There is a narrow safe range of endotracheal intubation depth for paediatric patients, particularly small babies such as neonates and premature infants. Various calculation formulas have long been proposed for the endotracheal tube (ETT) insertion length [1–4]. However, they were all formulas for estimating the ETT insertion depth at the mouth corners or nasal wings, although the anatomy of the oral cavity, i.e. the distance from the vocal cords to the mouth corners or nasal wings, may vary among patients. In addition, the ETT insertion depth may be too deep in some cases when these formulas are applied to neonates and infants [5]. Therefore, in our previous study [6], we focused on the ETT insertion length at the vocal-cord level, because the effects of individual differences in oral and nasal anatomy need not be considered, and the vocal cords are always visualized in all cases during laryngoscopy by tracheal intubation. The previous study aimed at defining the distance between the vocal cords and carina tracheae as tracheal length involving 425 and 335 cardiac paediatric patients in Germany and Japan, respectively, and revealed that the tracheal length in cardiac paediatric patients ranged from 6 to 10% of the body height in Germany and from 7 to 11% in Japan, thus revealing ethnic differences in tracheal length and in the ideal depth of endotracheal intubation at the vocal-cord level [6]. The aim of the current study was to determine whether the tracheal length differs between cardiac and non-cardiac paediatric patients and whether the results can be generalised to adult patients, in order to provide additional information to our pre-vious study [6].
METHODS
Study protocol and patients
This study was approved by the Ethics Committee of Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan (registration number: 2019-0362), and was registered with the UMIN Clinical Trials Registry (registration number: UMIN000045033). Written informed consent for general anaesthesia, including endotracheal intubation, was obtained from the patients undergoing surgery or their parents or guardians.
The study was conducted in two stages at Niiga- ta University Medical and Dental Hospital (Niigata, Japan). The first stage was a retrospective observational evaluation to compare the tracheal length between cardiac and non-cardiac paediatric patients. The second stage was a prospective validation including four groups: paediatric patients with congenital heart diseases who underwent cardiovascular surgery, paediatric patients without congenital heart diseases who underwent non-cardiac surgery, adult patients who underwent cardiac surgery, and adult patients who underwent non-cardiac surgery.
First stage: retrospective observational evaluation to compare the tracheal length between cardiac and non-cardiac paediatric patients
The first stage of the study included 335 paediatric patients with congenital heart diseases who underwent cardiac surgery and 275 paediatric patients without congenital heart diseases who underwent non-cardiac surgery between April 2010 and March 2020 at Niigata University Medical and Dental Hospital. Our previous study revealed that the tracheal length is significantly longer in the standing position than in the supine position and confirmed the validity of tracheal length measurements using chest radiographs taken in the supine position, that is, the intraoperative position [6]. Therefore, we included patients whose vocal cords were visible on preoperative chest radiographs taken in the supine position. The distance between the vocal cords and carina tracheae was defined as the tracheal length, which was measured on chest radiographs using the Picture Archiving Communication System (Figure 1). All tracheal length measurements were performed by the same person (T.Y.) to eliminate the variability bias that could be introduced if the values were measured by different examiners. The body height (cm), body weight (kg), and age (months) of the patients were retrospectively retrieved from the hospital records. The body height and body weight were measured in the supine position in small paediatric patients including infants who could not yet stand alone, and in the standing position in patients who could stand alone.
FIGURE 1
Measurement of tracheal length on chest radiographs using the Picture Archiving Communication System. The distance between the vocal cords (arrow) and the carina tracheae was defined as the tracheal length. This male participant was 2 years and 4 months old, 77.4 cm tall, weighed 10.1 kg, and underwent surgery for complete atrioventricular septal defect. The tracheal length was approximately 6.3 cm, which was 8.1% of the body height

Second stage: validation phase to evaluate the formula for ideal endotracheal tube insertion depth at the vocal-cord level
In the second stage, endotracheal intubation was performed according to the results of the first stage of the study, and the distance between the ETT tip and carina tracheae was measured on postoperative chest radiographs (Figure 2). To avoid unnecessary exposure of the patients to extra X-rays in the current study, we only included patients whose postoperative chest radiographs were essential and planned to check the remains or confirm the absence of pneumothorax before waking the patients from general anaesthesia. Therefore, all postoperative chest radiographs were taken in the supine position. We included a total of 132 paediatric patients with congenital heart diseases who underwent cardiovascular surgery, 14 paediatric patients without congenital heart diseases who underwent non-cardiac surgery in the chest area such as Hickman catheter implantation, 91 adult patients who underwent cardiac surgery, and 71 adult patients who underwent non-cardiac surgery with central venous catheter insertion between August 2020 and May 2021 at Niigata University Medical and Dental Hospital.
FIGURE 2
The distance between the endotracheal tube (ETT) tip and carina tracheae was measured on the postoperative chest radiographs of a male paediatric patient who was 2 years and 4 months old, with a height of 77.4 cm (the same patient as in Figure 1). The ETT was inserted at 5.5 cm (approximately 7% of the body height) from the vocal cords. The measured distance between the ETT tip and carina tracheae was 1.9 cm (approximately 2.5% of the body height). The calculated tracheal length was 7.4 cm (approximately 9.5% of the body height)

Statistical analyses
Numerical data are presented as the mean ± standard deviation (SD), and their 95% confidence interval (CI) was calculated. Statistical significance was determined as P < 0.05 by using the f-test. Scatter plots were drawn and equations and Pearson’s correlation coefficient (Pearson’s r) were calculated to determine the relationship between the tracheal length and the body height in the first stage. Scatter plots were used to evaluate variations in the distance between the ETT tip and the carina tracheae in the second stage. N indicated the number of patients included.
RESULTS
First stage: retrospective observational evaluation to compare the tracheal length between cardiac and non-cardiac paediatric patients
Association between tracheal length and body height in cardiac paediatric patients
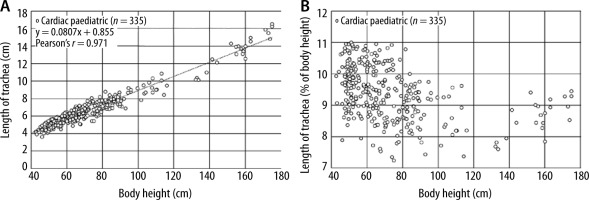
Our previous study investigated the relationship between body height, body weight, or patient age and tracheal length and revealed that body height exhibited the strongest correlation with tracheal length in cardiac paediatric patients, including neonates [6]. Therefore, in this study, we used a scatter plot to exclusively determine the association between tracheal length and body height in cardiac paediatric patients at Niigata University Medical and Dental Hospital. The data of 335 patients who were included in the current study were as follows: male/female patients, 145/190; body height, 36.0–175.0 cm; body weight, 1.4–78.8 kg; and age, 0 days to 216 months. The mean ± SD and 95% CI for body height and age of the cardiac paediatric patients were 72.4 cm ± 27.4 cm and 69.4–75.3, and 18.4 months ± 32.0 months and 14.9–21.9, respectively. The association between tracheal length and body height was evaluated using the scatter plot, and the following formula was obtained: tracheal length (cm) = 0.0807 × (body height [cm]) + 0.855 (Pearson’s r = 0.971) (Figure 3A). Although the calculated Pearson’s r indicates that there is a very strong positive correlation between tracheal length and body height, this formula is extremely complex to apply in daily clinical practice, and in addition, it only represented the aver-age tracheal length of patients, suggesting that single-lung intubation could occur in some patients when ETTs were inserted at the vocal-cord level using the length based on this formula. Therefore, a scatter plot, whose horizontal axis and vertical axis represented the body height and the percentage ratio of the tracheal length to body height (%BH tracheal length; Figure 3B), respectively, was drawn. The tracheal length ranged from 7 to 11% of the body height in the cardiac paediatric patients of this study (minimum, 7.24%; maximum, 11.0%).
FIGURE 3
Association between tracheal length and body height in Japanese cardiac paediatric patients. A) Horizontal axis: body height (cm); vertical axis: tracheal length (cm). Average tracheal length (cm) = 0.0807 × (body height [cm]) + 0.855 (Pearson’s r = 0.971). B) Horizontal axis: body height (cm) of the patients; vertical axis: percentage ratio of the tracheal length to body height (%BH tracheal length)
Association between tracheal length and body height in non-cardiac paediatric patients
A total of 275 paediatric patients (male/female: 147/128; body height: 42.0–169.6 cm; body weight: 1.5–100.0 kg; age: 0 days to 216 months) without congenital heart disease, who were undergoing non-cardiac surgery at Niigata University Medical and Dental Hospital, were evaluated. The mean ± SD and 95% CI for body height and age of the non-cardiac paediatric patients were 88.9 cm ± 30.7 cm and 85.2–92.5, and 46.5 months ± 54.7 months and 40.0–53.0, respectively. The association between tracheal length and body height was evaluated using a scatter plot, and the following formula was obtained: tracheal length (cm) = 0.0732× (body height [cm]) + 0.972 (Pearson’s r = 0.955) (Figure 4A). For the same reason as above, a scatter plot with body height on the horizontal axis and %BH tracheal length on the vertical axis was drawn (Figure 4B). The tracheal length ranged from 7 to 11% of the body height in the non-cardiac paediatric patients (minimum, 7.0%; maximum, 11.0%).
FIGURE 4
Association between tracheal length and body height in non-cardiac paediatric patients. A) Horizontal axis: body height (cm); vertical axis: tracheal length (cm). Average tracheal length (cm) = 0.0732 × (body height [cm]) + 0.972 (Pearson’s r = 0.955). B) Horizontal axis: body height (cm) of the patients; vertical axis: percentage ratio of the tracheal length to body height (%BH tracheal length)

Comparison of the distribution of the percentage ratio of the tracheal length to body height (%BH tracheal length) between cardiac and non-cardiac paediatric patients
The distribution of the %BH tracheal length was compared between cardiac and non-cardiac paedia-tric patients. The mean ± SD and 95% CI for %BH tracheal length of the cardiac paediatric patients were 9.38% ± 0.84% and 9.29–9.47, respectively. The mean ± SD and 95% CI for %BH tracheal length of the non-cardiac paediatric patients were 8.57% ± 1.00% and 8.45–8.69, respectively (Figure 5). The f-test proved that the distribution of %BH tracheal length as well as body height and age of the cardiac and non-cardiac paediatric patients included in the current study were not statistically equally distributed (P < 0.05). Nevertheless, the tracheal length ranged from 7 to 11% of the body height in both cardiac and non-cardiac paediatric patients, as shown above.
FIGURE 5
Comparison of the tracheal length between cardiac and non-cardiac paediatric patients. Horizontal axis: body height (cm) of the patients; vertical axis: percentage ratio of the tracheal length to body height (%BH tracheal length). The tracheal length ranged from 7 to 11% of the body height in cardiac (n = 335) and non-cardiac (n = 275) paediatric patients

Second stage: prospective evaluation of the formula for ideal endotracheal tube insertion depth at the vocal-cord level
The first stage of the study revealed that the tracheal length was 7–11% of the body length in Japanese paediatric patients with or without congenital heart diseases. Therefore, we hypothesized that single-lung intubation in paediatric patients could be avoided by inserting ETTs with the minimum tracheal length of their specific racial group at the vocal-cord level. To verify this hypothesis, ETTs were inserted at a depth of 7% of the body height at the vocal-cord level in paediatric patients with congenital heart diseases who underwent cardiovascular surgery (N = 132, male/female: 64/68, body height: 44.0–173.3 cm, age: 0 days to 216 months) and paediatric patients without congenital heart diseases who underwent non-cardiac surgery (N = 14, male/female: 8/6, body height: 50.0–157.5 cm, age: 0 days to 149 months) at Niigata University Medical and Dental Hospital. The distance between the ETT tip and the carina tracheae was measured on postoperative chest radiographs taken in the supine position (Figure 2). Furthermore, to confirm that the results of the first stage were also applicable to adults, a verification phase was conducted using the same method in adult patients undergoing cardiac surgery (N = 91, male/female: 49/42, body height: 139.5–183.3 cm, age: 22 years 5 months to 83 years 4 months) or non-cardiac surgery (N = 71, male/female: 44/27, body height: 137.0–178.4 cm, age: 23 years 7 months to 91 years 6 months) at Niigata University Medical and Dental Hospital. None of the 308 paediatric and adult patients underwent single-lung intubation after insertion of ETTs at a depth of 7% of the body height at the vocal-cord level. The distance between the ETT tip and carina tracheae was generally within approximately 4% or less of the body height for all body height ranges. The minimum and maximum values of the distance between the ETT tip and carina tracheae were as follows: cardiac paediatric patients, 0.232% and 4.219%; non-cardiac paediatric patients, 0.284% and 4.241%; adult cardiac patients, 0.393% and 4.331%; non-cardiac adult patients, 0.482% and 4.290%.
The tracheal length is calculated using the following formula:
“tracheal length” = “ETT insertion length at the vocal-cord level (= 7% of body height)” + “distance between the ETT tip and the carina tracheae”.
That is, the length of the trachea for each group included in the second stage was calculated as follows: cardiac paediatric patients, 7.232–11.219%; non-cardiac paediatric patients, 7.284–11.241%; adult cardiac patients, 7.393–11.331%; non-cardiac adult patients, 7.482–11.290%. This result agrees with the result of the first stage that the tracheal length generally ranges from 7 to 11% of the body height in paediatric patients and it can be applied to adult patients as well.
DISCUSSION
Determination of the appropriate depth of endo-tracheal intubation and simple and reliable endotracheal intubation procedures are very important for safe airway management. This is particularly important in small babies, including neonates or premature infants, who have a shorter tracheal length and less reserve capacity for hypoxia than adults.
Our previous study [6] involving 425 cardiac paediatric patients, including neonates, showed that body height had the strongest correlation with tracheal length. This result is in agreement with other reports that identified body height as the most strongly correlated parameter with tracheal length in paediatric patients including neonates [7–10]. Therefore, we investigated only the association between the tracheal length and body height in the first stage of the current study involving 335 cardiac and 275 non-cardiac Japanese paediatric patients. The findings showed that the tracheal length ranged from 7 to 11% of the body height in Japanese paediatric patients both with and without congenital heart diseases (Figures 3 and 4).
In the second stage (prospective validation) of the study, ETTs were inserted at a length equivalent to 7% of the body height at the vocal-cord level in 146 paediatric patients (132 paediatric patients with congenital heart diseases and 14 without congenital heart diseases), since it corresponded to the shortest tracheal length in Japanese paediatric patients, whose tracheal length ranged from 7 to 11% of the body height. It was confirmed that no patient experienced single-lung intubation at this insertion depth, and that the distance between the ETT tip and carina tracheae was within 4% of the body height for all body height ranges.
Based on the results of the current study and our previous study [6], which revealed a clear ethnic difference in the tracheal length of cardiac paediatric patients including neonates, between patient groups from Germany (ranging from 6 to 10% of the body height) and Japan (ranging from 7 to 11% of the body height), we hypothesized that the tracheal length of non-cardiac paediatric patients from Germany would also range from 6 to 10% of the body height. That is, single-lung intubation can be avoided by inserting ETTs at a length of 6% of the body height (the minimum tracheal length for German paediatric patients) at the vocal-cord level in German paediatric patients both with and without congenital heart diseases.
The most important condition when assessing the ETT depth on chest radiographs is that the ETT, which is inserted at the minimum tracheal length at the vocal-cord level for the population groups, appears to be shallow on chest radiographs in patients with a relatively long trachea in a population group. This never means increase in the accidental extubation risk, because the ETT is inserted at the minimum tracheal length from the vocal cords for the ethnic group of the patient (i.e., 6% of the body height in Europeans and 7% of the body height in Asians). This suggests that the ETT should be inserted at a sufficient length from the vocal cords; thus, if the ETT appears to be shallow on the chest radiographs, it should be interpreted that it is not a matter of the ETT insertion length but of the length of the patient’s trachea.
By inserting ETTs at a length of 7% of the body height (the minimum tracheal length for Japanese) at the vocal-cord level in the second stage (prospective validation), we showed that the distance between the ETT tip and the carina tracheae as well as the calculated percentage ratio of the tracheal length to body height in adults were similar to the corresponding values in paediatric patients. Hence, the results obtained in the first stage investigation with paediatric patients can also be genera-lized to adult patients.
CONCLUSIONS
The current study demonstrated that endotracheal intubation at an adequate depth could be achieved by inserting ETTs at the minimum tracheal length for the specific ethnic group at the vocal-cord level. This would help avoid unnecessary procedures, such as withdrawing an ETT from the carina tracheae after single-lung intubation, in paediatric patients [11], including neonates and premature infants, as well as adults. Further, the ETT depth at the mouth corner or nasal wing is only an outcome of the anatomical differences of the oral and nasal cavity among patients and is not an appropriate indicator of the ETT insertion length. The insertion depth at the vocal-cord level should be calculated to confirm whether the position of the vocal-cord marker on the ETT, which differs among products, is adequate for each patient (Figure 6). If not, an appropriate insertion depth should be marked on the ETT in advance before initiating the endotracheal intubation procedure.
FIGURE 6
Confirmation of depth marker and appropriate endotracheal tube (ETT) insertion length for a 2-year-4-month-old male paediatric patient with a body height of 77.4 cm (same patient as in Figures 1 and 2). A) It was confirmed that the appropriate ETT insertion length (7% of body height is equivalent to approximately 5.5 cm) coincided with the first depth marker from the tip (arrow) on a cuffed Shiley endotracheal tube (Covidien Japan Inc., Tokyo, Japan) with an inner diameter of 4.5 mm. B) An appropriate vocalcord marker should be placed at 5.5 cm from the tip (arrow) before the endotracheal intubation procedure when choosing an uncuffed Portex endo-tracheal tube (Smiths Medical Japan Ltd., Tokyo, Japan) with an inner diameter of 4.5 mm, as was the case with this patient





