressure was the one measured 2 hours before induction of anaesthesia, when BIA was performed. During the intervention, non-invasive arterial blood pressure was assessed every minute during the first 10 minutes after the induction of anaesthesia.
Statistical analysis
All analyses were performed using Stata SE software, version 13 (Stata Statistical Software: Release 12. College Station, TX: Stata Corp LP). Continuous data are presented as mean ± standard deviation (SD), median with interquartile range (IQR), and categorical data as number and percent frequency. The between-group comparisons were performed using the χ2 or Fisher test, the Mann-Whitney U test or the independent t-test, as appropriate. The distribution of the variables was assessed using the Shapiro-Wilk test.
Logistic and linear regression analyses were used to assess the relationships between different variables derived from the bioimpedance analysis (TBW, ECW, intracellular water [ICW], AFO, RFO and ECW to ICW ratio) and PIH incidence and duration. For the multiva-riable analysis, as in the previous analysis [15], we selected a priori, based on existing knowledge and literature, the following confounders: age, gender, ASA physical status, comorbidities (coronary artery disease, blood hypertension, diabetes mellitus and malignancy) and medication (β-blocker and angiotensin II receptor blockers/angiotensin converting enzyme inhibitors use). When needed, we performed bootstrapping validation to avoid the problem of overfitting owing to the low number outcomes (PIH at different thresholds). A 2-tailed P < 0.05 was considered statistically significant.
Results
Study population characteristics
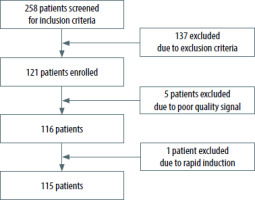
Out of the 258 patients screened for inclusion criteria, 115 patients were included in the final ana-lysis (Figure 1).
The baseline characteristics of the study population were previously presented [12]. The mean age was 58.1 years and 69.6% were female (Table 1). More than 60% of the study population had the dia-gnosis of cancer.
TABLE 1
Baseline characteristics of the study population (N = 115)
The incidence of PIH, defined as a decrease in systolic (SBP) and mean blood pressure (MBP), or a as a relative decrease of SBP and MBP from baseline, is presented in Table 2.
TABLE 2
Incidence of postinduction hypotension (PIH) using different thresholds
BIA assessed fluid status and incidence of PIH
In the univariable analysis, TBW was associated with the development of PIH when defined as an absolute SBP decrease < 80 mmHg and as a relative MAP decrease of > 20% from baseline (Table 3). In the multivariable analysis, only the association with an absolute SBP decrease < 80 mmHg remained statisti-cally sig-nificant (OR = 0.91, 95% CI: 0.83–0.99) (Table 3).
TABLE 3
The relationship between total body water (L) and postinduction hypotension (PIH) using different thresholds
Similar results were obtained for ICW. It was asso-ciated with the development of PIH when defined as an absolute SBP decrease < 80 mmHg and as a relative MAP decrease of > 20% from baseline (Table 4). In the multivariable analysis, only the association with an absolute SBP decrease < 80 mmHg remained statistically significant (OR = 0.85, 95% CI: 0.74–0.99) (Table 4).
TABLE 4
The relationship between intracellular water (L) and postinduction hypotension (PIH) using different thresholds
There was no association between ECW, AFO, RFO, and PIH incidence in the univariable and multivariable analysis, as shown in Supplementary Tables 1, 2 and 3, respectively.
BIA assessed fluid status and duration of PIH
There was no correlation between any of the BIA-derived parameters of fluid status and the duration of PIH (see Tables 5 and 6 and Supplementary Tables 4, 5 and 6).
TABLE 5
The relationship between total body water and duration of postinduction hypotension (PIH) using different thresholds
TABLE 6
The relationship between intracellular water and duration of postinduction hypotension (PIH) using different thresholds
Discussion
To our knowledge, this is the first study that has investigated the relationship between fluid status assessed using BIA and PIH. We found that TBW and its ICW component were the only two BIA-derived parameters associated with the development of PIH.
BIA is a simple technique that provides an objective assessment of fluid status with numerical results. It is helpful even in the case of patients with subclinical abnormalities. BIA was validated by isotope dilution methods [11], the gold standard for assessing body fluid composition, and is commonly used to guide fluid removal in dialysis patients [16, 18]. BIA defines the hydration status of an individual based on normal extracellular volume and body composition [19]. It performs well for healthy subjects and chronic patients with major and subtle water distribution disturbances [20]. BIA measures ECW but cannot discriminate between extravascular and intravascular volume [21]. Steinwandel et al. [22] evaluated whether intravascular volume status in haemodialysis patients measured by inferior vena cava ultrasound correlates with BIA values. Their results showed agreement between the two fluid assessment methods, concluding that both can determine the risk of intradialytic hypotension [22]. We used the cut-off BIA value for defining normo-, over- and dehydrated patients, as recommended for chronic patients undergoing haemodialysis. Other authors used the same values for perioperative fluid status assessment [23].
The ability to assess patient fluid status is an essential part of perioperative care. There is a need to identify easily available variables that can help clinicians recognize a modifiable risk factor for developing hemodynamic instability during sur--gery [24]. Hypovolaemia is probably the most important factor associated with PIH [7]. In the case of overt hypovolaemia, anaesthesia induction protocols are adapted to avoid or minimize PIH. Subtle, subclinical dehydration escapes clinical exa-mination. Based on the assumption of preoperative dehydration, administering a variable amount of intravenous fluid before anaesthesia induction is frequently encountered in clinical practice, even though increased intraoperative fluid balance is associated with increased postoperative morbidity and mortality [25, 26]. Preoperative BIA examination is a sensitive method that allows objective assessment of patient fluid status, being able to detect subclinical changes.
Using a protocol for anaesthesia induction and monitoring, we aimed to exclude induction agents as risk factors for PIH.
As previously reported for the same study group population, arterial stiffness identifies patients at risk of developing severe hypotension defined as an SBP or MBP decrease of more than 40% from baseline [15]. Also, arterial stiffness, evaluated by carotid-femoral pulse wave velocity, is significantly associated with the duration of PIH, defined as above [15]. This means that both factors, fluid status and arterial stiffness, could influence PIH. The exact mechanism by which these physiopathological pathways interact needs further investigation in the context of personalized medicine.
Administering large amounts of fluids during the induction period could result in hypervolaemia, which is harmful to vascular barrier competence [27]. Infusing fluids in a primarily normovolaemic circulation may lead to a breakdown of the endothelial surface layer [28], altering patient outcome. A more physiological strategy to prevent PIH is the use of vasopressor to re-establish blood pressure, fluids being a second-line strategy.
There is a high variability of PIH (5-99%), mainly due to the absence of an accepted definition of IOH [29]. Jor et al. [7] identified an incidence of PIH of 36.5%. Our results show a much higher incidence of PIH when using the same definition of PIH, 84.4%. The important difference between the PIH incidence is probably due to the frequency of blood pressure determination after induction, as we determined the blood pressure every minute and Jor et al. determined it only twice, at 5 and 10 minutes after induction.
Considering that, in the literature, there is strong evidence to support the relationship between IOH and increased postoperative morbidity and mortality after non-cardiac surgery [2, 30], we did not intend to quantify PIH effects on clinical outcome variables, as our study was designed to evaluate whether preoperative BIA assessment could identify patients at risk of PIH. Furthermore, although seve-ral studies have reported an association between intraoperative mean arterial blood pressure, especially relative decreases, with worse outcomes [31–34], we did not identify any relationship between BIA-derived parameters and MBP.
Strengths and limitations
Our study excluded patients with comorbidities recognized as risk factors for PIH. By protocolizing patient preoperative preparation, induction of anaes-thesia and monitoring during anaesthesia induction, we excluded confounders. We evaluated the decrease of blood pressure during induction of anaesthesia using multiple definitions for PIH for both SBP and MBP. Also, baseline blood pressure was measured outside the operating theatre. This is important because most studies evaluating IOH use the first blood pressure measured in the operating room as baseline blood pressure. This may reflect transient hypertension at arrival in the operating room, thus overestimating the severity of PIH.
There are multiple limitations of our study. We included a relatively small sample size of elective surgical patients from a single-centre unit, with a high incidence of known cancer disease. Our findings regarding the BIA values measured in this group of patients might not apply to other settings because all patients underwent surgery in a single university tertiary medical centre, treating the patients according to local clinical standards. Our findings need to be verified by larger or multi-centric studies.