Purpose
Esophageal carcinoma (EC) is a common malignant tumor in China, and has the third highest incidence rate and second highest mortality rate among all tumors [1]. Majority of patients visit a hospital because of severe esophageal obstruction, of which only 15-20% can undergo radical surgical treatment [2]. Patients with advanced EC cannot tolerate traditional treatments, such as irradiation and chemoradiotherapy, because of their weakness; however, some elderly patients from underdeveloped areas of China have very low Karnofsky scores of less than 50, and the first goal of treatment for these patients is to improve their nutritional state as quickly as possible.
Iodine-125 (125I) brachytherapy (BT) has become an important part of the comprehensive treatment of malignant tumors, such as prostate cancer, lung cancer, liver cancer, and bone metastases, because it involves low-dose continuous irradiation, satisfactory local effects, and strong repeatability [3-6]. Animal studies confirmed that 125I BT can significantly inhibit squamous cell carcinoma [7]. Theoretically, 125I BT is sensitive to esophageal squamous cell carcinoma. Some scholars have combined covered esophageal stent with 125I seed to form a brachytherapy stent, which was then implanted into malignant esophageal obstruction segment to reduce the obstruction and perform brachytherapy. Results showed that quality of life (QoL) of patients and overall survival (OS) improved significantly [8]. However, palliative esophageal stenting is not suitable for some patients, including those with high cervical EC, dyspnea caused by tumor compression, and those who refuse esophageal stenting. For such patients, nasal feeding nutritional tubes (NFNTs) are the simplest and most effective alternative strategy. Can nutrition tubes be loaded with radioactive 125I seeds and placed across malignant EC areas to improve nutrition and perform intra-luminal brachytherapy (ILBT) simultaneously? In this pilot study, 125I seeds were regularly placed on a sticky medical device, and then attached to NFNT to form a brachytherapy nutritional tube (BNT), which was used to treat elderly EC patients.
Material and methods
General information
With the approval of ethics committee of our hospital (ethical number: 2017-KY-441), 26 esophageal carcinoma elderly patients with a 3/4 dysphagia score underwent NFNT-loaded 125I BT for ILBT simultaneously. Inclusion criteria were: 1) Age from 65 to 85 years, 2) Esophageal carcinoma confirmed by a pathological examination, 3) Clinical symptoms including a 3/4 dysphagia score, 4) Inability or unwillingness to undergo surgical resection or traditional chemoradiotherapy, 5) Karnofsky score ≥ 40 and ≤ 80, 6) Maximum diameter of the tumor ≤ 5.0 cm. Exclusion criteria were: 1) A benign esophagus tumor, 2) A platelet count < 30 × 109/l and prothrombin time > 25 sec, 3) A New York Heart Association class III or IV.
Pre-procedure investigations
All patients underwent routine blood examinations, including liver, kidney, electrolyte level, heart function tests, coagulation function tests, and electrocardiograms. Karnofsky and QoL scores (SF-36, Boston, USA) were applied to assess patient’s physical and physiological functions. An enhanced thoracic CT scan was performed within 1 week before the interventional procedure.
Equipment and apparatus
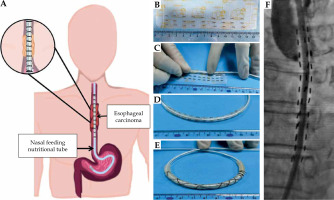
Regarding the production of BNT (Figure 1), three-column 125I seeds were regularly placed on a sticky medical device with a 5 mm interval distance, which was adhered to NFNT. The position was consistent with the occlusion according to pre-operative CT and esophagography results; 125I seeds exceeded the tumor length by 2 cm above and below the tumor. Finally, No. 7 non-absorbable nylon wire was used to fix 125I seeds to prevent displacement. Every 125I radioactive seed (Tianjin Saide Biopharmaceutical Co., Ltd., China) was 4.5 mm × 0.8 mm, with an average energy of 27-35 keV, half-life of 59.6 days, tissue penetration capacity of 1.7 cm, and single seed radioactivity of 0.8 mCi. Fluoroscopy was performed with a flat-panel detector and digital subtraction angiography (Artis Zeego, Siemens, Germany).
Fig. 1
Schematic diagram of the production and implantation process of brachytherapy nutritional tubes (BNTs) for the treatment of esophageal carcinoma. A) Diagrammatic sketch of BNT for esophageal carcinoma. B-E) The production process of BNT: three-column 125I seeds regularly placed on a sticky medical device with a 5 mm interval distance, which adhered to the nasogastric feeding tube. F) 125I seeds evenly distributed on the outside of NFNT under fluoroscopy
Procedure
CT scan image (thickness of 5 mm) was transmitted to treatment planning system (TPS) (Beijing University of Aeronautics and Astronautics, China) for target area delineation, prescription dose definition (60 Gy in this pilot study), and setting of dose limits for organs at risk. Gross tumor volume (GTV) referred to visible tumor area on imaging. Dosage requirements were D90 ≥ prescription dosage, V100 > 95%, and V150 < 100%.
Patient was placed in a supine position on a digital subtraction angiography operation table, and monitored by oxygen and electrocardiography equipment. Patient was anesthetized with a 2% lidocaine in the nasal cavity and oral mucosa. With a 0.035 inch soft guidewire (Cook, USA), a 5-F vertebral artery catheter (Cordis, USA) was introduced through esophageal occlusion segment, and the length of obstruction was measured with trans-catheter angiography. Then, the 0.035 inch soft guidewire was exchanged with a reinforced guidewire (length, 180 cm; Terumo, Japan). Along with the reinforced guidewire, BNT was advanced to the occluded area. The head end of nutrient tube was located in the stomach cavity. An 8 mm diameter balloon was used to expand the occluded segment, if necessary. BNT completely covered the upper and lower occluded areas by less than 2 cm, and BNT was placed within the body for 6 weeks.
Definition and follow-up
The successful placement of BNT into the area of malignant esophageal carcinoma was defined as technical success. Clinical success was defined as the successful removal of BNT and a dysphagia score ≤ 2. Dysphagia scores were interpreted as follows: score 0 – ability to maintain a normal diet, score 1 – ability to swallow some solid food, score 2 – ability to swallow semisolids only, score 3 – ability to swallow liquids only, score 4 – complete dysphagia. Dysphagia-free time (DFT) was defined as the time span from the removal of NFNT to the recurrence of a dysphagia score ≥ 3. Karnofsky, dysphagia, and QoL scores were evaluated 6 weeks after the procedure. CT data obtained within post-operative 3 days were uploaded to TPS for dose verification. The prescription dose was 60 Gy, and the spinal cord was considered an organ at risk (OAR). A SPECT (NM/CT 670, GE company, USA) scan was performed to evaluate γ-ray radiation distribution in EC zone. A health-related short form-36 (SF-36) questionnaire was used to assess eight domains, including physical functioning (PF), physical role (RP), bodily pain (BP), general health (GH), vitality, social functioning (SF), emotional role (RE), and mental health (M). All domains were scored on a scale of 0 to 100. All patients were followed up after BNT placement and underwent systemic treatments after ILBT. Dysphagia score and OS were determined by a telephone every 2 months. The last follow-up was performed in December 2020.
Statistical methods
Continuous data were expressed as mean ± standard deviation, range, or median value. SF-36 and Karnofsky scores were compared with Pearson’s χ2 test; the tumor diameter was compared using paired t-test, and TFS and OS were calculated using Kaplan-Meier method (SPSS v. 17.0 software, USA). P-value < 0.05 was considered statistically significant.
Results
The technical success rate was 100%. Five (19.2%) patients needed small balloon-assisted dilatation (diameter, 8 mm). Twenty patients underwent BNT removal and had a dysphagia score of less than 2, leading to a clinical success (76.9%, 20/26). The remaining 6 patients (4 and 2 with dysphagia scores of 4 and 3, respectively) were defined as technical failure. Five patients immediately underwent esophageal stenting (stent size, 18 mm × 120 mm; Taewoong, Korea), and one patient underwent conventional nutrition tube placement instead of BNT to resolve nutrition problems. Among the 20 patients with technical success, four patients underwent esophageal stenting at 2.3, 3.6, 5.2, and 6.2 months due to dysphagia recurrence after BNT removal. The mean durations required to place BNT and perform interventional procedure were 4.2 ±1.3 min (range, 3.3-6.5 min) and 20.9 ±4.3 min (range, 14.5-33.2 min), respectively. The mean D90 and OAR doses were 39.7 ±7.2 Gy (range, 28.5-55.3 Gy) and 2.3 Gy (range, 1.5-3.4 Gy), respectively (Table 1). Eight patients (30.8%) complained of intermittent postero-sternal pain during ILBT, and one of these patients experienced mild hematemesis (< 10 ml), which resolved after symptomatic treatment without major complications, such as seed loss, fistulas, or massive bleeding. The maximum transverse tumor diameter and dysphagia score significantly decreased from 3.1 ±0.6 cm and 3.8 ±0.4 to 1.9 ±0.3 cm and 1.8 ±1.2, respectively (p < 0.05) (Figures 2, 3). The mean Karnofsky score significantly increased from 58.4 ±9.4 to 77.2 ±7.4 (p < 0.05). The mean DFT was 3.1 ±1.2 months after BNT removal in 20 cases. SF-36 scores are listed in Table 2. The QoL assessments at 6 weeks showed significant improvements compared with pre-treatment data of PF, RF, GH, vitality, and RE scores (p < 0.05), while BP (p = 0.54), SF (p = 0.10), and MH scores (p = 0.07) showed no significant improvements.
Fig. 2
A 76-year-old male patient with cervical esophageal carcinoma (Karnofsky score, 50; dysphagia score, 4). A) Esophagography showed local esophageal complete occlusion (arrow). B) A small balloon (arrow; diameter, 8 mm) was used to dilate the occluded esophageal segment. C) Brachytherapy nutritional tube was placed across the tumor area, and post-operative SPECT (arrow) showed no seed migration and loss. D) Esophagography after 6 weeks showed that the contrast medium passed smoothly. E, F) Pre-operative CT showed that the esophageal wall had significantly thickened (diameter, 3.82 cm). G, H) Six weeks after the operation, the local tumor had significantly decreased according to CT (arrow)
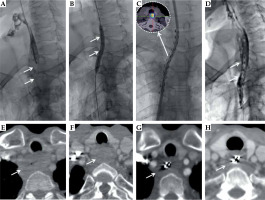
Fig. 3
An 82-year-old female patient with cervical esophageal carcinoma (Karnofsky score, 50; dysphagia score 4) underwent tracheal stenting because of difficulty in breathing after systemic chemotherapy failure. A) Pre-operative CT showed that the esophageal wall had significantly thickened (arrow; diameter, 2.8 cm). B) The post-operation SPECT showed the γ-ray covered the tumor satisfactorily. C) Six weeks after the operation, the local tumor had significantly decreased according to CT (arrow). D) Esophagography showed local esophageal complete occlusion (arrow). E, F) Brachytherapy nutritional tube was placed across the tumor area (E), and post-operative SPECT (F) showed no seed migration or loss. G) Esophagography after 6 weeks showed that the contrast medium passed smoothly
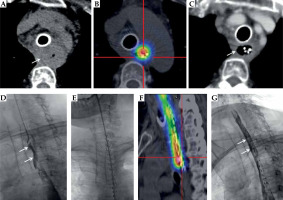
Table 1
Patient characteristics
Table 2
Pre- and post-treatment changes
During a median follow-up period of 8.3 months (range, 2.6-15.8 months), 19 patients (73.1%) underwent additional systemic chemotherapy (n = 12), oral anti-angiogenic agent (apatinib mesylate tablets) combined with PD-1 treatments (n = 5), and external irradiation (n = 2). Some patients (n = 7) did not undergo additional treatments due to various personal reasons. The mean DFT was 3.1 ±1.2 months. Four patients died, of whom two died due to multiple organ failure, one died of pulmonary infection due to local tumor progression, and one died of sudden massive hematemesis; the remaining 22 patients survived. The median overall survival time was 13.7 months (95% CI: 11.8-15.5).
Discussion
Dysphagia is the most common clinical symptom in patients with advanced EC, which severely affects their nutritional status and QoL, but more than 30% of patients, especially elderly patients, cannot tolerate surgery or concurrent chemoradiotherapy due to a poor health status [9]. Nutritional support is very important for elderly patients with EC and low Karnofsky scores, as nutritional support not only improves QoL but also is a form of continued anti-tumor treatment. Patients with Karnofsky scores above 70 can better tolerate conventional anti-tumor treatments [10]. External beam radiation therapy (EBRT) can help relieve dysphagia in long-term; however, there is a long period of time from the beginning of treatment to the remission of symptoms [11]. Moreover, due to uneven regional economic development, some county hospitals in China lack EBRT equipment. Esophageal stents are the first choice in non-surgical palliative care for patients with EC and 3/4 dysphagia scores, as these stents can quickly resolve obstructions. However, stenting may not be the best choice for patient with advanced cervical esophageal cancer because of foreign body sensation, for patients with cardiac cancer due to the risk of stent migration, and for patients with severe tracheal compression caused by EC [12]. Moreover, stent-related granulation proliferation and dysfunction are common complications for long-term stent placement.
Iodine-125 brachytherapy compared with EBRT, offers a fast reduction of intra-luminal portion of the tumor, thus rapidly restoring swallowing function and delivering a very low-dose of the agent to surrounding normal tissues, such as the lung, spinal cord, and adjacent normal esophageal mucosa. Moreover, 125I brachytherapy can be completed at home, and reducing social costs. Other scholars have applied ILBT using 125I strands to treat malignant biliary obstruction [13, 14] and vascular thrombus [15, 16], and showed that the local tumor response was better than that of single stenting, which was expected. Local 125I brachytherapy inhibits the proliferation of intra-luminal tumors to some extent, resulting in long-term stent patency. The present pilot study showed the technical success rate of 100% without major complications, and the dysphagia scores were also satisfactory comparing with those reported in previous studies on 125I brachytherapy stents, as shown in Table 3 [technical success rate, 91.5-100%; complication rate, 0-29.6%; dysphagia scores decreased from before (3.3-3.4) to after treatment (0.0-2.0)] [8, 17-24]. The results were not unexpected; this treatment takes advantage of not only the above- mentioned 125I bio-dosimetry, but also NFNT. Six cases (23.1%) with long areas of occlusion experienced clinical failure, possibly because the 125I seeds were arranged uniformly and linearly on the surface of BNT, while the tumor distribution at the esophageal lumen was uneven. In addition, the mean D90 of the six patients was only 29.3 Gy, which means that insufficient dosage and excessive tumor size are still the core reasons for poor local control effect. Further changes in the seed activity and number, or adding radiotherapy after physical recovery of elderly patients, are still a very important clinical topic, and we plan to examine this idea in the future.
Table 3
Recent studies on esophageal carcinoma brachytherapy using 125I seeds
| Author(s), year [Ref.] | Design | Sample size | Median age | Technical success | Complication | Dysphagia change | Overall survival | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Qin J, 2020 [17] | Rs | 153 (103 and 54 pts. in 18 mm and 20 mm stent groups) | 72.6 vs. 67.9 yrs. | 100% vs. 100% | Sp 15.4% in 18 mm vs. 32.7% in 20 mm stent groups | 2.02 in 18 mm stent vs. 2.0 in 20 mm stent | Median OS: 176 days in 18 mm vs. 109 days in 20 mm stent group | 18 mm stent showed a similar outcome of DR with 20 mm stent |
| Bi Y, 2020 [18] | Rs | 22 pts. | 72.2 yrs. | 100% | 27.3% incidence of stent migration | 3.4 vs. 0.5 after stenting | 9.9 months | Technical feasibility |
| Qin J, 2019 [19] | Rs | 201 pts. | 71.0 yrs. | 100% | Hemorrhage: 9%, Ap: 11.9%, fistula: 6.5% | 3.3 vs. 2.0 after treatment | Median OS: 153 days (95% CI: 128-181) | T-stage/tumor location/age were associated with DR |
| Zhao P, 2017 [20] | Rs | 43 pts. (18 in Is vs. 25 in Cs groups) | 70.4 yrs. | 100% vs. 100% | Sp/esophageal re-stenosis occurred in 16.7/11.1% and 16.0/12.0% in Is/Cs groups, respectively | Dysphagia scores decreased to 0-1 in all cases | 9.8 months in Is group and 4.8 in Cs group | Is group showed prolonged DR and OS |
| Tian D, 2016 [21] | Rs | 131 pts. (40/91 in Is/Cs groups, respectively) | 66.3/66.9 yrs. in Is and Cs groups | 100% vs. 100% | Massive hemorrhage/Sp/stent migration in 2.5/6.6%, 13.3/40%, 2.2/12.5%, respectively | Dysphagia score decreased in all cases | 4.4/4.2 months in Is and Cs groups, respectively | Is group showed improved OS and hospitalization costs |
| Liu N, 2014 [22] | Rs | 63 pts. (31/32 pts. in Is and Cs groups, respectively) | 65.0 yrs. | 93.5% vs. 93.8% | Sp/Gr/bleeding/fistula occurred 25.8/28.1%, 29.0/21.9%, 35.5/21.9%, 3.2/3.1% | Dysphagia score decreased in all cases | 4.0 vs. 3.0 months in Is and Cs groups, respectively | Is has potential benefit of longer DR but no significant on OS |
| Zhu HD, 2014 [23] | Ps | 160 pts. (80/80 in Is/Cs groups) | 71.0 yrs. | 91.5% vs. 93.8% | Sp/fistula/Ap/hemorrhage/recurrent dysphagia were 23/20%, 8/7%, 11/14%, 7/7%, 21/20% in Is/Cs groups | Dysphagia scores decreased from 3.3 to 1.4 in Is and from 3.4 to 1.4 in Cs group | 177 and 147 days in Is and Cs groups | Is had benefit on OS than in Cs group |
| Zhong- min W, 2012 [24] | Rs | 58 pts. (28/30 in Is/Cs groups) | 65.0/68.8 yrs. in Is/Cs groups | 100% vs. 100% | Sp/Gr/migration/re-stenosis were 53.6/80%, 7.1/10%, 3.6/6.7%, 3.6/6.7% in Is/Cs groups, respectively | Dysphagia scores decreased from 3.4 to 1.0 in Is and 3.4 to 1.0 in Cs groups | 11 and 4.9 months in Is and Cs groups | Implantation is technically feasible and effective |
| Guo JH, 2008 [8] | Ps | 53 (27/26 in Is/Cs groups) | 69.5/72.1 yrs. in Is/Cs groups, respectively | 100% vs. 100% | Sp/fistula/Ap/hemorrhage/stent migration/re-stenosis were 29.6/26.9%, 3.7/0.0%, 3.7/7.7%, 33.3/26.9%, 7.4%/11/5%, 29.6/23.1% in Is/Cs groups | Dysphagia scores decreased from 3.4 to 1.1 in Is and 3.4 to 1.2 in Cs group | 7 and 4 months in Is and Cs groups | Is implantation having potential benefit of longer DR and OS |
Regarding complications, 30.8% of patients complained of intermittent postero-sternal pain during ILBT, which could be related to tissue edema during 125I brachytherapy. No severe tumor bleeding or esophageal fistula occurred, indicating that the level of tissue tolerance was good. As the local tumor cumulative dose increased, the tumor shrank, the patients’ physical strength improved, and positive nitrogen level increased, which laid a foundation for further anti-tumor treatments. Although all the patients in this study were elderly patients with a mean age of 75.3 years, 73.1% of the patients underwent additional systemic anti-tumor therapy, which means that it could be an acceptable bridging therapy for advanced anti-cancer treatment, especially for patients with very low Karnofsky scores.
The present study paid more attention to QoL than nutrition status. The PF, RF, GH, vitality, and RE scores showed significant improvements after 125I brachytherapy, which could be caused by nutritional status improvements. The BP, SF and MH scores showed no significant improvements. The reason was that the BNT in the nose affected patients’ level of social participation and self-esteem, especially among the elderly patients, and mental health of these patients should be considered more carefully. SPECT was used to evaluate 125I seed displacement and loss. Although the cost is high, the dose coverage can be observed more directly with SPECT. Because the dose decreases by 80% within 2 cm of ILBT, this method needs to be combined with subsequent external radiotherapy for tumors with obvious wall thickening. Most of the cases in this study exhibited partial responses, suggesting that further improvement of local dose and radiosensitivity are still needed.
This study has several limitations. First, it was a retrospective study with a small sample size, no control group, and a limited observation period. In addition, the effects of follow-up treatments on the outcomes were not evaluated.
In summary, BNT for ILBT is technically a safe and effective strategy for elderly EC patients with low Karnofsky scores, and can be a bridging therapy for advanced anti-cancer treatment.



