Preoperative fasting has long been regarded as a cornerstone of anesthetic practice. In the past, “nothing per os” was the ideal, and it was supposed to last at least eight hours. However, the recent fasting recommendations have changed a lot by allowing free clear fluid intake up to two hours before induction of anesthesia [1]. Drinking clear liquids with carbohydrates up to two hours before surgery is advised according to the most recent guidelines. 400 mL is the suggested amount [2].
Anesthesiologists are concerned with gastric emptying especially when general anesthesia is planned. Measurement of residual gastric volume is therefore important to estimate the final amount of fluids remaining in the stomach just before induction of anes-thesia. This includes measurement of plasma levels of orally administered drugs e.g. paracetamol [3], nasogastric aspiration of gastric contents [4], measurement of upper abdominal impedance, measurement of radioactivity after ingestion of radioactive substance [5], X-ray after ingestion of contrast medium and most recently utilizing ultrasonography [6].
Domperidone is a selective dopamine-2 receptor antagonist. It increases gastroduodenal contractions and coordination, which stimulates upper gastrointestinal motility. It does not cross the blood-brain barrier, which means that, unlike other antiemetic and prokinetic medications, it is less likely to have sedative or extrapyramidal effects [7]. Domperidone functions as an antiemetic by affecting the chemoreceptor trigger zone within the area postrema (outside of the blood-brain barrier) [8].
Associated risk of ventricular arrhythmias was virtually nullified by withholding the injectable form of the drug in the 1980s and by restricting the daily oral dose to below 30 mg [9].
In the present research, it was hypothesized that oral domperidone administration at a dose of 10 mg would enhance the gastric emptying of 400 mL of clear apple juice given 2 hours before induction of general anesthesia.
METHODS
The Ain-Shams University Faculty of Medicine Research Ethics Committee certified this prospective randomized controlled comparative trial (FMASU MS 210/2022), and it was registered at clinicaltrials.gov (NCT05577292) on 05/10/2022, before patient enrollment started on 10/10/2022. The study ended on 15/04/2023. For this study, the Declaration of Helsinki’s principles were followed. The study was conducted at the Department of General Surgery at the Ain-Shams University.
Forty adult patients were enrolled in the study with an age range of 21–65 years, both sexes, with a score of American Society of Anesthesiologists physical status (ASA-PS) I or II, who were scheduled for elective surgery under general anesthesia. All patients who were enrolled provided written fully informed consent.
Patients were excluded from the study if they refused to share or they were known or suspected of delayed gastric emptying (gastroparesis) which may be idiopathic, due to diabetes mellitus or post-gastric surgery. Also, patients had an allergy to the study drugs, had a history of prolonged QT syndrome or cardiac dysrhythmia, and patients having procedures that are known to cause a high incidence of postoperative nausea and vomiting (PONV), such as cholecystectomy, gynecological, ophthalmological, otorhinolaryngological, and laparoscopic procedures, were not included in the study.
All patients were told to abstain from food and drink for 6 to 8 hours the day before surgery. Every patient underwent a clinical evaluation, and standard preoperative tests including complete blood count (CBC), coagulation profile, liver function tests, kidney function tests, fasting blood sugar, and ECG were performed.
Patients were randomly assigned using computer-generated random numbers. After enrolling the patients, a sealed opaque envelope containing the group allocation number was opened. Patients were randomly assigned to one of the following groups: Group D (n = 20): patients received oral domperidone 10 mg tablet orally 2 hours before surgery and Group P (n = 20): patients received a placebo tablet 2 hours before surgery. In both groups, patients received 400 mL of apple juice as a clear fluid. We used a placebo in the control group to determine if any difference between groups, practically the effect on the gastric residual volume, was due to the domperidone action or the participants’ perceptions (the placebo effect).
Measurement of gastric residual volume
Measurement of preoperative gastric residual volume in the right lateral position was performed one hour and two hours after oral apple juice intake using ultrasound by a curved-array 2- to 5-MHz transducer of a Mindray portable ultrasound device in the right lateral decubitus (RLD); this is calculated by defining the cross-sectional area (CSA) of the antrum of the stomach. Anteroposterior diameter (D1) and cranio-caudal diameter (D2) were measured and the cross-sectional area was calculated.
Gastric residual volume (mL) = 27.0 + 14.6 × right-lateral CSA – 1.28 × age (equation by Perlas et al. [10]).
The left liver lobe and the descending abdominal aorta served as the anterior and posterior landmarks, respectively, for this evaluation. According to antral shape and contents, a flat antrum with anterior and posterior walls was assumed to be empty; a distended antrum with hypoechoic contents and thin walls was assumed to be fluid-containing; and a distended antrum with contents showing mixed echogenicity was assumed to be solid-containing and thus omitted from the study.
Anesthetic technique
Lactated Ringer’s solution10 mL kg–1 was initiated after inserting a wide-bore IV cannula. Before the induction of anesthesia, routine monitoring was started. This included checking the heart rate (HR), blood pressure (BP), and oxygen saturation (SpO2).
Fentanyl 2 μg kg–1 and propofol 2 mg kg–1 were administered to induce general anesthesia, and atracurium besylate 0.5 mg kg–1 was administered to aid in endotracheal intubation. Following intubation, capnography was connected, and the lungs were ventilated to maintain normocapnia (etCO2 of 35–40 mmHg). This end-tidal concentration of isoflurane was between 1% and 1.5%. Atracurium besylate top-up doses of 0.1 mg kg–1 were administered if needed. During surgical manipulation, a further dose of fentanyl 1μg kg–1 was administered. No medications with a substantial risk of PONV (such as ketamine or nitrous oxide) were used. Continuous measurements of heart rate, systolic, diastolic, mean arterial blood pressure, and SpO2 were performed during the intraoperative period.
When the procedure was finished, the isoflurane was stopped, and the remaining atracurium block was countered with neostigmine 0.05 mg kg–1 and atropine 0.02 mg kg–1. Patients were taken to the post-anesthesia care unit (PACU) after being extubated.
The primary outcome in the study was to measure the gastric residual volume by ultrasound, one and two hours after premedication with domperidone with clear fluid ingestion and before induction of general anesthesia. The secondary outcome included addressing the incidence of postoperative nausea and vomiting according to “the PONV impact scale” in the first post-operative 24 hours [11].
Q1. Have you experienced dry retching or vo-mited?
0. No, 1. Once, 2. Twice, 3. Three or more times
Q2. Have you experienced being nauseous (described as “an unsettled feeling in the stomach and a slight urge to vomit”)? If so, has your nausea prevented you from performing basic daily tasks like getting out of bed, moving around comfortably in bed, walking normally, or eating and drinking?
0. Not at all, 1. Sometimes, 2. Often or most of the time, 3. All of the time.
The numerical answers to questions 1 and 2 should be added to determine the PONV Impact Scale score. Clinically significant PONV is defined as a PONV Impact Scale score of ≥ 5.
Sample size calculation
No study on measuring the gastric residual volume (GRV) after premedication with domperidone with clear fluid ingestion was found. Therefore, a pilot study was performed by the same research group before starting the present study to estimate the sample size (unpublished). In this pilot study, the effect of domperidone was tested on GRV; domperidone was capable of decreasing GRV from 76.11 ± 12.16 to 65.12 ± 11.31 mL. Therefore, a sample size of 19 in each group was sufficient to achieve a power of 80% with an α error of 0.05. We included 20 patients in each group.
Statistical analysis
SPSS Statistics version 23.0 (IBM, USA) was employed to analyze the collected data. When the distribution of the quantitative data was parametric (normal), it was shown as mean with standard deviation and range; when it was not (non-parametric data), it was shown as median with inter-quartile range (IQR). Additionally, qualitative variables were shown as percentages and numbers. Shapiro-Wilk and Kolmogorov-Smirnov tests were used to examine the data for normality. P-values less than 0.05 were regarded as significant, and those greater than 0.05 were regarded as insignificant.
RESULTS
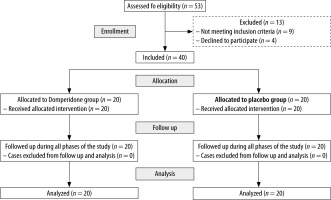
Fifty-three patients in total were evaluated for study eligibility; 9 were not selected because they did not meet the criteria for participation, and 4 patients declined to participate. Finally, 40 patients who were scheduled for elective surgery under GA were included in this study. Patients were randomly allocated to 2 groups (20 in each group). Figure 1 displays the flowchart for the Consolidated Standards of Reporting Trials (CONSORT).
There were no statistically significant differences between the two groups regarding demographic data including age, sex, ASA status, and type of surgery (Table 1).
TABLE 1
Comparison between group D and group P regarding demographic data
Regarding ultrasound-derived measures, one hour after the clear fluid ingestion and either oral domperidone or placebo, there were no statistically significant differences in all parameters measured (D1 and D2) or calculated (CSA and GRV) between groups (Table 2).
TABLE 2
Comparison between group D and group P regarding ultrasound measurements in the right lateral position after 1 hour
However, all previously mentioned parameters were statistically significant different between the two groups 1 hour later with group D having the lower values (Table 3). All measured parameters in group D showed statistically significantly lower values 2 hours after ingestion compared with group P (Table 4).
TABLE 3
Comparison between group D and group P regarding ultrasound measurements in the right lateral position after 2 hours
TABLE 4
Comparison between group D and group P regarding change in ultrasound measurements in the right lateral position (after 2 hours – 1 hour)
Regarding postoperative nausea and vomiting (PONV), there were no statistically significant findings in both groups (Table 5).
DISCUSSION
After publication of the iconic study of Mendelson [12] in 1946, the anesthetic practice changed with regard to preventing oral intake preoperatively. With the introduction of the concept of ERAS (Enhanced Recovery After Surgery) in 1997 [13], the practice of prolonged preoperative fasting was questioned because it harmed the patient’s overall recovery from surgery. As markers of stress reactions, postoperative accelerated protein catabolism and increased insulin resistance were found to be related to longer preoperative fasting [14]. In light of this, the American Society of Anesthesiologists (ASA) [15], which first released pre-operative fasting guidelines in 1999 and later updated them in 2017, shortened them and advised all healthy patients scheduled for elective surgery to be allowed to eat a heavy, substantial meal 8 hours before surgery, a light meal (toast and clear tea) at 6 hours before, and unlimited clear liquids (water, fruit juices without pulp, clear tea, and black coffee) up to 2 hours before surgery (2017). Long-term preoperative fasting is upsetting for patients as well as their families without having any beneficial effects on clinical outcomes.
A lot of factors determine the possibility of the event of pulmonary aspiration and how to avoid it as much as possible. One of the essential elements is the gastric residual volume, which is directly proportionate to the possibility of aspiration; the greater the gastric residual volume is, the greater is the liability of the patient to aspirate. Research work on GRV was not widespread until the mid-1990s and it was mainly directed at measuring it for the avoidance of pulmonary aspiration for ICU patients on enteral feeding. Gastric emptying could be evaluated by various methods, for example, scintigraphy [16], the paracetamol absorption test [17], refractometry [18], the breath test [19], and gastric impedance monitoring [20]. With the recently introduced ultrasound techniques, measurement of GRV is a bedside test performed in a matter of minutes.
Because of all the above, this study was conducted to assess the effect of domperidone as a prokinetic drug on GRV before induction of anes-thesia. This drug has known effects on enhancing gastric motility and the fewest possible side effects. The main outcome of the current study is that domperidone proved effective in enhancing gastric emptying of the preoperatively ingested clear fluids, 2 hours before induction of general anesthesia. One hour after ingestion of 400 mL the calculated gastric volume was 71.41 and 75.16 mL in groups D and P, respectively, without a significant difference between groups. One hour later, the control group (Group P) dropped to 70.22 mL. Gastric volume in the study group continued to decrease to 55.95 mL, proving the efficacy of domperidone as a prokinetic drug. Changes in gastric volume from one hour after ingestion of the clear fluid to 2 hours after ingestion of the clear fluid were significant in both groups. Group D showed a significantly greater decrease in gastric volume (–15.8%) compared with group P (–5.00%).
Previous research on another prokinetic drug (metoclopramide) was performed on patients who had fasted for surgical intervention. In a study by Jellish et al. [21], the gastric volume was minimal even in diabetic patients to the degree that the authors concluded that metoclopramide prophylaxis was not necessary to reduce gastric volumes preoperatively. Sayyadi et al. [22] again challenged the prokinetic properties of metoclopramide but this time on patients scheduled for urgent surgery with insufficient fasting time. They concluded that metoclopramide could accelerate gastric emptying. Metoclopramide has a long history with anesthetic management being available worldwide in almost all operative theatres. It carries the advantages of being available as an injectant for IV and IM use and as a tablet for oral administration.
On the other hand, domperidone was not previously tested for perioperative use by anesthetists. The reasons behind this were the availability of only oral formulations and restriction of usage in some countries. Oral syrup is available for pediatric usage. Moreover, in the current study, no clear effect of the drug was observed after one hour of ingestion. Two hours after ingestion, a greater gastric emptying effect was recorded. This means that oral administration of domperidone needed less than 2 hours for the onset of action.
In the current study, it was presumed that at time zero the empty stomach received a volume of 400 mL of clear fluid. One hour later this volume was reduced “physiologically” to 71–75 mL. After another hour this volume was reduced “physiologically” to 70 mL or “pharmacologically” to 56 mL. More studies are needed, with a consideration of using a larger volume (more than 400 mL) preoperatively for optimization of patient satisfaction and better hydration with the use of domperidone to induce gastric emptying to maintain the risk of vomiting/regurgitation at zero level as the patient who is fasting for 6–8 hours [23]. More studies are needed to investigate the effect of domperidone on a full/ partially full stomach to reduce gastric volume before trauma and emergency cases can go to the operating theater. This also may extend to include critical care patients who are going to the operation theatre either for emergency or scheduled surgery.
The current study had some limitations. First, it was a single-center study. Second, our results were limited to patients with elective surgery. Additionally, we did not include patients with gastroparesis to avoid confounding factors related to delayed gastric emptying.
CONCLUSIONS
The findings of this study demonstrate that preoperative oral domperidone may be an effective agent to decrease the GRV measured by ultrasound, more than the decrease of GRV by applying a placebo. Further studies are needed to determine the optimal dosage of preoperative oral domperidone.