Atopic dermatitis (AD) is a chronic inflammatory skin disease. The manifestations of AD are eczematous lesions, persistent itch, and recurrent course. AD mainly occurs in the paediatric population, but adults can be also affected [1]. AD is associated with other inflammatory diseases, such as asthma and allergic rhinitis [2]. Besides inflammatory diseases, the relationship between AD and fractures is shown. Current investigations have found that AD (or eczema) is strongly associated with fractures, both in adults and children [3]. However, in a single study, the statistical power may be limited due to the inappropriate design, small sample size, and inclusion of certain participants only. AD has a great influence on the physical and mental health of patients, meanwhile fracture is associated with high morbidity and mortality. As a result, a comprehensive assessment of fracture risks in AD patients is in need. In this study, we evaluated the risks through meta-analysis and trial sequential analysis.
We searched six databases to obtain publications. The selection was based on the inclusion and exclusion criteria. After inclusion, the study quality was assessed by Newcastle-Ottawa Scale (NOS). The total score is 9, when a study’s score is ≥ 6, high quality was considered. The risk ratio (RR) was applied to evaluate the risk. According to the between-study heterogeneity, a fixed or random effects model could be chosen. In the Q-statistical test and I2 test, if p-value is > 0.10 and I2 is < 50%, the heterogeneity was not significant, the fixed-effects model was selected, otherwise the random model was used. Sensitivity was analyzed to test the impact of an individual study. Funnel plots were performed to estimate the publication bias. In each comparison, p-value < 0.05 was defined as statistical significance. Trial sequential analysis (TSA) was conducted to evaluate if the case numbers were enough/sufficient. The 5% risk of type I error (false positive) and 30% risk of type II error (false negative) were set.
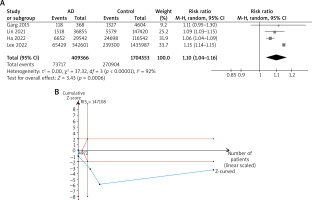
Based on the inclusion and exclusion criteria, four studies were included for meta-analysis [3–6]. The sources of the data were all national surveys or databases. One study investigated patients in the US, one in Taiwan of China, and two in Korea. The included studies were all of high quality. The detailed information of the included studies was shown in Table 1. A total of 409366 AD patients and 1704553 control subjects were included. The between-study heterogeneity was significant (I2 = 92%, p < 0.001), so the random effect model was selected for the analysis. The pooled data suggest that the risks of bone fractures were elevated in AD patients, with RR = 1.10 (95% CI: 1.04–1.16). In trial sequential analysis, the Z-curve crossed the required information line (RIS), which indicated that a total of 147108 cases need to be included. Our study included 2113919 cases (409366+1704553) in total. The TSA result suggested that the case number is sufficient to draw a reliable conclusion. The results of meta-analysis and TSA were shown in Figure 1. From the sensitivity analysis, the result of meta-analysis was robust. When each study was ignored one by one, the significance was still shown.
Table 1
Characteristics of included studies
Our study evaluated risks of bone fracture in AD patients and increased risks of fractures in AD patients were shown. The findings of this study were similar with several previous publications. Inflammation plays an important role in the mechanism of AD. Multiple proinflammatory molecules and cytokines, including interleukin (IL)-1, IL-4, IL-17, IL-31, and tumor necrosis factor-α (TNF-α), contribute to the occurrence of the lesions. Meanwhile, those factors also participate in the stimulation of osteoclast and bone resorption, which will lead to the poor bone health and fractures [3]. On the other hand, oral and topical corticosteroids, disease-modifying anti-rheumatic drugs (DMARDs), and phototherapy treatment are main treatments for AD patients. However, the above methods were all considered as risk factors for fractures [3, 7]. Generally, those factors explain the relationship between AD and bone health, however, more basic research is still needed to explore the mechanisms of AD and fracture.
Previously, a meta-analysis study to evaluate the bone mineral density and fracture risk in AD patients was published [8]. Different from this study, our analysis included more studies, and we used the total number of fractures for comparison, while the risks of different parts were included for the comparison in the previous study. Besides, we further performed trial sequential analysis, and we found that the current case number is sufficient to draw a reliable conclusion.
There were still some limitations in our study. Firstly, in general populations, the fracture risk was increased with age, and females are at higher risk for fractures than males [8], however, due to the format of the included data, we could not analyse the fracture risk based on different groups. Secondly, the sources of data in the included studies were all national surveys or databases. The number of cases could be guaranteed, nevertheless, the lack of clinical-based case-control or cohort studies limited our further analysis.
In conclusion, compared with non-AD control subjects, AD patients were associated with elevated risks of bone fractures. For clinicians, AD-related fractures should be noticed. Further basic and clinical studies are still in need to verify the relationship between AD and fracture.