The Impella (Abiomed) is a mechanical circulatory support device which augments cardiac output, but may also unload a left ventricle during venoarterial extracorporeal membrane oxygenation (ECMO) [1]. However, the Impella requires an access to a large artery and this may be problematic in a severe peripheral arterial disease. The presented case demonstrates how to insert and remove the Impella CP via a subclavian approach without surgical cutting.
A 69-year-old man was admitted due to an ambulatory myocardial infarction (i.e. he presented a decreasing level of cardiac enzymes and a history of chest pain several days before) and heart failure symptoms with the left ventricular ejection fraction (LVEF) 20%. He also suffered from chronic obstructive pulmonary disease, neurofibromatosis (i.e. von Recklinghausen’s disease), prostate cancer and depression. Coronary angiography revealed chronic total occlusion of the left anterior descending artery (without myocardium viability in a subsequent dobutamine echocardiography), significant stenoses (up to 80–90%) in the proximal, medial and distal portion of the left circumflex coronary artery (Figure 1 A), and a hypoplastic right coronary artery. After examinations, the Heart Team qualified the patient for percutaneous coronary intervention (PCI) of the left circumflex coronary artery. Because of the high risk, PCI had to be performed with the Impella; however, the ultrasound examination and multi-slice computed tomography revealed an occlusion of the right iliac artery, a significant (80%) calcified stenosis of the left iliac artery, and a critical stenosis of the left subclavian artery. Due to long calcified lesions within iliac arteries, according to the Heart Team opinion, the best option was insertion of the Impella via a subclavian approach and PCI via a left femoral access.
Figure 1
Percutaneous coronary intervention with Impella CP insertion via a subclavian approach without surgical cutting. A – Left coronary angiography shows an occlusion of the left anterior descending artery (LAD) and multi-level stenoses within the circumflex artery (the cranial left anterior oblique projection). B – Angiography of the right subclavian and axillary arteries, and a presumable puncture site is depicted. C – A peripheral balloon (inserted via radial access) is inflated at the puncture site determined with the help of ultrasound imaging. The puncture should be done at a shallow angulation to facilitate insertion of a large sheath (the tip of the needle is depicted). In this technique, the intention is to puncture the balloon, then a guidewire is inserted into the balloon, and they both are pushed to the aorta (it is easy because the puncture causes deflation of the balloon) – the balloon should be replaced with a new one which will serve as a hemostatic measure during following maneuvers. However, it may happen that only the artery is punctured (without puncturing the balloon), then the guidewire is inserted in a standard way but the balloon should be simultaneously deflated. D – When deploying Proglide closure devices and placing a 14F introducer, the peripheral balloon should be inflated in the proximal portion of the subclavian artery to prevent bleeding from the access site. Of note, a 0.035" (260 cm) guidewire, inserted via the radial artery to the aorta, should be left throughout the whole procedure for safety reasons
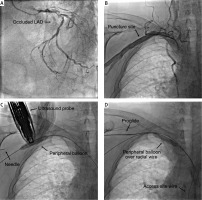
Figure 1 E
E – The left circumflex coronary artery after PCI with rotational atherectomy and implantation of five drug-eluting stents is presented. F – The peripheral balloon (inserted via radial access) should be inflated at the puncture site during removal of the 14F introducer and when sealing the vessel with Proglide sutures. Importantly, before retracting the 14F introducer, a safety stiff guidewire should be placed which may be used to deliver other Proglides or AngioSeal in the case of insufficient hemostasis. G – Angiography performed via the radial access shows a good hemostatic effect (such angiography may be done by using the inner lumen of the over-the-wire peripheral balloon). H – The access site after the procedure is shown
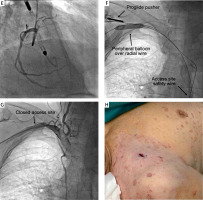
To place the Impella without surgical cutting, a 7F Glidesheath Slender Introducer (Terumo) was placed into the right radial artery and angiography was performed to reveal the anatomy of the subclavian and axillary arteries (Figure 1 B). A 0.035" (260 cm) guidewire was inserted into the aorta and an over-the-wire 9/40 mm peripheral balloon was positioned at the puncture site which was determined in the ultrasound imaging several centimeters below the right clavicula. The arterial puncture was guided by ultrasound and fluoroscopy and was performed on the fully inflated peripheral balloon – the balloon stabilized the vessel position and prevented squeezing of the vessel and an unintentional puncture of the opposite arterial wall which might result in hematoma (Figure 1 C). Then, a 6F sheath was placed and the access site was dilated to create a space for the 14F introducer (i.e. the Impella peel-away introducer). Three Proglide closure devices (Abbott Vascular) were deployed to ensure effective closure of the puncture site, and a 0.035" (150 cm) stiff guidewire was inserted which was used to deliver the 14F peel-away introducer. During exchanging all these devices, the peripheral balloon was inflated within the subclavian artery to prevent bleeding (Figure 1 D). After placing the 14F introducer, the Impella CP was installed in a standard way, and PCI with rotational atherectomy and drug-eluting stents implantation was performed (Figure 1 E). The Impella was removed immediately after the coronary intervention, and then a 0.035" stiff guidewire was inserted through the 14F introducer for safety reasons. Via the radial access, a peripheral balloon was placed and inflated at the puncture site to prevent bleeding during the 14F introducer removal (Figure 1 F). Finally, the vessel was closed with Proglide devices, and an 8F AngioSeal (Terumo) was placed to eliminate a residual leak. The angiography confirmed a good hemostatic effect (Figures 1 G, H). After PCI, the patient’s condition improved and LVEF increased to 38%.
In the described technique, both the Impella CP and peripheral balloons for hemostasis were delivered through a single extremity (i.e. the right upper one). However, other operators insert peripheral balloons for hemostasis by using another limb (usually through a femoral artery) [2, 3]. Thus, the presented technique is simpler and feasible even in the case where a second limb access is not possible. Moreover, it may be potentially utilized in a single access technique where no other peripheral access is necessary [4].








