Adjuvants have been administered in spinal anaes-thesia since the development of the technique. They prolong the duration of sensory and motor blockade, in addition to providing postoperative analgesia [1–3]. Clonidine is one of the main adjuvants used intrathecally in association with local anaesthetics. It acts by stimulating a2 receptors in the spinal cord, activating nociceptors, and reducing the sympathetic response, in addition to causing vasodilation. Its main side effect is the increased incidence of perioperative hypotension and bradycardia due to the autonomic imbalance caused by the potentiation of the sympathetic blockade due to clonidine [3].
Heart rate variability (HRV) was used to estimate autonomic nervous system activity, a technique already validated to indirectly measure autonomic control in different scenarios, including spinal anaesthesia. Linear methods were used in the low-frequency/high-frequency ratio (LF/HF) in the frequency domain and in non-linear methods in the chaos domain: Poincaré plot standard deviation (SD2/SD1), approximate entropy (ApEn), detrended fluctuation analysis (DFAa1 and DFAa2), and correlation dimension (D2) [4–6]. There is a difference in sensitivity between motor, sensory, and sympathetic fibres to local anaesthetics and clonidine.
This study aims to assess whether there is a difference between the recovery of motor and sympathetic function in patients who received spinal anaesthesia with clonidine as an adjuvant.
METHODS
The study was submitted to and approved by the Ethics Committee for Research on Human Beings (CEP) of the Instituto de Gestão Hospitalar e Saúde (ISGH). The clinical trial was registered in the Brazilian Registry of Clinical Trials (ReBEC), http://www.ensaiosclinicos.gov.br/, under number RBR-4Q53D6 and registered on 08/10/2018 under the title “Fractal and chaotic behavior of heart rate variability in subarachnoid anesthesia”. Written informed consent was obtained from all subjects, a legal surrogate, the parents, or legal guardians of minor subjects.
This is a randomised, double-blind clinical trial, with masking of patients and researchers involved. Allocation selection was performed by simple draw with envelopes. Diabetic and hypertensive patients using beta-blockers or calcium channel antagonists, conditions that may influence HRV and autonomic nervous system (ANS) measurements, were excluded. The study protocol considered the following as exclusion criteria: patients who used antihypertensive drugs with action on nerve conduction of myocardial fibres (b-blockers, calcium channel antagonists), chemical dependents, smokers, uncontrolled diabetics, and patients submitted to other types of surgical or anaesthetic procedures, technique, and change in surgical or anaesthetic management during the perioperative period.
The sample consisted of 64 patients, aged between 16 and 64 years, with physical status American Society of Anesthesiology (ASA) I and II and admitted for orthopaedic surgery under spinal anaesthesia. The patients were divided into 2 groups: group B (bupivacaine) and group C (bupivacaine + clonidine). HRV was measured for 10 minutes at 2 specific times. T1 was considered the measurement at rest; T2 was considered the moment of return of motor function in the post-anaesthesia care unit (PACU). Motor block recovery was considered when the patient reached a Bromage score of 2. The device used to collect the electrocardiographic signal was the POLAR V800® heart rate monitor. After acquiring the signal, the worksheet was manually filtered in Excel®, and the automatic filtering and analysis of the parameters was performed using the KUBIOS 3.0® software. SPSS® software was used for statistical analysis.
All patients received standard monitoring with ECG, pulse oximetry, and non-invasive assessment of blood pressure and temperature, initiated in the preparation before entering the operating room. The room temperature during preparation was maintained between 22 and 24°C, in the operating room between 18 and 22°C, and in the post-anaesthetic recovery room between 22 and 24°C. Humidity was recorded and ranged from 40 to 60%. Vital signs and anthropometric data were recorded upon arrival in the operating room.
After the first collection of heart rate variability at rest, one of the researchers was responsible for selecting one sealed envelope, which contained the writing “with clonidine” or “without clonidine”, and preparing the syringe with the anaesthetic solution contained in the selected envelope; 20 mg of hyperbaric bupivacaine + 75 mg of clonidine for the group drawn with the term clonidine and 20 mg of hyperbaric bupivacaine + 0.5 mL of distilled water for the group drawn with the term bupivacaine. All filled syringes had a volume of 4.5 mL. The anaesthesiologist who performed the procedure was unaware of the solution to be administered. The administration of adjuvants can change the baricity of the solution, increasing the duration of anaesthesia [6].
The initial hypothesis of this study considers that the sympathetic component of spinal anaesthesia lasts longer than the motor component when clonidine is used as an adjuvant in spinal anaesthesia.
RESULTS
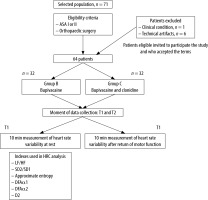
The patient recruitment flowchart is shown in Figure 1. The final sample included 64 of 71 eligible patients. Seven patients were excluded due to excess artifacts in the sample after collection or due to changes in anaesthetic management during the perioperative period. Statistical analysis of group homogeneity predicted the sample size, considering a sampling error of 10% and a significance level of 95%, which was calculated as 62 participants. The χ2 test with Yates’ correction was used to assess gender distribution between groups, with χ2 = 0.074 with one degree of freedom and P = 0.7857, showing statistical similarity between groups.
Student’s unpaired t-test was used to assess differences in means in relation to age, height, weight, heart rate and systolic blood pressure, with no statistical difference between groups (Table 1). Student’s unpaired t-test was used to compare the LF/HF, SD2/SD1, ApEn, DFAa1, DFAa2, and D2 indices in the 2 groups at rest and at the time of motor function recovery, and Student’s paired t-test was used to compare T1 and T2 times in each group individually. In the bupivacaine group, there was no statistically significant difference between the 2 measurements. In the clonidine group, there was a significant difference only in the approximate entropy index, where a p value of 0.0124 was obtained (Tables 2 and 3).
TABLE 1
Comparison between the average of the clonidine and bupivacaine groups of the following parameters: age, height, weight, and heart rate, using the Student’s t-test at T1
TABLE 2
Comparison between the means and standard deviations of the indices at times evaluated in the clonidine group
TABLE 3
Comparison between the means and standard deviations of the indices at times evaluated in the bupivacaine group
[i] LF/HF – low frequency/high frequency, SD2/SD1 – represents the ratio of long-term standard deviation to instantaneous standard deviation, ApEN – approximate entropy, DFAα1 – is refined analysis of short-range trends, DFAα2 – is the refined analysis of long-range trends, D2 –correlation dimension
DISCUSSION
Spinal anaesthesia is an established, safe, and relatively simple technique, the main complications being hypotension and bradycardia resulting from the sympathetic blockade inherent to the technique. Administration of local anaesthetics into the intrathecal space causes sensory, motor, and sympathetic blockade with relatively similar onset of action and duration. Clonidine has been administered in association with local anaesthetics with the main objective of prolonging the duration of surgical anaesthesia and providing better postoperative analgesia [3, 7].
There is a difference between the half-life of clonidine (1.1–1.3 h) and that of bupivacaine (2–3 h), with a synergistic action that prolongs the duration of anaesthesia by approximately 50 minutes. Bupivacaine works by binding and inactivating sodium channels in nerve fibres in the spinal cord. Clonidine, in turn, acts by binding mainly to a2 adrenergic and potassium channels, potentiating the effects of bupivacaine. Thus, due to the difference in half-life and sites of action of clonidine and bupivacaine, the persistence of sympathetic blockade after recovery from motor blockade was questioned when clonidine is used as an adjuvant in spinal anaesthesia [3, 8–13]. Furthermore, the pharmacokinetic changes that occur between bupivacaine and clonidine administered intrathecally are not fully understood.
The evaluation of motor block recovery in spinal anaesthesia is already well defined in clinical practice by the Bromage scale, being one of the criteria for discharge from the post-anaesthesia care unit. Sympathetic blockade can be assessed using heart rate variability measurements, with several studies published in different clinical contexts, including perioperative and spinal anaesthesia [14–20]; however, we found no studies evaluating HRV in spinal anaesthesia when clonidine is used as an adjuvant.
Heart rate variability can be assessed by linear and non-linear methods in the chaos domain. In this study, both methods were used, but linear methods apparently do not reflect the complexity of interactions between the various organ systems in the surgical setting. Time series extracted from biological signals show chaotic and complex behaviour, making it impossible to characterize their nature with a single analysis method [22].
In the analysis of heart rate variability in the chaos domain, the association of 2 or 3 methods reveals information that is more representative of natural events [4, 11], allowing estimation of the complex, regular, or random behaviour of the time series, bringing to light information and variables not shown by traditional methods [13]. Despite this, the importance and clinical applicability of these new methods have yet to be defined.
In the group that received only bupivacaine, we found similar values of LF/HF, SD2/SD1, ApEn, DFA, and D2 between T2 and T1, with no statistically significant difference, indicating concomitant recovery of the return of motor and sympathetic functions (Table 2). Backlund et al. [20], in a randomized clinical trial with 40 patients at high risk of ischaemic heart disease, found a reduction in the power spectrum for up to 3 postoperative days. However, they observed that sympathovagal balance, as measured by the LF/HF ratio, is better maintained during spinal anaesthesia when compared to general anaesthesia.
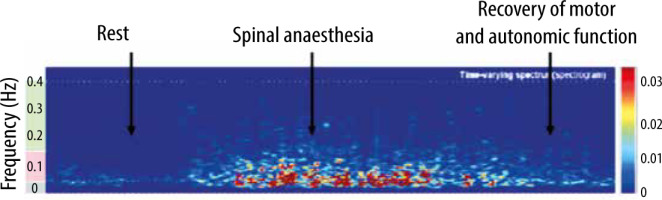
In the clonidine group, there was a statistically significant difference between T2 and T1 only in approximate entropy, with P = 0.0124. The other indices showed no difference between T2 and T1. However, as already mentioned, the variation of only one of the HRV indices to the detriment of the others is not significant. Therefore, we consider that there was no difference between the evaluated moments, and the return of motor function occurred concomitantly with the return of sympathetic function (Figure 2).
FIGURE 2
Spectral analysis of one of the patients in the clonidine group during the entire perioperative period of rest at PACU discharge, showing the simultaneous return of autonomic and motor function
Some factors related to the collection environment may interfere with the study result, such as the emotional state of the patient, the noise present in the operating room, and the level of surgical aggression, which varies between different procedures. Furthermore, we did not identify any studies evaluating HRV in spinal anaesthesia with intrathecal clonidine as an adjunct. More studies need to be carried out to analyse the listed hypotheses.
CONCLUSIONS
Findings suggest simultaneous recovery of motor and sympathetic functions after spinal anaesthesia when clonidine is used as an adjunct.
FUTURE PERSPECTIVES
Heart rate variability is promising in the field of perioperative medicine. Several tools are being developed for use in anaesthesiology based on HRV. Some are already available on the market and measure the level of perioperative pain using these parameters in association with other biological signs.