Introduction
Obesity has become one of the major health problems for healthcare. According to the World Health Organization (WHO), worldwide in 2016, 39% of adults were overweight and 13% were obese [1]. This means the number of obese people has tripled since 1975. In 2020, 39 million children under the age of 5 were overweight or obese. According to the WHO, one billion people will be obese by 2030 [1, 2]. Obesity and overweight are characterized by excessive fat accumulation in the body, which can cause health problems such as insulin resistance, type 2 diabetes mellitus (T2DM), sleep disorders, cardiovascular diseases, dementia, immune disorders, and nonalcoholic fatty liver disease (NAFLD), in addition to many type of cancers [3]. The greater the mass of adipose tissue, the more pro-inflammatory factors are secreted [e.g. interleukin (IL)-1, IL-6, tumor necrosis factor α (TNF-α)], influencing the risk of metabolic diseases [4]. Lifestyle modification, caloric restriction and weight loss reverse changes associated with low-grade inflammation such as metabolic syndrome and endothelial dysfunction [4, 5]. The Mediterranean diet is recommended as a model of nutrition conducive to the normalization of body weight and for prevention of cardiovascular diseases. This type of nutrition contains food groups and nutrients with anti-inflammatory properties. It eliminates pro-inflammatory factors and enriches the diet with whole grains, nuts, legumes, vegetables, fruits, skimmed dairy, eggs, fish and vegetable oils, for example olive oil. These food groups are rich in antioxidants, flavonoids, fiber and folate [6].
Numerous studies have described the role of IL-6, TNF and interferon (IFN) in the pathogenesis of obesity. However, our study aims to describe these three cytokines in obese patients in relation to dietary habits, lifestyle and body composition. The results of our study may indicate the direction of further research to determine the prevention of diseases resulting from obesity and inflammation, including cardiovascular diseases.
Material and methods
Ethics
The project was approved by the institutional Bioethics Committee (Resolution No. 10/04/2017) and was carried out in accordance with the Declaration of Helsinki. Prior to the study, all subjects voluntarily agreed to participate by signing the required documents.
Subjects
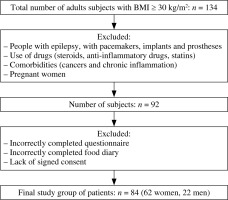
A total of 134 individuals with obesity [body mass index (BMI) ≥ 30 kg/m2] were eligible for the study. Among the volunteers, those who could not adopt an upright body posture due to the inability to perform anthropometric tests were excluded immediately. Also pregnant women, people with epilepsy, with pacemakers, implants and prostheses were excluded from the project due to the bioelectrical impedance analysis (BIA) study. In addition, people taking drugs affecting the immune system (steroids, anti-inflammatory drugs, statins) were excluded from the study. Subjects suffering from cancer and chronic inflammatory diseases were also excluded. All of the above conditions could change the level of the tested cytokines so were not examined. The data of those whose questionnaires and food diaries were incomplete were excluded. The condition necessary to participate in the study was to sign an informed and voluntary consent form. A total of 42 subjects were rejected from the results. The study finally involved 84 people (73.8% women and 26.2% men) (Fig. 1). They were aged 18 to 73, and the mean age was 41.38 ±12.54 years.
The minimum body weight of the subjects was 70.6 kg, the maximum was 156.4 kg, and the mean body weight was 103.01 ±18.23 kg. The mean BMI was 36.65 ±5.27 kg/m2. Table 1 presents the obesity class among the subjects.
Table 1
Obesity class among the subjects
| Obesity class | n | % |
|---|---|---|
| Obesity class I | 34 | 40.5 |
| Obesity class II | 34 | 40.5 |
| Obesity class III | 16 | 19.0 |
| Total | 84 | 100.0 |
Among the subjects, 21 (25%) were diagnosed with arterial hypertension, 3 (3.6%) had NAFLD, 6 were treated for hypothyroidism (7.1%) and 2 for atherosclerosis (2.4%). The participants took the following drugs: blood pressure lowering drugs (n = 21), levothyroxine (n = 4), β-blockers (n = 10), non-steroidal anti-inflammatory drugs (NSAIDs) ad hoc (n = 3).
Blood sampling and laboratory analysis
Trained personnel collected blood samples in the morning (7:00-9:00) from subjects who had not eaten or drunk anything but water for 12-14 hours before. The subjects were instructed to refrain from alcohol, coffee, diuretics and physical activity for 24 hours prior to giving a blood sample. Blood samples were collected in MLVacuCol (MEDLAB-PRODUCTS Sp. z o.o., Raszyn, Poland) and centrifuged at 700 × g at 15°C to 25°C. The serum was cryopreserved at –86°C. The samples were analyzed using the commercially available Milliplex MAP Human Th17 Magnetic Bead Panel Kit by multiplex magnetic bead assay (Merck Millipore, Burlington, MA, USA) and the FLEXMAP 3D system (Merck Millipore, Burlington, MA, USA). This kit enables the analysis of Th17 cytokine and chemokine biomarkers in serum.
Height and body composition measurements
Bioelectrical impedance analysis examination and height measurement were performed in the morning on the fasted subjects. Body height was measured twice using a Tanita HR-001 stadimeter (TANITA, Tokyo, Japan) and the mean value was calculated. A body composition analysis was performed using bioelectrical impedance using a variable frequency analyzer (5 kHz, 50 kHz, 250 kHz) MC-780 MA Tanita (TANITA, Tokyo, Japan). The accuracy of segmental multifrequency BIA is comparable to that of dual-energy X-ray absorptiometry and has been confirmed in various clinical studies [7–9]. The following parameters in percentages and kilograms were obtained: fat-free mass (FFM), fat mass (FM), muscle mass (MM), total body water (TBW), intra- and extracellular water (ICW and ECW) (kg and %) and level of visceral adipose tissue (VF). All of those parameters were also obtained in total and in segments (torso and limb). The GMON PRO software (Medizin & Service, Chemnitz, Germany) was used to collect the results of the analysis.
Lifestyle and nutrition assessment
Each participant had previously completed a very detailed food diary containing 2 work days and 1 weekend day of normal nutrition. The respondents also completed the original questionnaire enriched with a standardized food consumption frequency questionnaire – FFQ-6. The FFQ-6 is a qualitative questionnaire and analyzes the frequency of consumption of selected food groups. The wide scope of application of the FFQ-6 questionnaire has been confirmed by its use, e.g. in a pilot, controlled, randomized study in children with celiac disease on a gluten-free diet, in a study of people with non-alcoholic fatty liver disease and among hemodialysis patients [10–13]. The 62-item questionnaire has been modified to distinguish pro- and anti-inflammatory products. The survey included questions about eating habits, stimulants and physical activity. In addition, nutritional values were summarized using the Aliant program (Cambridge Nutritional Sciences, Alva, UK).
Statistical analysis
Statistica 13.1 (StatSoft, Kraków, Poland) was used for statistical analysis. Comparison of serum concentrations in the blood of the obese participants according to obesity classes was made using the Kruskal-Wallis test. The data did not meet the basic assumptions of parametric tests, such as compliance of the tested variables with a normal distribution. For this reason, they were analyzed using non-parametric tests. The assessment was made using the Shapiro-Wilk test. Numerical features in both populations were assessed using the Mann-Whitney U test. Variables not meeting the criteria of normal distribution were analyzed using Spearman’s rank coefficient. Pearson’s chi-square test was used for categorical variables. The level of statistical significance was p < 0.05.
Results
Due to the large amount of data collected, results important for the manuscript and statistically significant results are described in this section. Others are included in supplementary tables. Each of them represents an analysis of the data of different experiments (BIA, FFQ-6, nutritional diary) in correlation with cytokine levels.
A statistically significant correlation was found between reporting having diagnosed atherosclerosis and the level of pro-inflammatory cytokines. The subjects with atherosclerosis had higher levels of IL-6 (p = 0.026) and IFN-γ (p = 0.029). The group of individuals with atherosclerosis was very small (n = 2), so these correlations require further research. The correlations between the levels of IL-6, IFN-γ and TNF-α and the other morbidities occurring among the subjects are shown in Table 2.
Table 2
Correlation between diagnosed chronic diseases reported by participants and cytokine levels
| Cytokine levels | Hypertension | Non-alcoholic fatty liver disease | Treated hypothyroidism | Atherosclerosis | ||||
|---|---|---|---|---|---|---|---|---|
| Z | p | Z | p | Z | p | Z | p | |
| IFN-γ (pg/ml) | −0.01 | 0.991 | 0.60 | 0.547 | 1.95 | 0.051 | 2.18 | 0.029* |
| IL-6 (pg/ml) | 0.06 | 0.949 | 0.08 | 0.935 | 1.64 | 0.101 | 2.23 | 0.026* |
| TNF-α (pg/ml) | 1.52 | 0.130 | 0.99 | 0.322 | 1.69 | 0.091 | 1.00 | 0.319 |
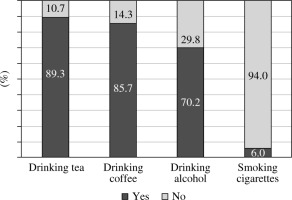
The results from the original questionnaire, FFQ-6 and nutritional diary were thoroughly analyzed. In the diet of subjects, the frequency of consumption of sweetened dairy products (R = 0.22, p = 0.047) correlated positively with the level of IL-6, while consuming large amounts of alcohol negatively correlated with the level of IL-6 (R = 0.23, p = 0.043). A high content of sugars in the diet showed a positive association with the level of TNF-α (R = 0.28, p = 0.010). Sugars include monosaccharides and disaccharides. In addition, correlations between galactose (R = 0.24, p = 0.030), sucrose (R = 0.28, p = 0.010) and the TNF-α level were observed. The correlations between the levels of IL-6, IFN-γ and TNF-α and the other food groups or nutrients are shown in Supplementary Tables S1 and S2. The original questionnaire included questions about eating habits (amount of fluids drunk, number of meals, snacking between meals, eating place, sweetening drinks, using more than 5 g of salt per day), addictions and physical activity. These lifestyle aspects had no statistically significant association with cytokine levels. The frequency of dietary habits is shown in Figure 2.
Fig. 2
Percentage of respondents who reported drinking alcohol, tea, and coffee and smoking cigarettes
Respondents were also asked to state whether they were physically active, which gave them a subjective opinion about the level of exercise. Only 22.6% considered themselves physically active. People practicing sports had a higher IL-6 concentration (p = 0.049) in comparison with physically inactive people. There were no differences in IFN-γ (p = 0.387) and TNF-α (p = 0.859) between physically active and inactive subjects. Respondents did not indicate the number of hours of physical activity per week. They subjectively stated whether they were physically active or not. Due to significant obesity, activity is very difficult and it is impossible to meet the WHO recommendations [14]. After the statistical analysis of the results of the BIA, the following significant relationships were found. The level of IL-6 showed a positive correlation with the content of subcutaneous adipose tissue (SAT) measured on the limbs, but not visceral fat. There was a correlation between level of IL-6 (pg/ml) and fat mass in the right leg (R = 0.26, p = 0.020), the left leg (R = 0.24, p = 0.30), the right hand (R = 0.26, p = 0.020), and the left hand (R = 0.22, p = 0.047). All the correlations between the levels of IL-6, IFN-γ and TNF-α and the results of full BIA analysis are shown in Supplementary Table S3. Correlations for obesity class and concentrations of IFN-γ (H = 0.3388992, p = 0.8441), IL-6 (H = 2.195273, p = 0.3337) and TNF-α (H = 0.8682144, p = 0.6478) were not statistically significant.
There was a positive correlation between IL-6, IFN-γ and TNF-α. The level of IL-6 showed a positive correlation with the level of IFN-γ (R = 0.46, p < 0.001) and TNF-α (R = 0.32, p = 0.004). There was also a positive correlation between IFN-γ and TNF-α (R = 0.56, p < 0.001). Their levels may be interdependent, which may result from interconnectedness in the process of low-grade inflammation.
Discussion
Interleukin 6, TNF-α and IFN-γ play a significant role in the formation of atherosclerotic plaque, including in obese subjects [15, 16]. Atherosclerosis is the accumulation of macrophages, lipid-laden cells, mast cells, T cells and other degenerative material that occurs in the inner layer (tunica intima) of arterial walls. Then, Th1-activated macrophages release numerous pro-inflammatory cytokines that have a huge role in the development of atherosclerotic plaques. It turns out that increased release of cytokines, including TNF-α, IL-6 and IL-1, promotes expression of the proatherogenic gene [16]. An elevated blood IL-6 level has proven to be a better indicator of atherosclerotic plaque development than C-reactive protein (CRP) or low-density lipoprotein (LDL) levels [17, 18]. Interleukin 6 levels in healthy individuals can range from 0 pg/ml to 43.5 pg/ml [19]. In a study of 346 patients suffering from chest discomfort who had undergone coronary angiography it was found that IL-6 level was closely linked to the extent of coronary artery disease in acute coronary syndrome (ACS) patients [20]. Other cytokines such as IFN-γ and TNF-α have a very similar correlation with atherosclerosis. Liu et al. [21] stated that plasma levels of IL-6 and TNF-α can be used as monitoring indicators for intracranial and extracranial atherosclerosis. Intracranial atherosclerosis is significantly associated with an increase in the concentration of IL-6 and TNF-α in patients over 60 years old [21]. In the cited research no correlation was found between the level of TNF-α and atherosclerosis but there was a correlation between IFN-γ and atherosclerosis. The role of IFN-γ is well described in atherosclerotic plaque progression. Interferon γ enhances foam cell formation and lipid uptake and may activate macrophages [22]. Interferon γ is an important proatherogenic cytokine and is expressed in arterial plaques in patients with coronary atherosclerosis. The IFN-γ axis is activated independently of IL-6 or CRP [23].
The risk factors for an increase in the levels of IL-6, IFN-γ and TNF-α in the body are excessive body weight and, in particular, additional adipose tissue. Adipose tissue is endocrine active and, as a result of immunological processes, causes low-grade inflammation [24]. Both adipocytes and macrophages are important in low-grade inflammation because they work synergistically. An important role in this process is played by the inflammasome, consisting of intracellular sensor molecules, e.g. the pyrin domain from the NOD-like receptor family containing-3 (NLRP3). It is most likely activated by free fatty acids, reactive oxygen species, glucose, LPS and oxidized LDL cholesterol, causing the activation of caspase-1, which cleaves pro-IL-1β and pro-IL-18. Caspase-1 and these cytokines play a key role in insulin resistance and adipocyte differentiation. Leptin produced by SAT shows a linear relationship with adipose tissue. Leptin has pro-inflammatory effects via macrophages, T lymphocytes and other immune cells, stimulating the production of a broad spectrum of cytokines [25]. In the study group, the level of IL-6 increased with the amount of subcutaneous adipose tissue in the limbs. It is claimed that visceral adipose tissue is primarily responsible for the production of inflammatory markers present in low-grade inflammation [24]. Health problems associated with obesity are related more to the central (abdominal, visceral) distribution of fat rather than to its amount, and significant abdominal obesity increases the risk of metabolic and cardiovascular problems [26]. However, there are studies that support our results. Ramji et al. [27] found that excess body weight increases gene and protein expression of the IL-6R and IL-6 in human subcutaneous adipose tissue. The IL-6R protein expression was significantly intensified in the SAT from subjects with a BMI equal to or higher than 30 kg/m2 as compared to individuals with a lower BMI [27]. Adipose tissue macrophages are responsible for almost all TNF-α expression in adipose tissue and significant amounts of IL-6 expression. The accumulation of macrophages in subcutaneous adipocytes reaches its maximum when obesity is present. The SAT in lean mice contains 10% of the total number of macrophages and 50% in very obese mice. Among obese humans, adipose tissue is infiltrated by 40% of the total number of macrophages. This may be a direct cause of the increased concentration of IL-6 in correlation with SAT in humans with obesity [28].
Other factors that influence cytokine levels include diet and physical activity. In the latest umbrella review, 73 meta-analyses and 83 health outcomes from 8601 unique articles were analyzed. It was concluded that high sugar intake is generally most harmful for health, especially in cardiometabolic disease [29]. Also, eating large amounts of fructose in processed foods increases the risk of coronary heart disease due to obesity, insulin resistance, type 2 diabetes and increased triglyceride levels [30]. In addition, there is a relationship between the glycemic index of the diet and the risk of cardiovascular disease [31]. In the research, the consumption of large amounts of sweetened milk fruit drinks (high in glucose-fructose syrup – GF) promotes high levels of interleukin 6 in the serum, which indicates an increase of the presence of inflammation in the body [32]. Most publications confirm the adverse effects of sucrose and GF. The body weight of the subjects and the amount of calories in the diet have a significant impact on IL-6 levels. Intervention studies have often been performed with a eucaloric or hypercaloric diet, which may confound the outcome of the study [33–35]. Tumor necrosis factor in research shows a positive correlation with high intake of carbohydrates, in particular in conjunction with galactose and sucrose. A study showed that a low carbohydrate diet reduced TNF-α levels in 21 subjects after 25 weeks and it was as effective as treatment with a TNF-α inhibitor for 24 weeks in 21 subjects [36]. Similar results have been found in other studies [37]. A diet high in sweets has also been found to increase tumor necrosis factor levels [38]. In a research group of 1,128 people with a mean BMI of 29 kg/m2, it was found that higher consumption of sugary drinks could also be associated with an increase in the level of TNF-α in the blood [39]. In the study by Szczuko et al. [40], it was not the amount of carbohydrates but the glycemic index which was considered a factor favoring the increase in the level of TNF-α [40]. A low glycemic index anti-inflammatory diet might significantly reduce HbA1c, total cholesterol, cholesterol LDL, triglycerides, IL-6, and TNF-α levels after 6 months compared to the usual diet of the control group [41]. A diet rich in whole grains and products with a low glycemic index contributes to lowering the levels of TNF-α and IL-6. Although the underlying mechanisms remain unclear, some promising evidence suggests that short-chain fatty acids (SCFAs), which are produced in the intestines from fiber, may be a major contributing factor [42].
The IL-6 levels in our research were affected by alcohol consumption. The results may suggest that the more often the subjects consumed alcohol, the lower was the level of IL-6 in the serum. Studies by other authors are diametrically different. Ethanol has been proven to significantly increase the amount of IL-6 in the blood in an animal model [43, 44]. However, in a study where inflammation was achieved with lipopolysaccharide, acute intoxication with high doses of alcohol caused a decrease in the level of the above-mentioned interleukin 6 [45]. Ethanol reduced the amount of IL-6 in individuals in whom inflammation was already present [46, 47]. Crew et al. found that LPS-induced TNFα and IL-1β production was significantly reduced in monocytes obtained 16 hours after alcohol consumption compared to monocytes from the same subjects before alcohol consumption. This was associated with reduced nuclear translocation and DNA binding of nuclear regulatory factor-κB (NF-κB). NF-κB is induced by LPS and is a central regulator of proinflammatory cytokine gene activation, including TNF-α, IL-1, and IL-6. It can be concluded that acute alcohol consumption reduces the production of pro-inflammatory cytokines by inhibiting NF-κB-mediated intracellular pathways [48].
Interleukin 6 has a positive correlation with the occurrence of physical activity in the subjects. People who report doing physical exercises have a higher level of it. Studies by other authors have shown that the level of IL-6 is affected by the intensity and time spent on physical activity. The more intense physical effort or the longer the duration of an activity, the higher is the level of this cytokine. According to Ostrowski et al., this is not related to muscle damage during exercise. Rather this cytokine is produced locally in the muscles of the exercising person and it is muscle contraction that causes its increase in the serum [49]. This is also confirmed by other studies [50–52]. Interleukin 6 pending exercise acts as an energy sensor by triggering AMP-activated protein kinase and improving glucose usage and control mechanisms such as lipolysis and gluconeogenesis in adipose tissue and the liver [53]. Zhang et al. found that participation in physical activity of more than 150 minutes per week was associated with a lower 10-year cardiovascular disease (CVD) risk in overweight and obese adults [54]. This makes it possible to reduce the risk of heart disease through lifestyle modification and possible supplementation [55].
Limitations
This study concerns the significant problem of obesity. However, one should not forget about the limitations, such as the relatively small study group and the lack of a control group. We additionally consider atherosclerosis as a slowly developing pathological condition, which is difficult to diagnose in its early stages, so we decided to group participants based on their medical records and assign individuals to the atherosclerosis group if they had ever been diagnosed with the I70 identification code according to ICD10 (International Statistical Classification of Diseases and Related Health Problems). Respondents could have subjectively completed the original questionnaire, food diary and frequency of consumption of products in the FFQ-6 survey. The assessment of physical activity depends on the respondent. Norms were not imposed due to significant obesity, which makes it impossible to perform exercises at the same level as in the case of people with a normal body weight.
This study, however, provides some direction for future research, as it reveals the possible mechanisms linking low-grade inflammation to dietary components. This is all the more important due to the possibility of planning an effective dietary or pharmacological intervention limiting the occurrence of disease entities that occur in obesity as a result of low-grade inflammation.
Conclusions
The frequency of obesity and cardiovascular diseases is a growing problem. Obesity is associated with continual low-grade inflammation and a rise in the levels of inflammatory markers implicated in the development of many diseases. Future research will explore the correlation of other inflammatory markers with dietary patterns, food groups and nutrients to prevent obesity-related diseases such as cardiovascular diseases and many others. In our own research, excessive adipose tissue was found to be associated with higher levels of IL-6 and IFN-γ, which are also correlated with atherosclerosis. Limiting sugars, galactose and sucrose in the diet and reducing the frequency of consumption of sweet flavored dairy products may reduce the risk of heart disease. The introduction of physical activity can also be an effective anti-inflammatory intervention.