Laparoscopic surgery is increasingly popular and is slowly replacing conventional open surgery because it offers greater benefit to patients and health care practitioners. The overall risk of complications during laparoscopic surgery is lower than during laparotomy. Laparoscopic hysterectomy, compared to open vaginal hysterectomy, reduces post-operative pain, reduces post-operative anal-gesic requirements, and shortens the duration of hospital admission [1]. Traditionally, pneumoperitoneum was created at 15 mmHg [2]. High intra-abdominal pressure (IAP) created during laparoscopic surgery can affect cardiovascular, pulmonary, and renal physiology. Besides the risk of post-operative nausea and vomiting, it is also stated that the pneumoperitoneum created during laparoscopic surgery is an important factor in the cause of post-operative shoulder pain [3]. Insufflation of intraabdominal carbon dioxide may cause post-operative shoulder pain in up to 70% in some studies of gynaecologic laparoscopic surgery [4].
The usage of a lower-pressure pneumoperitoneum might decrease post-operative pain, decrease post-operative shoulder tip pain, and reduce the risk of laparoscopic-related complications [5, 6]. Many studies used lower insufflation of IAP as an intraoperative intervention to reduce the complication [6, 7]. However, a lower IAP may worsen surgical space and increase the risk of conversion to open surgery. Numerous studies also have shown that deep neuromuscular block improves surgical conditions in different types of laparoscopic surgery, including laparoscopic gynaecology surgery and robotic-assisted laparoscopic surgery, allowing the use of lower-pressure pneumoperitoneum [8, 9]. However, there is a lot of heterogeneity in previous studies to compare the superiority of deep neuromuscular block over moderate neuromuscular block. There is also a lack of study in local clinical healthcare settings pertaining to this subject. Therefore, further studies are required to evaluate the benefit of deep neuromuscular block.
METHODS
Study design, respondents, and randomisation
This randomised control study was conducted in a university-affiliated hospital, a tertiary referral centre for gynaecology cases covering east Malaysia. The study protocol was submitted, evaluated, and approved for execution by Human Research and Ethics USM protocol code: USM/JEPeM/20080410. ASA I and ASA II patients above 18 years old who underwent laparoscopic gynaecology surgery were included. Informed consent was obtained. Exclusion criteria include allergy to study drugs (rocuronium, sugammadex), severe cardiac and respiratory disease (reactive airway disease, upper respiratory tract infection), neurological or neuromuscular disease (epilepsy, family history and history of malignant hyperthermia, etc.), pregnancy, and morbid obesity with body mass index more than 35 kg m–2. Patients were randomised using computer-generated simple randomisation – Random Allocation software version 2.0 – into two groups: either deep or moderate neuromuscular block. The randomisation sequence was kept in an envelope and was given to the anaesthesiologist in charge upon starting the cases. The patient was assessed preoperatively and provided informed consent. As per standard monitoring, non-invasive blood pressure, mean arterial pressure, heart rate, pulse oximeter, electrocardiogram, and oxygen saturation were monitored. In addition, TOF-Watch® SX-acceleromyograph was applied at the adductor pollicis muscle and calibrated before neuromuscular block commencement to monitor response and degree of neuromuscular block. Gene-ral anaesthesia was commenced in both groups with bolus intravenous fentanyl 100 µg, intravenous propofol 2 mg kg–1, and intravenous rocuronium 0.6 mg kg–1 as an induction agent. The patient was intubated at train-of-four (TOF) 0. Anaesthesia was maintained with an inhalational anaesthetic agent at the minimum alveolar concentration (MAC) of 1.0. Intermittent bolus rocuronium 0.2 mg kg–1 was given in moderate block to maintain post-tetanic count (PTC) > 1, TOF 0–2, whereas the patient in the deep block was infused with intravenous rocuronium infusion at 8–12 µg kg–1 min–1 (0.48–0.72 mg kg–1 h–1) to maintain PTC 0–1. Intravenous paracetamol 1 g was given after induction with intravenous morphine 0.05 mg kg–1. Initial pneumoperitoneum was created at 8 mmHg. The surgical procedure was started at an IAP of 8 mmHg. The surgeon was allowed to change IAP to 10–14 mmHg if they decided that the visual field was unsatisfactory for the operation. At the end of the operation, the surgical condition was rated based on a 4-point scale (1 = excellent, 2 = good, 3 = acceptable, 4 = poor). To prevent the surgeon from being distracted, assessment was performed after surgery. The possibility of recall bias is also mini-mal because assessment of the surgical condition was done immediately after the surgery. The infusion drug was discontinued, and the neuro-muscular drug was reversed with sugammadex based on TOF count for both groups. IAP levels were recorded to enable any subsequent analysis. Intravenous dexamethasone and ondansetron were given as anti-emetics. Post-operative pain and shoulder tip pain were evaluated immediately in the post-anaesthesia care unit – 0, 30 minutes, and 24 hours post-operatively. Fentanyl was injected intravenously in the post-anaesthesia care unit for rescue analgesia as needed. The pain was measured using an 11-point numerical rating scale (NRS), ranging from 0 (no pain) to 10 (most pain imaginable). Both surgeon and patient were blinded in this study.
Measurement of primary and secondary outcomes
This study’s primary outcome is the difference in the rate of increasing IAP between groups. The highest IAP used has also been analysed. Secondary outcomes include quality of surgical space condition (1: excellent, 2: good but not optimum, 3: poor but acceptable, 4: unacceptable), abdominal pain score, and shoulder tip pain at recovery bay-time 0, 30 minutes, and 24 hours.
Sample size
PS Power and Sample Size Calculations Version 3.0 (January 2009 Copyright © 1997–2009 by William D. Dupont and Walton D. Plummer) was used to calculate the sample size.
Primary outcome calculation was based on a previous study by Dubois et al. [10] in laparoscopic hysterectomy in which the probability of an outcome for excellent and good surgical condition was 0.6 in control subjects (P0), and the probability of outcome in study subjects (P1) was 0.9. For the secondary outcome, based on Martini et al. [11], the true difference in surgical space quality between the group with moderate NMB (control) and the deep-NMB group is 0.5, with a standard deviation of 0.4. The true difference in pain score between the moderate (control) and deep groups is 1, with a standard deviation of 1.4 [12]. This study used a 0.05 significance level and a power of 80%. With a ratio of 1 : 1 between the 2 groups, including 10% dropout, we estimate 70 samples, 35 in each group, to reject all the null hypotheses.
Statistical analysis
The χ2 test was used to compare the proportion of the rate of increasing IAP between the 2 groups. The mean highest IAP and surgical space condition between the 2 groups were analysed using an independent t-test. Two-way repeated measure ANOVA was used to determine whether there was a significant difference in deep NMB and moderate NMB in abdominal pain score and shoulder tip pain score measured at 3 time points (baseline, post-intervention 30 minutes, and post-intervention 24 hours). The normality assumption, covariance homogeneity, and compound symmetry of the model were all verified. 0.05 was used as the significance level. All data obtained were analysed using SPSS version 26.
RESULTS
A total of 70 patients were recruited for the study. They were randomised equally into 2 groups: group 1 – deep NMB, and group 2 – moderate NMB. There was no dropout in this study.
Demographic and clinical characteristic
The mean age of patients in moderate NMB was 33.7 (± 6.5) years, whereas in moderate NMB it was 32.2 (± 7.7) years. Mean BMI was 25.8 (± 4.0) in deep NMB and 25.5 (± 3.2) in moderate NMB. Mainly ASA I patients were recruited in this study. Most operations were laparoscopic cystectomy. Detailed descriptions are shown in Table 1.
TABLE 1
Demographics
Rate of increasing intraabdominal pressure
There is a significant difference in the mean highest IAP used between groups, with a P-value of 0.001. The mean highest IAP use in the deep-NMB group was slightly lower at 10.31 (± 1.39) mmHg, whereas it was 11.54 (± 1.69) mmHg in the moderate-NMB group (Table 2).
TABLE 2
Rate of increasing intraabdominal pressure between deep and moderate neuromuscular block groups
| Group | Surgery completed at intraabdominal pressure 8 mmHg | χ2 stat (df) | P-value* | |
|---|---|---|---|---|
| No | Yes | |||
| Moderate NMB | 32 (45.7) | 3 (4.3) | 1.87 (1) | 0.172 |
| Deep NMB | 28 (40.0) | 7 (10.0) | ||
In the deep-NMB group, 7 patients (20%) completed surgery at IAP 8 mmHg, whereas 3 patients (8%) in moderated neuromuscular block completed surgery at IAP 8 mmHg. There is no statistically significant difference in the rate of increasing IAP in the deep and moderate neuromuscular blocks, with a P-value of 0.172 using the χ2 test (Table 3).
Surgical space condition
The mean surgical space condition at the deep NMB is slightly better at 2.4 (± 0.7), and 3.2 (± 0.66) at the moderate NMB. Using the independent t-test, surgical space condition in the deep NMB is statistically significant compared to the moderate NMB, with a P-value < 0.005, as shown in Table 4.
Post-operative pain score
Abdominal pain score
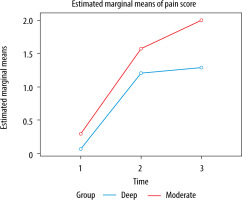
Independent t-test analysis showed there was a significant mean difference in abdominal pain between the deep NMB and moderate NMB groups recorded at time 0 (P = 0.011) and 24 hours (P < 0.001), but there was no significant mean difference at 30 minutes (P = 0.053) (Table 5). Further statistical analysis using two-way repeated measure ANOVA shows that there was a significant difference in mean abdominal pain score between the deep-NMB and moderate-NMB groups with regard to time (F (1, 68) = 18.863; P < 0.001). Mauchly’s test for sphericity indicated that the assumption was met (χ2 = 1.728, df = 2, P = 0.421). There was an overall significant change in abdominal pain score over time (F (2, 136) = 139.93; P < 0.001), but there was also a significant interaction between group and time (F (2, 136) = 3.53; P = 0.032). Hence, the analysis was stratified based on the group where one-way repeated measure ANOVA was used. Among patients with deep NMB, there was a significant effect of time on the abdominal pain score (Wilks’ Lambda = 0.187, F (2, 33) = 71.70, P < 0.001). Multiple pairwise comparisons with Bonferroni correction showed that the difference in abdominal pain score between each time point was significant except for 30 minutes to 24 hours. As for the moderate NMB, there was a significant effect of time on the abdominal pain score (Wilks’ Lambda = 0.153, F (2, 33) = 91.61, P < 0.001). Multiple pairwise comparisons with Bonferroni correction showed that the difference in abdominal pain score between each time point was significant (Table 6, Figure 1).
TABLE 5
Abdominal pain score between deep NMB and moderate NMB
TABLE 6
Multiple comparison of mean abdominal pain scores between deep NMB and moderate NMB over time
Shoulder tip pain score
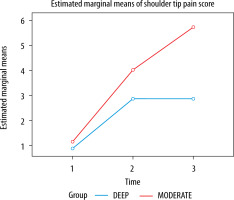
Independent t-test analysis showed a significant mean difference in shoulder tip pain between deep NMB and moderate NMB groups recorded at 24 hours. However, there was no significant mean difference at time 0 (P = 0.695) and 30 minutes (P = 0.350) (Table 7). The data was further analysed using repeated measure ANOVA. There was no significant difference in mean shoulder tip pain score between the deep-NMB and moderate-NMB groups with regard to time (F (1, 68) = 3.382; P = 0.07). Mauchly’s test for sphericity indicated that the assumption was met (χ2 = 1.299, df = 2, P = 0.522). There was an overall significant change in shoulder tip pain score over time (F (2, 136) = 13.827; P < 0.001), but there was no significant interaction between group and time (F (1, 136) = 2.04; P = 0.134). Multiple pairwise comparisons demonstrated a statistically significant mean difference in shoulder tip pain score for moderate NMB from 0 to 30 minutes and from 0 to 24 hours. Otherwise, there was no significant mean difference across time for deep NMB (Table 8, Figure 2).
TABLE 7
Shoulder tip pain score between deep NMB and moderate NMB
TABLE 8
Multiple comparison on mean shoulder tip pain score between deep NMB and moderate NMB over time
DISCUSSION
All numerical variables in this study are normally distributed because the study population consisted of women in their reproductive years. This is consistent with a previous study involving gynaecological surgery [9]. The advantage of using the mean value as an estimator in a normally distributed population is that it considers all values when calculating the average.
The deep-NMB group (mean: 10.31 (± 1.39) mmHg) requires significantly less pneumoperitoneum than the moderate-NMB group (mean: 11.54 (± 1.69) mmHg) to complete the surgery. This is lower than the standard pressure used in laparoscopic surgery, which is 12 mmHg [13, 14]. In this study, there is no significant difference in the rate of increasing IAP between the 2 groups, in which the majority need an IAP slightly higher than 8 mmHg to complete the surgery, in contrast to a previous study in laparoscopic cholecystectomy where the rate of IAP is higher in the moderate neuromuscular block [8]. The limitation of this study is that while evaluating the mean highest IAP use between 2 group, the surgeon was allowed to change IAP to 10–14 mmHg if they decide that the visual field was unsatisfactory for the operation, which may create an additional confounding factor introduced by the surgeon into the IAP. It has been confirmed that usage of higher IAP in laparoscopic surgery led to many unfavourable side effects such as compression of inferior vena cava and aorta aortic compression, reduction in splanchnic blood flow and renal blood flow, and diaphragmatic splinting [15]. Further study can be done to investigate the possible reduction of side effects in low-pressure pneumoperitoneum.
The mean surgical space condition in deep NMB is better at a mean of 2.4 (± 0.7) compared to a mean of 3.2 (± 0.6) in moderate NMB (95% CI: 0.47–1.13, P < 0.05). Although most of the surgery cannot be completed at the very low IAP of 8 mmHg and the rate of increasing IAP is statistically insignificant, this study demonstrated that deep NMB reduced the IAP requirement in laparoscopic surgery without interfering with the surgical space condition. In a previous study, Dubois et al. [10] also revealed that deep moderate neuromuscular block decreased the incidence of unacceptable surgical conditions at pneumoperitoneum 13 mmHg using a 4-point surgical field scale. Another study using a 4-point surgical rating scale comparing deep and moderate NMB at different IAP also demonstrated that deep NMB improves surgical space by a mean of 0.33 cm (95% CI: 0.07–0.59, P = 0.01) at 12 mmHg but only improved by a mean of 0.3 cm at 8 mmHg [9]. Recent study in 2022 by Nikolaos et al. [16] also showed that there is no statistically significant improvement in operative visual field and handling of small and large bowel between moderate and deep NMB. Surgical rating scales enable the surgeon to quantify the surgical space condition, especially during research works in laparoscopic surgery. The limitation of this study is that we are using a 4-point scale, but scales with 5–7 items have better test–retest reliability, internal consistency, and discriminating power than short scales (2–4 item points) or very big scales (> 10 item points). Besides, quality, methodology, and results reporting in the surgical condition rating scales are all inconsistent. To improve the quality and repeatability of future studies, it is necessary to consistently employ high-quality surgical rating scales [17]. Nevertheless, the same systematic review also observed that 4-point rating scales are predominantly used in laparoscopic gynaecological surgery [17].
This study shows a significant difference in mean pain score between deep NMB and moderate NMB. The mean pain score in deep NMB is lower than in moderate NMB. There is an increase in pain score over time. This is possibly because intraoperative analgesics were standardised and still had the effect when the pain score was assessed on arrival in recovery at time 0. Across the reviewed literature, post-operative pain was lesser when lower pressure was used during laparoscopic surgery. A total of 150 patients were included in the randomised, controlled prospective experiment, which was conducted at a tertiary education hospital and involved gynaecological laparoscopy with 3 different abdominal insufflation pressures at low (8 mmHg), standard (12 mmHg), and high (15 mmHg), and which demonstrated that low insufflation pressure reduces pain as compared to standard and high insufflation pressure. However, this study shows that low insufflation pressure, on the other hand, may lead to prolonged operation times and higher bleeding [14]. This study did not use deep NMB to assist in low-pressure pneumoperitoneum. In spine surgery, Kang et al. [18] investigated whether deep NMB could reduce surgical haemorrhage compared to mild NMB (2 or 3 spinal levels, in a prone position). When compared to mild NMB, deep NMB considerably reduced intra-operative surgical haemorrhage. Additionally, a meta-analysis done by Bruintjes et al. [19] in 2017 combining 5 studies showed that there is lesser post-operative pain during the first hour of surgery in deep NMB (MD = 0.52 [95% CI: –0.71 to 0.32]) with 0% heterogeneity between studies. Interestingly, fewer trials reported post-opera-tive pain after 24 hours, so meta-analysis of this outcome were not done [19]. On the contrary, a newer meta-analysis in 2020 by Yiyong et al. [20] demonstrated that there was no significant reduction in early post-operative pain in the low IAP and deep NMB (MD = 0.14 [95% CI: 0.51–0.23]). The study-to-study heterogeneity was 0%. Similarly, the study could not conduct any post-operative pain meta-analyses after 24 hours because of limited trials reported on this outcome. Therefore, this study was done in response to the limited study that examined 24-hour pain scores in deep NMB.
There was no significant difference in shoulder tip pain in deep NMB compared to moderate NMB in this study. However, the change in shoulder tip pain score with time was significant (F (2, 136) = 13.827, P = 0.001), but there was no significant interaction between the groups and time points (F (1, 136) = 2.04, P = 0.134). This is contrary to the study done by Madsen et al. [3], where shoulder tip pain after laparoscopic hysterectomy was lesser in the deep-NMB and low-pressure (8 mmHg) pneumoperitoneum group compared to the moderate-NMB and standard-pressure pneumoperitoneum groups (12 mmHg). Another study by Koo et al. [21] in 2016 demonstrated that there were no differences in post-operative pain and shoulder tip pain between deep NMB and moderate NMB at 30 minutes after laparoscopic cholecystectomy, but pain score at 24 hours post-surgery was lower in deep NMB (P = 0.048 and 0.02, respectively). However, they analysed the pain score at different times using an independent t-test. So, the advantages of this study were statistically superior results because the test was done using two-way repeated measure ANOVA, which makes an experiment more efficient and reduces variability. This helps keep the results’ validity higher while allowing for smaller subject groups than normal. The limitation of this study was that there was no standard post-operative analgesics protocol from 30 minutes to 24 hours. Thus, further study can be done with a standard post-operative analgesic protocol to overcome this limitation.
CONCLUSIONS
There was no difference in the rate of increasing IAP between the 2 groups, but deep NMB required less pneumoperitoneum to complete the surgery. Thus, further study needs to be done to determine the optimal IAP requirement in deep neuromuscular block-assisted laparoscopic surgery. The surgical condition is better in deep NMB. Post-operative pain was significantly lower in deep neuromuscular block within 24 hours post-surgery, but there was no significant difference in shoulder tip pain observed in both groups.